Endocervical adenocarcinoma in situ
Endocervical adenocarcinoma in situ, also adenocarcinoma in situ of the uterine endocervix, is pre-invasive change of the uterine endocervix. It is closely tied to HPV infection.
| Endocervical adenocarcinoma in situ | |
|---|---|
| Diagnosis in short | |
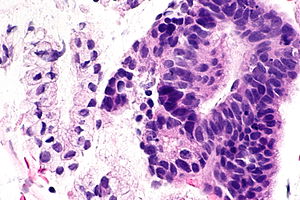 Endocervical adenocarcinoma in situ. H&E stain. | |
|
| |
| LM | Nuclear changes (nuclear crowding/pseudostratification, nuclear enlargement (often cigar-shaped nuclei), coarse chromatin, small nucleolus or nucleoli), +/-mitoses, +/-reduced cytoplasmic mucin, preservation of glandular architecture |
| LM DDx | tubal metaplasia, Arias-Stella reaction, endometriosis, lower uterine segment epithelium (esp. proliferative phase endometrium), endocervical adenocarcinoma, metastatic adenocarcinoma |
| IHC | p16 +ve |
| Site | uterine cervix - endocervical canal |
|
| |
| Associated Dx | squamous lesions (LSIL, HSIL) |
| Clinical history | +/-HPV |
| Symptoms | asymptomatic |
| Prevalence | uncommon |
| Clin. DDx | endocervical adenocarcinoma (invasive), endometrial carcinoma, squamous cervical lesions |
| Treatment | typically LEEP |
- For the cytology see Endocervical adenocarcinoma in situ (cytology)
If the context is clear, it may be referred to as adenocarcinoma in situ, abbreviated AIS.
General
- Usually due to HPV.
- May be found together with squamous neoplasias of the cervix.
- AIS of the cervix is much less common than squamous dysplasia of the cervix/SCC of the cervix.
- Generally, definitely diagnosed with an endocervical curettage (ECC).
Gross
- Not apparent at colposcopy.
Microscopic
Features:[1]
- Nuclear changes - key feature:
- Variable nuclear stratification.
- Nuclear crowding/pseudostratification.
- Nuclear enlargement.
- Often cigar-shaped nuclei.
- Coarse chromatin.
- Small nucleolus or nucleoli.
- Variable nuclear stratification.
- +/-Mitoses.
- +/-Reduced cytoplasmic mucin.
- Preservation of glandular architecture.
- Normal gland spacing - lack of complexity ("lobular pattern").
- Normal gland depth (subjective).
Ioffe, et al, :[2] devised a reproducible schema by which one might discern reactive glandular atypia, glandular dysplasia, and adenocarcinoma in situ, summarized in the table below from the article:
Sum the scores for stratification, nuclear atypia, and mitoses/apoptotic bodies
Stratification
None (0 points)
Mild (1 point)
Moderate (2 points)
Up to the luminal surface (3 points)
Nuclear atypia
As normal (0 points)
Small (size of normal) or slightly enlarged uniform nuclei, minimal hyperchromasia, little dispolarity, no nucleoli (1 point)
Nuclear enlargement (≤3× normal), moderate anisocytosis/hyperchromasia/dispolarity, occasional small nucleoli (2 points)
Large nuclei (>3× normal), marked anisocytosis, marked hyperchromasia, severe dispolarity, frequent prominent nucleoli (3 points)
Mitoses and apoptoses in two most active glands, number per gland (average between two glands)
None (0 points)
Less than 0.5 per gland (1 point)
0.6–3.0 per gland (2 points)
>3.0 per gland (3 points)
Total score 0–3 = benign 4–5 = endocervical glandular dysplasia (EGD) 6–9 = adenocarcinoma in situ
DDx:
- Tubal metaplasia.
- Arias-Stella reaction.
- Endometriosis.
- Lower uterine segment epithelium[3] - esp. proliferative phase endometrium - mitoses rare, NC ratio normal, stroma different.
- Endocervical adenocarcinoma - often has paradoxical maturation... paler cytoplasm & nuclei than adjacent AIS.
- Metastatic adenocarcinoma.
- Proliferative phase endometrium - endometrial type stroma, cytoplasm not pale staining, no nuclear atypia (smooth nuclear contour, stratified).
Images
Case - ECC
Case - biopsy
www
IHC
- p16 +ve.
- CEA +ve.
- Vimentin -ve.
Sign out
UTERINE CERVIX, BIOPSY: - HIGH-GRADE SQUAMOUS INTRAEPITHELIAL LESION (HSIL). - ENDOCERVICAL ADENOCARCINOMA IN SITU (AIS). - ACUTE AND CHRONIC INFLAMMATION. COMMENT: A p16 immunostain marks the full thickness of the squamous epithelium and is strong. A Ki-67 immunostain marks increased numbers of superficial squamous cells. The atypical endocervical epithelium (interpreted as AIS) is strongly p16 positive and has an increased proliferative activity with Ki-67 staining.
Micro
The atypical endocervical epithelium (interpreted as AIS) shows marked hyperchromasia, nuclear crowding and moderate nuclear atypia with a relatively abundant cytoplasm ( nucleus to cell size = 1:2 ).
See also
References
- ↑ Zaino, RJ. (Mar 2000). "Glandular lesions of the uterine cervix.". Mod Pathol 13 (3): 261-74. doi:10.1038/modpathol.3880047. PMID 10757337. http://www.nature.com/modpathol/journal/v13/n3/full/3880047a.html.
- ↑ Ioffe OB, Sagae S, Moritani S, Dahmoush L, Chen TT, Silverberg SG. (2003). "Proposal of a new scoring scheme for the diagnosis of noninvasive endocervical glandular lesions". Am J Surg Pathol 27 (4): 452–460. PMID 12657929.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 167. ISBN 978-0443069208.
- ↑ URL: http://www.womenshealthsection.com/content/print.php3?title=gynpc006&cat=60&lng=english. Accessed on: 20 March 2013.