Difference between revisions of "Complex endometrial hyperplasia"
Jump to navigation
Jump to search
| Line 26: | Line 26: | ||
| Prognosis = | | Prognosis = | ||
| Other = | | Other = | ||
| ClinDDx = [[dysfunctional uterine bleeding]] (diagnosis of exclusion), [[endometrial carcinoma]], [[inactive endometrium|atrophy]] | | ClinDDx = [[dysfunctional uterine bleeding]] (diagnosis of exclusion), [[endometrial carcinoma]], [[inactive endometrium|atrophy]], [[endometrial polyp]], others | ||
}} | }} | ||
{{ Infobox external links | {{ Infobox external links | ||
Revision as of 03:08, 20 December 2013
| Complex endometrial hyperplasia | |
|---|---|
| Diagnosis in short | |
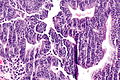
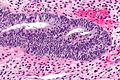
 Complex endometrial hyperplasia. H&E stain. | |
| Site | endometrium - see endometrial hyperplasia |
|
| |
| Associated Dx | obesity |
| Clinical history | usu. premenopausal or perimenopausal |
| Symptoms | abnormal uterine bleeding (AUB) |
| Prevalence | common |
| Clin. DDx | dysfunctional uterine bleeding (diagnosis of exclusion), endometrial carcinoma, atrophy, endometrial polyp, others |
| Complex endometrial hyperplasia | |
|---|---|
| External resources | |
| EHVSC | 10169 10181 (CEH with atypia) |
Complex endometrial hyperplasia, abbreviated CEH, is a relatively common pre-malignant pathology of the endometrium.
It is generally subdivided into complex endometrial hyperplasia without atypia and complex endometrial hyperplasia with atypia.
CEH with atypia is also known as complex atypical hyperplasia.
General
- Usually premenopausal or perimenopausal women.
- Associated with obesity.
- High risk of transformation to endometrial carcinoma especially when with atypia.
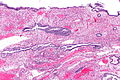
Microscopic
Features:
- Increase in size & number of glands + irregular shape - key feature.
- Cell stratification.
- Nuclear enlargement.
- Mitoses common.
- +/-Nuclear atypia:
- Round nuclei ~ 2-3x the size of a lymphocyte.
- Grey/translucent chromatin.
- Nucleoli.
Notes:
- Normal "gland-to-stroma ratio" is 1:3.
- Two "touching" glands may be one gland in section.
- Atypical nuclei often hide between non-typical nuclei, like peg cells in the fallopian tube.
DDx:
- Endometrioid endometrial carcinoma - see endometrial carcinoma versus complex endometrial hyperplasia.
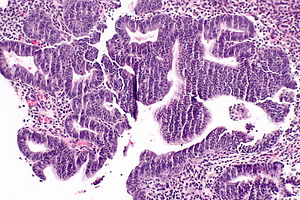
Endometrial carcinoma versus complex endometrial hyperplasia
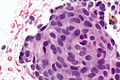
Complex endometrial hyperplasia:
- Non-confluent - glands distinct from one another.
Classic criteria for endometrial carcinoma
This is pimping material that shows up on exams.
Endometrial carcinoma has one of the following:[1][2][3]
- Desmoplastic stromal response.
- Confluent cribriform growth. †
- Extensive papillary growth. †
- Severe cytologic atypia. †
Note:
- † There is a size cut-off for criteria 2, 3 and 4: > 2.1 mm.[2]
How to remember ABCDE:
- Atypia Bad.
- Confluent cribriform growth.
- Desmoplasia.
- Extensive papillary growth.
Images
Complex endometrial hyperplasia:
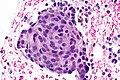
Squamous morules - commonly associated with hyperplasia and malignancy:
Fused glands suggestive of CEH in a polyp:
www:
- Endometrial hyperplasia (webpathology.com).
- Complex endometrial hyperplasia with atypia (webpathology.com).
Sign out
CEH without atypia
ENDOMETRIUM, BIOPSY: - COMPLEX ENDOMETRIAL HYPERPLASIA. -- NEGATIVE FOR CYTOLOGIC ATYPIA.
ENDOMETRIUM, BIOPSY: - SMALL FOCUS OF COMPLEX ENDOMETRIAL HYPERPLASIA WITHOUT ATYPIA, WITH SQUAMOUS MORULES. - ENDOMETRIAL POLYP WITH ONE ATYPICAL GLAND AND A SQUAMOUS MORULE. - SCANT ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY.
CEH with atypia
Insufficient confluence for carcinoma
ENDOMETRIUM, BIOPSY: - COMPLEX ENDOMETRIAL HYPERPLASIA WITH ATYPIA, SEE COMMENT. COMMENT: The sections show architecturally complex crowded glands with focal morular squamous metaplasia and focal cribriforming. Desmoplasia is not identified. The degree of gland confluence is not considered sufficient for the diagnosis of endometrial carcinoma. Nuclear atypia is present focally.
Insufficient extent for carcinoma
ENDOMETRIUM, BIOPSY: - COMPLEX ENDOMETRIAL HYPERPLASIA WITH ATYPIA, SEE COMMENT. COMMENT: The sections show architecturally complex back-to-back glands with focal morular squamous metaplasia and cribriforming. Desmoplasia is not present. The extent, i.e. the size of the abnormality, is not considered sufficient for the diagnosis of endometrial carcinoma.
See also
References
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 239. ISBN 978-0443069208.
- ↑ 2.0 2.1 Kurman, RJ.; Norris, HJ. (Jun 1982). "Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma.". Cancer 49 (12): 2547-59. PMID 7074572.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Endometrium_11protocol.pdf. Accessed on: 12 January 2012.