Difference between revisions of "Intramucosal colorectal carcinoma"
Jump to navigation
Jump to search
| Line 18: | Line 18: | ||
*[[Intramucosal carcinoma]]. | *[[Intramucosal carcinoma]]. | ||
*[[Colorectal cancer staging]]. | *[[Colorectal cancer staging]]. | ||
*[[Pseudoinvasion]]. | |||
==References== | ==References== | ||
Latest revision as of 06:29, 19 March 2018
Intramucosal colorectal carcinoma is a confusing term for high grade (colorectal) dysplasia that should be avoided.[1]
Intramucosal rectal carcinoma, intramucosal colonic carcinoma, intramucosal colonic adenocarcinoma, intramucosal rectal adenocarcinoma, intramucosal adenocarcinoma of the colon, and colorectal adenocarcinoma in situ redirect here.
Background
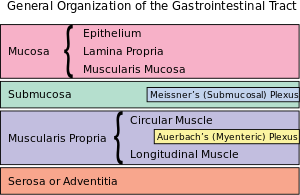
- Colorectal adenocarcinoma is defined by invasion into the submucosa.
- This is different than elsewhere in the GI tract, where cancer is defined by invasion through the basement membrane, i.e. into the lamina propria.
- Rationale: atypical (cancer-like) cells in lamina propria do not have metastatic potential as there are no lymphatics in the colorectal lamina propria.[2]
Note:
- If one wants to differentiate adenocarcinoma in situ and high-grade dysplasia:
- Adenocarcinoma in situ has invasion into the lamina propria and high-grade dysplasia does not have lamina propria invasion. Thus, the difference amounts to seeing a desmoplastic stroma or infiltrative cells; if one of these is present it is adenocarcinoma in situ, if both are not it is dysplasia.
See also
- Colorectal adenocarcinoma.
- Traditional adenoma.
- Intramucosal carcinoma.
- Colorectal cancer staging.
- Pseudoinvasion.
References
- ↑ Fleming, M.; Ravula, S.; Tatishchev, SF.; Wang, HL. (Sep 2012). "Colorectal carcinoma: Pathologic aspects.". J Gastrointest Oncol 3 (3): 153-73. doi:10.3978/j.issn.2078-6891.2012.030. PMID 22943008.
- ↑ Lewin, MR.; Fenton, H.; Burkart, AL.; Sheridan, T.; Abu-Alfa, AK.; Montgomery, EA. (Dec 2007). "Poorly differentiated colorectal carcinoma with invasion restricted to lamina propria (intramucosal carcinoma): a follow-up study of 15 cases.". Am J Surg Pathol 31 (12): 1882-6. doi:10.1097/PAS.0b013e318057fac2. PMID 18043043.