Difference between revisions of "Extramammary Paget disease"
Jump to navigation
Jump to search
(→DDx) |
(→IHC) |
||
| Line 91: | Line 91: | ||
==IHC== | ==IHC== | ||
*Extramammary Paget disease is a 'big' diagnosis in that the diagnosis will have significant clinical consequences. So a large panel of immuno is required to nail down the diangosis. | |||
*Is the lesion epithelial or melanocytic? (S100, Melan A) | |||
*Is the lesion adenocarcinoma or squamous cell carcinoma? | |||
**Low molecular weight (CK7, cam5.2) or high molecular weight keratins (34BE12, CK5/6)? | |||
**Adenocarcinoma markers? - CEA, BerEP4 | |||
**Nuclear differentiation markers? - p63 (squamous) vs GATA3 (adnexal) | |||
*Is the lesion primary or secondary | |||
**Secondary extramammary Paget disease may be CK20 positive (urothelial or rectal | |||
**If CK20 is positive are other organ specific markers positive? - CDX2 - colorectal or GATA3 - urothelial | |||
Panel: | Panel: | ||
*CEA | *A carcinoma marker - CEA or BerEP4 or both | ||
*Differential keratins - low molecular weight (glandular) cam5.2, CK7 vs high molecular weight (squamous) 34BE12, CK5/6<ref>RS. May 2010.</ref> | |||
*CK7 and CK20 - where does it come from? | |||
*S100 - | *S100 and Melan A - exclude melanoma in situ | ||
*Differentiation markers GATA - apocrine and urothelial; p63 - squamous, CDX2 - colorectal | |||
Notice that a CK20 negative urothelial origin EMPD will show the same immunoprofile as a primary cutaneous EMPD. | |||
Notice that you do not need to consider mammary Paget disease or Toker cells in your ddx. | |||
* | You can not rely on any one marker - a panel is required | ||
** | **Do not rely on CK7 alone as CK7 may be positive in pagetoid squamous cell carcinoma in situ or extramammary Paget disease <ref>{{Cite journal | last1 = Raju | first1 = RR. | last2 = Goldblum | first2 = JR. | last3 = Hart | first3 = WR. | title = Pagetoid squamous cell carcinoma in situ (pagetoid Bowen's disease) of the external genitalia. | journal = Int J Gynecol Pathol | volume = 22 | issue = 2 | pages = 127-35 | month = Apr | year = 2003 | doi = | PMID = 12649666 }}</ref> | ||
**p16 is not helpful in distinguishing between VIN and EMPD as may be positive in either. <ref>{{Cite journal | last1 = Sah | first1 = SP. | last2 = McCluggage | first2 = WG. | title = Florid vulval Paget disease exhibiting p16 immunoreactivity and mimicking classic VIN. | journal = Int J Gynecol Pathol | volume = 32 | issue = 2 | pages = 221-7 | month = Mar | year = 2013 | doi = 10.1097/PGP.0b013e31825909f6 | PMID = 23370646 }}</ref> | |||
==See also== | ==See also== | ||
Revision as of 11:12, 11 March 2015
| Extramammary Paget disease | |
|---|---|
| Diagnosis in short | |
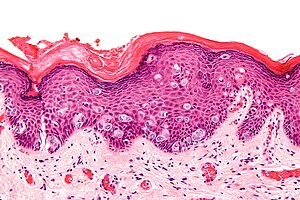 Extramammary Paget's disease. H&E stain. | |
|
| |
| LM | large epithelioid cells - nested or single - in the epidermis, clear/pale cytoplasm (occasionally eosinophilic), large nucleoli |
| LM DDx | benign Toker cell hyperplasia, malignant melanoma, Bowen's disease, apocrine carcinoma of the skin |
| IHC | CK7 +ve, CEA +ve, S-100 -ve, CK5/6 -ve, HER2 +ve |
| Gross | erythema, +/-weeping, +/-crusted |
| Site | vulva, penis, scrotum, others |
|
| |
| Symptoms | pruritis (itchy) |
| Prognosis | typically benign - usually not associated with an underlying malignancy (unlike Paget's disease of the breast) |
| Clin. DDx | contact dermatitis, lichen sclerosus |
Extramammary Paget disease, abbreviated EMPD, is a skin disease. As the name suggests, there is also a Paget disease of the breast.
There is also a Paget disease of the bone - just to make things confusing. This is dealt with in the bone article and has nothing (from a pathologic perspective) to do with the Paget disease discussed in this article
General
- Two types
- Primary Extramammary Paget disease - a malignancy of the cutaneous apocrine glands
- Arises in apocrine rich areas - usually the vulva but also the groin, inguinal area, perineum, penis[1] or scrotum.[2] and rarely axilla or eye.
- Usually entirely intraepidermal but may be associated with an underlying apocrine gland carcinoma (in contrast to mammary Paget disease which is usually associated with underlying mammary carcinoma).
- Secondary Extramammary Paget disease - intraepidermal spread from a distant tumor
- Usually of urothelial or colorectal origin.
- Arises in the perineal areas near these organs
- Primary Extramammary Paget disease - a malignancy of the cutaneous apocrine glands
Clinical:
- Pruritis.
- R/O VIN
- R/O vulvitis
Gross
Features:[2]
- Plaque with an irregular border.
- Erythematous or white.
Clinical DDx:
- Lichen sclerosus.[3]
- Vulvar intraepithelial neoplasia
- Vulvar squamous cell carcinoma in situ
- Other vulvitis
Images
Microscopic
Features:
- Epitheliod morphology (round/ovoid).
- Cells nested or single.
- Classically Paget cells ride above the basal cell layer
- But the process can fill the entire epidermis
- Clear/pale cytoplasm key feature - may also be eosinophilic.
- Large nucleoli.
Images
DDx
- Malignant melanoma in situ.
- Bowen disease - Pagetoid squamous cell carcinoma in situ.
- Pagetoid vulvar intraepithelial neoplasia
- Vulvar squamous cell carcinoma.
Stains
- Mucicarmine stain +ve.
IHC
- Extramammary Paget disease is a 'big' diagnosis in that the diagnosis will have significant clinical consequences. So a large panel of immuno is required to nail down the diangosis.
- Is the lesion epithelial or melanocytic? (S100, Melan A)
- Is the lesion adenocarcinoma or squamous cell carcinoma?
- Low molecular weight (CK7, cam5.2) or high molecular weight keratins (34BE12, CK5/6)?
- Adenocarcinoma markers? - CEA, BerEP4
- Nuclear differentiation markers? - p63 (squamous) vs GATA3 (adnexal)
- Is the lesion primary or secondary
- Secondary extramammary Paget disease may be CK20 positive (urothelial or rectal
- If CK20 is positive are other organ specific markers positive? - CDX2 - colorectal or GATA3 - urothelial
Panel:
- A carcinoma marker - CEA or BerEP4 or both
- Differential keratins - low molecular weight (glandular) cam5.2, CK7 vs high molecular weight (squamous) 34BE12, CK5/6[4]
- CK7 and CK20 - where does it come from?
- S100 and Melan A - exclude melanoma in situ
- Differentiation markers GATA - apocrine and urothelial; p63 - squamous, CDX2 - colorectal
Notice that a CK20 negative urothelial origin EMPD will show the same immunoprofile as a primary cutaneous EMPD. Notice that you do not need to consider mammary Paget disease or Toker cells in your ddx. You can not rely on any one marker - a panel is required
See also
References
- ↑ Ekwueme, KC.; Zakhour, HD.; Parr, NJ. (2009). "Extramammary Paget's disease of the penis: a case report and review of the literature.". J Med Case Reports 3: 4. doi:10.1186/1752-1947-3-4. PMID 19126202.
- ↑ 2.0 2.1 2.2 Guerra, R.; Misra, S. (2013). "Management of Extramammary Paget's Disease: A Case Report and Review of the Literature.". Case Rep Dermatol Med 2013: 436390. doi:10.1155/2013/436390. PMID 24349803.
- ↑ Bansal, D.; Bowman, CA. (Feb 2004). "Extramammary Paget's disease masquerading as lichen sclerosus.". Int J STD AIDS 15 (2): 141-2. doi:10.1258/095646204322764361. PMID 15006079.
- ↑ RS. May 2010.
- ↑ Raju, RR.; Goldblum, JR.; Hart, WR. (Apr 2003). "Pagetoid squamous cell carcinoma in situ (pagetoid Bowen's disease) of the external genitalia.". Int J Gynecol Pathol 22 (2): 127-35. PMID 12649666.
- ↑ Sah, SP.; McCluggage, WG. (Mar 2013). "Florid vulval Paget disease exhibiting p16 immunoreactivity and mimicking classic VIN.". Int J Gynecol Pathol 32 (2): 221-7. doi:10.1097/PGP.0b013e31825909f6. PMID 23370646.