Esophageal adenocarcinoma
Jump to navigation
Jump to search
Esophageal adenocarcinoma, also adenocarcinoma of the esophagus, is a common malignant epithelial-derived tumour of the distal esophagus, that classically arises in the context of Barrett's esophagus.
General
- Often a prognosis poor - as diagnosed in a late stage.
- May be difficult to distinguish from adenocarcinoma of the stomach.
- By convention (in the CAP checklist) gastroesophageal junction carcinomas are staged as esophageal carcinomas.[1]
Treatment
- Adenocarcinoma in situ (AIS) - may be treated with endoscopic mucosal resection & follow-up.[2]
- Surgery - esophagectomy.
Esophagus versus stomach
The convention is it's esophageal if both of the following are true:[3]
- Epicenter of tumour is in the esophagus.
- Barrett's mucosa is present.
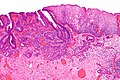
Microscopic
Features:
- Adenocarcinoma:
- Cell clusters that form glands.
- Nuclear atypia of malignancy:
- Size variation.
- Shape variation.
- Staining variation.
- Mitoses common.
DDx:
Images
Grading
Graded like other adenocarcinoma:[3]
- >95 % of tumour in glandular arrangement = well-differentiated.
- 95-50% of tumour in glandular arrangement= moderately-differentiated.
- <50% of tumour in glandular arrangment = poorly-differentiated.
Staging
Early esophageal adenocarcinoma has its own staging system:[4][5]
- M1 = lamina propria.
- M2 = superficial muscularis mucosae.
- M3 = submucosa.
- M4 = muscularis propria.
IHC
- CK7 +ve.
- CK20 +ve.
To rule-out SCC:
- p63 -ve.
- HWMK -ve.
Sign out
GASTROESOPHAGEAL JUNCTION, RESECTION: - INTRAMUCOSAL ADENOCARCINOMA, pT1a, pNx, SEE TUMOUR SUMMARY. -- MUCOSAL MARGIN HAS CAUTERIZED DYSPLASTIC EPITHELIUM, SEE COMMENT. -- DEEP MARGIN NEGATIVE FOR MALIGNANCY. COMMENT: The cauterized dysplastic epithelium cannot be further interpreted. Malignant-appearing glands are within 1 mm of the cauterized epithelium. Close follow-up and re-biopsy (or endoscopic re-resection if clinically indicated) is recommended. This case was partially reviewed internally. There is agreement on the presence of intramucosal adenocarcinoma and dysplastic epithelium at the mucosal margin.
See also
References
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Esophagus_11protocol.pdf. Accessed on: 6 April 2012.
- ↑ Sampliner, RE. (Jul 2009). "Endoscopic therapy for Barrett's esophagus.". Clin Gastroenterol Hepatol 7 (7): 716-20. doi:10.1016/j.cgh.2009.03.011. PMID 19306943.
- ↑ 3.0 3.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 168. ISBN 978-0781765275.
- ↑ Pech, O.; May, A.; Rabenstein, T.; Ell, C. (Nov 2007). "Endoscopic resection of early oesophageal cancer.". Gut 56 (11): 1625-34. doi:10.1136/gut.2006.112110. PMC 2095648. PMID 17938435. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2095648/.
- ↑ Thosani, N.; Singh, H.; Kapadia, A.; Ochi, N.; Lee, JH.; Ajani, J.; Swisher, SG.; Hofstetter, WL. et al. (Nov 2011). "Diagnostic accuracy of EUS in differentiating mucosal versus submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis.". Gastrointest Endosc. doi:10.1016/j.gie.2011.09.016. PMID 22115605.