Marginal zone lymphoma
Marginal zone lymphoma, abbreviated MZL, is a common type of lymphoma composed of small cells.
| Marginal zone lymphoma | |
|---|---|
| Diagnosis in short | |
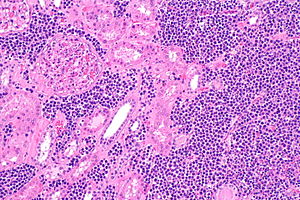 Marginal zone lymphoma of the kidney. H&E stain. | |
|
| |
| LM | small lymphoid cells +/-plasmacytoid features +/-lymphoepithelial lesion |
| LM DDx | other small cell lymphomas, DLBCL |
| IHC | CD20 +ve, BCL2 +ve, CD21 +ve, CD43 +ve/-ve |
| Site | gastrointestinal tract, lymph nodes |
|
| |
| Prevalence | moderate |
| Endoscopy | +/-nodularity |
| Other | CD11c +ve (flow cytometry or laser scanning cytometry) |
General
- Arise in the context chronic infections, e.g. Sjögren disease (salivary gland), Hashimoto thyroiditis (thyroid gland), Helicobacter pylori gastritis (stomach).[1]
Classification
- Comes in three different flavours:
- Extranodal marginal zone lymphoma.
- If in mucosa-associated lymphoid tissue known as a MALT lymphoma, AKA MALToma.
- Splenic marginal zone lymphoma (SMZL).
- Nodal marginal zone lymphoma (NMZL).
- Extranodal marginal zone lymphoma.
Microscopic
Features:
- Small (lymphoid) cells that may be plasma cell-like (plasmacytoid):[2]
- +/-Clockface nucleus.
- +/-Eccentric nucleus.
- +/-"Lymphoepithelial lesion" - gastric crypts invaded by a monomorphous population of lymphocytes.[3]
- Features:
- Cluster of lymphocytes - three cells or more - key feature.
- Single lymphocytes don't count.
- Clearing around the lymphocyte cluster.
- Cluster of lymphocytes - three cells or more - key feature.
- Not specific for MALT lymphoma, i.e. may be seen in other types of lymphoma.[4]
- Features:
DDx:
- Other small cell lymphomas.
- DLBCL - should be a distinctive region at low power.[citation needed]
Images
www:
Lymphoepithelial lesion
IHC
Features:[5]
- CD20 +ve.
- BCL2 +ve.
- CD21 +ve.
- CD11c +ve (flow cytometry or laser scanning cytometry - only; not available for paraffin).
- CD43 +ve/-ve.
- Typically positive in mantle cell lymphoma.
Others:
- CD5 -ve.
- CD10 -ve.
- CD23 -ve.
Molecular
There are several associated with MALT lymphoma:[6]
- t(11;18)(q21;q21) / API2‐MALT1[7] - most common translocation in MALT lymphoma.[8]
- t(14;18)(q32;q21) / IGH‐MALT1.
- Should not be confused with t(14;18) seen in follicular lymphoma between IGH-BCL2.[9]
- t(1;14)(p22;q32) / IGH‐BCL10.
The MALT1 associated translocations can be assessed with an ISH break apart probe for MALT1.
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 326. ISBN 978-1416054542.
- ↑ URL: http://surgpathcriteria.stanford.edu/bcell/marginalnodal/printable.html. Accessed on: 6 March 2012.
- ↑ Papadaki, L.; Wotherspoon, AC.; Isaacson, PG. (Nov 1992). "The lymphoepithelial lesion of gastric low-grade B-cell lymphoma of mucosa-associated lymphoid tissue (MALT): an ultrastructural study.". Histopathology 21 (5): 415-21. PMID 1452124.
- ↑ DB. 6 August 2010.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 95. ISBN 978-0443066450.
- ↑ Bacon CM, Du MQ, Dogan A (April 2007). "Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists". J. Clin. Pathol. 60 (4): 361–72. doi:10.1136/jcp.2005.031146. PMC 2001121. PMID 16950858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001121/.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 170. ISBN 978-1416054542.
- ↑ Streubel, B.; Lamprecht, A.; Dierlamm, J.; Cerroni, L.; Stolte, M.; Ott, G.; Raderer, M.; Chott, A. (Mar 2003). "T(14;18)(q32;q21) involving IGH and MALT1 is a frequent chromosomal aberration in MALT lymphoma.". Blood 101 (6): 2335-9. doi:10.1182/blood-2002-09-2963. PMID 12406890.
- ↑ Vitolo, U.; Ferreri, AJ.; Montoto, S. (Jun 2008). "Follicular lymphomas.". Crit Rev Oncol Hematol 66 (3): 248-61. doi:10.1016/j.critrevonc.2008.01.014. PMID 18359244.