Helicobacter gastritis
Jump to navigation
Jump to search
Helicobacter gastritis, abbreviated HG, is a common form of gastritis caused by Helicobacter species.
| Helicobacter gastritis | |
|---|---|
| Diagnosis in short | |
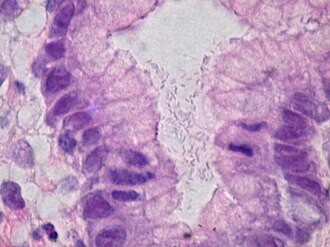 Helicobacter gastritis. H&E stain. | |
|
| |
| LM | helicobacter organisms, moderate chronic active gastritis (neutrophils esp. at the luminal aspect/intraepithelial, numerous plasma cell clusters) |
| Subtypes | Helicobacter pylori, Helicobacter heilmannii |
| LM DDx | chronic gastritis |
| Stains | Diff-Quik, Cresyl violet stain, Warthin-Starry stain |
| IHC | Helicobacter IHC |
| Site | stomach |
|
| |
| Associated Dx | MALT lymphoma, gastric carcinoma, intestinal metaplasia of the stomach, peptic ulcer, duodenitis |
| Prevalence | common |
| Endoscopy | erythema |
| Prognosis | benign |
| Clin. DDx | normal stomach |
The most common Helicobacter implicated is Helicobacter pylori, abbreviated HP.
General
- Several Helicobacter species can cause gastritis:
- Helicobacter pylori - most common.
- Helicobacter heilmannii.
Epidemiologic associations - Helicobacter infections are associated with:[1]
- Gastritis.
- Peptic ulcers.
- Cancer.
- Carcinoma.
- MALT lymphoma.
Gross
- Thickened gastric folds.
- Erythema.
Microscopic
Features:
- Helicobacter organisms - key feature.
- Inflammation - usually moderate chronic active.
- Clusters of (lamina propria) plasma cells.
- Neutrophils, numerous, classically intraepithelial.
Tips:
- One needs to look at 400x magnification. Even at 400x they are possible to miss.
- Helicobacter are damn small. They are smaller than the nucleus of the gastric foveollar cell.
- Look for mucus - they preferentially reside there.
- This is usually close to the opening of the gastric pits.
- Helicobacter are found in groups. When you see several that are the same size and shape you can be sure they are real.
Notes:
- Helicobacter can be in antrum and/or body.[4]
- Helicobacter don't like the intestinal mucosa or mucosa that has undergone intestinal metaplasia; you're less likely to find 'em adjacent to it. In general, Helicobacter is uncommon in the context of a case with IM... but common enough that one still ought to look for it.
- May be associated with G-cell hyperplasia.[5]
DDx:
- Dirt - material has a variable size.
- Contamination from oropharynx - bacilli straight, not associated with gastric mucosa.
- Chronic gastritis.
Images
www:
Stains
- Cresyl violet stain - background and organisms blue.
- Warthin-Starry stain - background yellow, organisms black.
IHC
- Helicobacter pylori IHC stain +ve.
Note:
- Reportly also stains Helicobacter heilmannii.[3]
Sign out
Body
STOMACH, BIOPSY: - BODY-TYPE MUCOSA WITH MODERATE CHRONIC ACTIVE GASTRITIS. - ABUNDANT HELICOBACTER-LIKE ORGANISMS PRESENT. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Antrum
STOMACH, BIOPSY: - ANTRAL-TYPE MUCOSA WITH MODERATE CHRONIC ACTIVE GASTRITIS. - ABUNDANT HELICOBACTER-LIKE ORGANISMS PRESENT. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show antral-type gastric mucosa with abundant lamina propria plasma cells and focal intraepithelial neutrophils. Cocci and bacilli are present. Some of the bacilli are Helicobactor-like. The epithelium matures normally to the surface. No goblet cells are identified.
See also
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 814. ISBN 0-7216-0187-1.
- ↑ Mobley, HLT.; Mendz, GL.; Hazell, SL.; Andersen, LP.; Wadström, T.. Basic Bacteriology and Culture. PMID 21290743. http://www.ncbi.nlm.nih.gov/books/NBK2444/.
- ↑ 3.0 3.1 Singhal, AV.; Sepulveda, AR. (Nov 2005). "Helicobacter heilmannii gastritis: a case study with review of literature.". Am J Surg Pathol 29 (11): 1537-9. PMID 16224223.
- ↑ Maaroos HI, Kekki M, Villako K, Sipponen P, Tamm A, Sadeniemi L (October 1990). "The occurrence and extent of Helicobacter pylori colonization and antral and body gastritis profiles in an Estonian population sample". Scand. J. Gastroenterol. 25 (10): 1010-7. PMID 2263873.
- ↑ Kwan, CP.; Tytgat, GN. (Nov 1995). "Antral G-cell hyperplasia: a vanishing disease?". Eur J Gastroenterol Hepatol 7 (11): 1099-1103. PMID 8680911.
- ↑ URL: http://gut.bmj.com/content/58/12/1669.extract. Accessed on: 2 March 2012.