Follicular lymphoma
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Follicular lymphoma | |
|---|---|
| Diagnosis in short | |
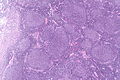
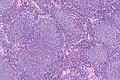
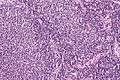
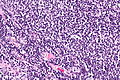
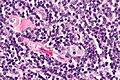
 Follicular lymphoma. H&E stain. | |
|
| |
| LM | Lymph node: abundant abnormally-shaped lymphoid follicles with some of the following: non-polarized mantle zone, non-polarized germinal center, loss of tingible body macrophages, sinuses effaced (lost) |
| LM DDx | diffuse large B-cell lymphoma, other small cell lymphomas, reactive follicular hyperplasia |
| IHC | CD20 +ve, CD10 +ve, BCL-6 +ve, BCL-2 +ve |
| Molecular | t(14;18)(q32;q21) / IGH-BCL2 |
| Gross | white lesions +/-subtle fine nodularity (fish flesh-like appearance) |
| Site | lymph node, spleen, bone marrow, others |
|
| |
| Prevalence | common |
| Prognosis | moderate to good |
| Clin. DDx | other causes of lymphadenopathy - other lymphomas, metastatic carcinoma |
Follicular lymphoma, abbreviated FL, is a very common non-Hodgkin lymphoma. It is a small cell lymphoma.
General
- A very common type of lymphoma.
- Moderate prognosis - overall five year survival ~ 66% in one cohort without transformation.[1]
- May transform to a more aggressive lymphoma, e.g. diffuse large B-cell lymphoma.
Gross
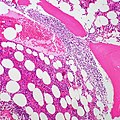
- Lymph node enlargement.
- Classically white and uniform - usually described as fish flesh-like.
- May have a vague nodularity.
Images
FL in the spleen. (WC)
Microscopic
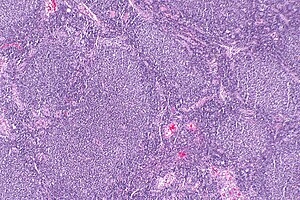
Features (lymph node):
- Abundant abnormally-shaped lymphoid follicles - key feature - including some of the following:
- Non-polarized mantle zone (normal mantle zone is usu. thicker at capsular aspect).
- Non-polarized germinal center (normal germinal center has dark & light area).
- Loss of tingible body macrophages.
- Sinuses effaced (lost).
Note:
- The intrafollicular component of the lymph node is compressed - follicles are often described as "kissing", as they nearly touch.
- In bone marrow specimens the neoplastic cells classically have a paratrabecular arrangement,[2] i.e. the lymphoma cells are found adjacent to the bone spicules.
DDx:
- Reactive follicular hyperplasia.
- Diffuse large B-cell lymphoma - esp. for the grade 3B.
Images
www:
Grading
- Grade 1-2: <= 22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective).
- Grade 3A: >22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective).
- Grade 3B: only centroblasts (within a nodular architecture).
Notes:
- Significant interobserver variability.[3]
- Grade 1 & Grade 2 lumped together.
- One should evaluate 10 HPFs.
- Only centroblasts without a nodular architecture is Diffuse large B cell lymphoma (DLBCL).
The usual cut points mentioned by people with HPFitis are:[4]
- Grade 1: 0-5 centroblasts / HPF.
- Grade 2: 5-15 centroblasts / HPF.
- Grade 3: >15 centroblasts / HPF.
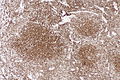
IHC
Features:[5]
- CD10 +ve.
- BCL6 +ve.
Others:
- CD5 -ve.
- +ve in mantle cell lymphoma.
- CD23 -ve/+ve.
- +ve in CLL.
- CD43 -ve.
- +ve in mantle cell lymphoma, marginal zone lymphoma.
- CD11c -ve -- flow cytometry only.
- CD21 -ve in tumour cells; highlights follicular dendritic cells.
- BCL2 +ve[5] - like many other small cell lymphomas.
- Usually negative in benign germinal centres.
A panel to work-up:
- BCL2, BCL6, CD3, CD5, CD10, CD20, CD23, cyclin D1.
Images
www:
Molecular
- t(14;18)(q32;q21)/IGH-BCL2 in 70-95% of cases.[5]
- Should not be confused with t(14;18)(q32;q21)/IGH-MALT1 seen in MALT lymphomas.[6]
Sign out
RETROPERITONEAL MASS, RIGHT, CORE BIOPSIES: - NON-HODGKIN B-CELL LYMPHOMA, FAVOUR FOLLICULAR LYMPHOMA. COMMENT: Morphology: -Small cells: size ~ mature lymphocytes, quantity - many, angular and round. -Large cells (intermixed with small cells): size ~1.5-2x mature lymphocyte, small nucleoli, moderate quantity of grey/basophilic cytoplasm, moderate nuclear pleomorphism. -Architecture: no gland formation, discohesive, no follicles apparent, no sheets of large cells. -Mitoses are uncommon. Immunohistochemical stains (tumour cells): Positive: CD45 (strong, membranous/cytoplasmic), CD20 (strong, membranous/cytoplasmic), BCL-2 (strong, membranous/cytoplasmic), CD10 (strong, membranous), BCL-6 (moderate, patchy, nuclear). Negative: pankeratin, CD3, CD5, CD30, CD21 (follicular dendritic cells not apparent), CD23 (scattered, rare). Ki-67: highlights the large cells, primarily -- 5-35% of cells within the core. The findings favour a follicular lymphoma, based on the cellular morphology and immunostains; however, they are limited by the type of tissue sampling (core biopsy). Clinical correlation is suggested.
See also
References
- ↑ 1.0 1.1 1.2 Link, BK.; Maurer, MJ.; Nowakowski, GS.; Ansell, SM.; Macon, WR.; Syrbu, SI.; Slager, SL.; Thompson, CA. et al. (Sep 2013). "Rates and outcomes of follicular lymphoma transformation in the immunochemotherapy era: a report from the University of Iowa/MayoClinic Specialized Program of Research Excellence Molecular Epidemiology Resource.". J Clin Oncol 31 (26): 3272-8. doi:10.1200/JCO.2012.48.3990. PMID 23897955.
- ↑ Iancu, D.; Hao, S.; Lin, P.; Anderson, SK.; Jorgensen, JL.; McLaughlin, P.; Medeiros, LJ. (Feb 2007). "Follicular lymphoma in staging bone marrow specimens: correlation of histologic findings with the results of flow cytometry immunophenotypic analysis.". Arch Pathol Lab Med 131 (2): 282-7. doi:10.1043/1543-2165(2007)131[282:FLISBM]2.0.CO;2. PMID 17284114.
- ↑ Good, D. 17 August 2010.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 813. ISBN 978-0781740517.
- ↑ 5.0 5.1 5.2 Vitolo U, Ferreri AJ, Montoto S (June 2008). "Follicular lymphomas". Crit. Rev. Oncol. Hematol. 66 (3): 248–61. doi:10.1016/j.critrevonc.2008.01.014. PMID 18359244.
- ↑ Bacon CM, Du MQ, Dogan A (April 2007). "Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists". J. Clin. Pathol. 60 (4): 361–72. doi:10.1136/jcp.2005.031146. PMC 2001121. PMID 16950858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001121/.