Difference between revisions of "Rectal prolapse"
Jump to navigation
Jump to search
(split out) |
m (+infobox) |
||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Rectal_prolapse_-_intermed_mag.jpg | |||
| Width = | |||
| Caption = Fibromuscular hyperplasia as seen in rectal prolapse. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = fibromuscular hyperplasia: lamina propria fibrosis and muscle, thick muscularis propria, +/-ischemic changes | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[rectum]] | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = women - multiparous & postmenopausal | |||
| Signs = "rectal mass" | |||
| Symptoms = | |||
| Prevalence = not common | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = rectal carcinoma (rarely) | |||
| Tx = surgery | |||
}} | |||
'''Rectal prolapse''' is a benign pathology of the [[rectum]], typically seen in women that are multiparous and postmenopausal. | '''Rectal prolapse''' is a benign pathology of the [[rectum]], typically seen in women that are multiparous and postmenopausal. | ||
| Line 18: | Line 49: | ||
**Muscularis mucosae is "too superficial" (muscle in the lamina propria). | **Muscularis mucosae is "too superficial" (muscle in the lamina propria). | ||
*Surface ulceration + inflammation ([[neutrophil]]s). | *Surface ulceration + inflammation ([[neutrophil]]s). | ||
**May show frank ischemic changes - see ''[[ischemic colitis]]''. | |||
*+/-Serration of epithelium at the surface. | *+/-Serration of epithelium at the surface. | ||
| Line 41: | Line 73: | ||
==See also== | ==See also== | ||
*[[Rectum]]. | *[[Rectum]]. | ||
*[[Solitary rectal ulcer]]. | |||
==References== | ==References== | ||
Revision as of 17:16, 31 December 2013
| Rectal prolapse | |
|---|---|
| Diagnosis in short | |
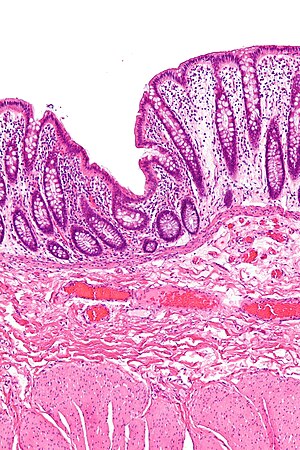 Fibromuscular hyperplasia as seen in rectal prolapse. H&E stain. | |
|
| |
| LM | fibromuscular hyperplasia: lamina propria fibrosis and muscle, thick muscularis propria, +/-ischemic changes |
| Site | rectum |
|
| |
| Clinical history | women - multiparous & postmenopausal |
| Signs | "rectal mass" |
| Prevalence | not common |
| Prognosis | benign |
| Clin. DDx | rectal carcinoma (rarely) |
| Treatment | surgery |
Rectal prolapse is a benign pathology of the rectum, typically seen in women that are multiparous and postmenopausal.
General
Epidemiology:
- ~90% women, postmenopausal and multiparous.[2]
Treatment:
- Surgical:
- Delorme procedure = mucosa stripped.
Microscopic
Features:[3]
- "Fibromuscular hyperplasia" - key feature:
- Fibrosis (submucosa, lamina propria).
- Muscularis mucosae is "too superficial" (muscle in the lamina propria).
- Surface ulceration + inflammation (neutrophils).
- May show frank ischemic changes - see ischemic colitis.
- +/-Serration of epithelium at the surface.
Notes:
- Important negative: no nuclear atypia.
Images
Sign out
RECTAL MUCOSA, DELORME PROCEDURE: - SUPERFICIAL RECTAL WALL WITH FIBROMUSCULAR HYPERPLASIA AND EDEMA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show rectal mucosa, submucosa and a small amount of muscularis propria. The mucosa shows fibromuscular hyperplasia with thickening of the muscularis mucosae and mild lamina propria fibrosis. The submucosa is edematous. The small amount of muscularis propria is unremarkable. The epithelium matures normally to the surface. No significant nuclear atypia is identified.
See also
References
- ↑ Brosens LA, Montgomery EA, Bhagavan BS, Offerhaus GJ, Giardiello FM (November 2009). "Mucosal prolapse syndrome presenting as rectal polyposis". J. Clin. Pathol. 62 (11): 1034–6. doi:10.1136/jcp.2009.067801. PMC 2853932. PMID 19861563. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2853932/.
- ↑ Lee, S.; Kye, BH.; Kim, HJ.; Cho, HM.; Kim, JG. (Feb 2012). "Delorme's Procedure for Complete Rectal Prolapse: Does It Still Have It's Own Role?". J Korean Soc Coloproctol 28 (1): 13-8. doi:10.3393/jksc.2012.28.1.13. PMID 22413077.
- ↑ Schneider A, Fritze C, Bosseckert H, Machnik G (1988). "[Primary clinical, endoscopic and histologic findings in solitary rectal ulcer]" (in German). Dtsch Z Verdau Stoffwechselkr 48 (3-4): 183–9. PMID 3234303.

