Difference between revisions of "Leukemia"
Jensflorian (talk | contribs) (→Leukemia classification: Latest progn) |
m (further tidy) |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
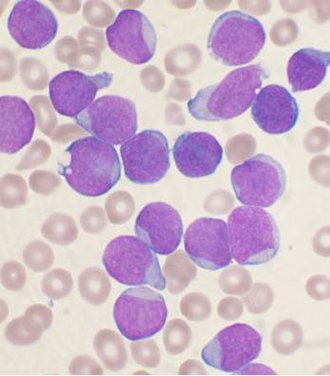
[[Image:Acute leukemia-ALL.jpg | thumb|right|A bone marrow of an individual with precursor B-cell lymphoblastic leukemia. [[Wright stain]]. (WC)]] | [[Image:Acute leukemia-ALL.jpg | thumb|right|A bone marrow of an individual with precursor B-cell lymphoblastic leukemia. [[Wright stain]]. (WC)]] | ||
The | The term '''leukemia''' is broadly used to refer to any haematological malignancy where the neoplastic cells in the circulation are the prominent feature. It is generally only seen by anatomical pathologists only in countries where hematopathology reporting is done by anatomical pathologists rather than hematologists. | ||
Lymphoma is discussed in the ''[[lymphoma]]'' article, and overlaps somewhat with leukemia as the clear distinction between the two is historical | Lymphoma is discussed in the ''[[lymphoma]]'' article, and overlaps somewhat with leukemia as the clear distinction between the two is somewhat arbitrary and historical:<ref>{{Ref PCPBoD8|314}}</ref> | ||
*Leukemia = involves bone marrow +/- peripheral blood. | *Leukemia = involves bone marrow +/- peripheral blood. | ||
**Classic presentation: infection, bleeding, anemia. | **Classic presentation: infection, bleeding, anemia. | ||
*Lymphoma = discrete mass(es), usu. [[lymph node]]. | *Lymphoma = discrete mass(es), usu. [[lymph node]]. | ||
**Classic presentation: non-tender lymph nodes | **Classic presentation: non-tender lymph nodes | ||
Leukemias may present as discrete massess, e.g. in the skin ([[leukemia cutis]]) or at other sites, where it is known by various names ([[myeloid sarcoma]], chloroma, etc.). | |||
Most leukemias are typically classified into acute or chronic. As a general rule, the designation of '''acute''' signifies a more immature and aggressive phenotype, whilst '''[[chronic]]''' leukemias generally show a more differentiated phenotype and run a more indolent course. There are exceptions, of course, and some chronic leukemias may transform into acute lymphomas. | |||
=Definition= | =Definition= | ||
This varies with the type. | |||
For acute myeloid leukemia, all of the following:<ref name=dg21mar20011>D. Good. 21 March 2011.</ref> | |||
#Morphologic abnormalities. | #Morphologic abnormalities. | ||
#>20% blasts ''or'' recurrent cytogenetic abnormality. | #>20% blasts ''or'' recurrent cytogenetic abnormality. | ||
=Leukemia classification= | |||
*[[Acute myeloid leukemia]] (AML). In this context, myeloid is used broadly to refer to non-lymphoid precursors rather than the more limited meaning granulopoietic: | |||
*#AML. | |||
*#AML with recurrent cytogenetic abnormalities, e.g. t(8;21), inv(16) and t(15;17). | |||
*#AML arising from [[MDS]]. | |||
*#AML in the setting of [[Down syndrome]]. | |||
*[[Acute lymphoblastic leukemia]] (ALL): | |||
*#B cell. | |||
*#B cell with recurrent cytogenetic abnormalities. | |||
*#T cell (sometimes abbreviated to T-ALL) | |||
*T-ALL should not to be confused with [[adult T-cell leukemia/lymphoma]] (ATLL) - this is associated with HTLV-1 infection | |||
*[[Chronic lymphocytic leukemia]] (CLL) - usually classified with lymphomas | |||
A few fall under the umbrella of '''[[myeloproliferative neoplasm]]s''': | |||
*[[Chronic myeloid leukemia]] (CML) | |||
*[[Chronic neutrophilic leukemia]] (rare) | |||
*[[Chronic eosinophilic leukemia]] (rare) | |||
And others under the myeloproliferative/myelodysplastic overlap syndromes: | |||
*[[Chronic myelomonocytic leukemia]] | |||
Other less common leukemias: | |||
*Hairy cell leukemia | |||
*T-cell prolymphocytic leukemia | |||
*T-cell large granular lymphocyte leukaemia (T-LGL) | |||
*Plasma cell leukaemia | |||
*Mast cell leukemia | |||
=Histomorphologic overview= | =Histomorphologic overview= | ||
| Line 38: | Line 68: | ||
|} | |} | ||
† should be easy to remember as smALL people, i.e. kids, get this type of acute leukemia. | † should be easy to remember as smALL people, i.e. kids, get this type of acute leukemia. | ||
=Algorithms= | =Algorithms= | ||
| Line 48: | Line 77: | ||
*Chemotherapy? | *Chemotherapy? | ||
*[[Down syndrome]]? | *[[Down syndrome]]? | ||
=Prognosis= | =Prognosis= | ||
| Line 68: | Line 83: | ||
#lymphoid leukaemia: 52.4% (Colombia) to 91.6% (Germany) | #lymphoid leukaemia: 52.4% (Colombia) to 91.6% (Germany) | ||
#acute myleoid leukemia: 33.3% (Bulgaria) to 78.2% (Germany) | #acute myleoid leukemia: 33.3% (Bulgaria) to 78.2% (Germany) | ||
=See also= | =See also= | ||
Latest revision as of 20:06, 26 May 2018
The term leukemia is broadly used to refer to any haematological malignancy where the neoplastic cells in the circulation are the prominent feature. It is generally only seen by anatomical pathologists only in countries where hematopathology reporting is done by anatomical pathologists rather than hematologists.
Lymphoma is discussed in the lymphoma article, and overlaps somewhat with leukemia as the clear distinction between the two is somewhat arbitrary and historical:[1]
- Leukemia = involves bone marrow +/- peripheral blood.
- Classic presentation: infection, bleeding, anemia.
- Lymphoma = discrete mass(es), usu. lymph node.
- Classic presentation: non-tender lymph nodes
Leukemias may present as discrete massess, e.g. in the skin (leukemia cutis) or at other sites, where it is known by various names (myeloid sarcoma, chloroma, etc.).
Most leukemias are typically classified into acute or chronic. As a general rule, the designation of acute signifies a more immature and aggressive phenotype, whilst chronic leukemias generally show a more differentiated phenotype and run a more indolent course. There are exceptions, of course, and some chronic leukemias may transform into acute lymphomas.
Definition
This varies with the type.
For acute myeloid leukemia, all of the following:[2]
- Morphologic abnormalities.
- >20% blasts or recurrent cytogenetic abnormality.
Leukemia classification
- Acute myeloid leukemia (AML). In this context, myeloid is used broadly to refer to non-lymphoid precursors rather than the more limited meaning granulopoietic:
- AML.
- AML with recurrent cytogenetic abnormalities, e.g. t(8;21), inv(16) and t(15;17).
- AML arising from MDS.
- AML in the setting of Down syndrome.
- Acute lymphoblastic leukemia (ALL):
- B cell.
- B cell with recurrent cytogenetic abnormalities.
- T cell (sometimes abbreviated to T-ALL)
- T-ALL should not to be confused with adult T-cell leukemia/lymphoma (ATLL) - this is associated with HTLV-1 infection
- Chronic lymphocytic leukemia (CLL) - usually classified with lymphomas
A few fall under the umbrella of myeloproliferative neoplasms:
- Chronic myeloid leukemia (CML)
- Chronic neutrophilic leukemia (rare)
- Chronic eosinophilic leukemia (rare)
And others under the myeloproliferative/myelodysplastic overlap syndromes:
Other less common leukemias:
- Hairy cell leukemia
- T-cell prolymphocytic leukemia
- T-cell large granular lymphocyte leukaemia (T-LGL)
- Plasma cell leukaemia
- Mast cell leukemia
Histomorphologic overview
| Disease/Feature | Blast size | Auer rods | Granulation of cytoplasm |
| Acute myeloid leukemia (AML) | larger | present | present |
| Acute lymphoid leukemia (ALL) | smaller † | none | absent or present |
† should be easy to remember as smALL people, i.e. kids, get this type of acute leukemia.
Algorithms
There is a nice set of algorithms from D. Arber - that were presented at the 2009 USCAP.
Clinical factors in classification
Clinical are important in the classification of leukemia.
- Hx of myelodysplastic syndrome?
- Chemotherapy?
- Down syndrome?
Prognosis
Highly dependent on health care system and treatment available[3]
- 5-year overall survival in children ranges:
- lymphoid leukaemia: 52.4% (Colombia) to 91.6% (Germany)
- acute myleoid leukemia: 33.3% (Bulgaria) to 78.2% (Germany)
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 314. ISBN 978-1416054542.
- ↑ D. Good. 21 March 2011.
- ↑ Bonaventure, A.; Harewood, R.; Stiller, CA.; Gatta, G.; Clavel, J.; Stefan, DC.; Carreira, H.; Spika, D. et al. (Apr 2017). "Worldwide comparison of survival from childhood leukaemia for 1995-2009, by subtype, age, and sex (CONCORD-2): a population-based study of individual data for 89 828 children from 198 registries in 53 countries.". Lancet Haematol. doi:10.1016/S2352-3026(17)30052-2. PMID 28411119.