Difference between revisions of "Giardiasis"
Jump to navigation
Jump to search
(→www: mk nicer) |
|||
| (2 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Giardia_small_bowel_--_high_mag.jpg | ||
| Width = | | Width = | ||
| Caption = Giardiasis. [[H&E stain]]. | | Caption = Giardiasis. [[H&E stain]]. | ||
| Line 57: | Line 57: | ||
Features: | Features: | ||
*+/-Loss of villi. | *+/-Loss of villi. | ||
*Intraepithelial lymphocytes. | *[[Intraepithelial lymphocytes]]. | ||
**+Other inflammatory cells, especially PMNs, close to the luminal surface. | **+Other inflammatory cells, especially [[PMNs]], close to the luminal surface. | ||
*Flagellate protozoa -- '''diagnostic feature'''. | *Flagellate protozoa -- '''diagnostic feature'''. | ||
**Organisms often at site of bad inflammation. | **Organisms often at site of bad inflammation. | ||
| Line 72: | Line 72: | ||
===Images=== | ===Images=== | ||
====Case 1==== | |||
<gallery> | <gallery> | ||
Image:Giardiasis_duodenum_high.jpg | Giardiasis - high mag. (WC) | Image:Giardiasis_duodenum_high.jpg | Giardiasis - high mag. (WC) | ||
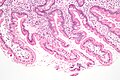
Image:Giardiasis_duodenum_low.jpg | Giardiasis - low mag. (WC) | Image:Giardiasis_duodenum_low.jpg | Giardiasis - low mag. (WC) | ||
</gallery> | </gallery> | ||
www | ====Case 2==== | ||
*[http://path.upmc.edu/cases/case278.html Giardiasis - several | <gallery> | ||
Giardia small bowel -- low mag.jpg | Giardia - low mag. | |||
Giardia small bowel -- intermed mag.jpg | Giardia - intermed. mag. | |||
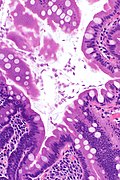
Giardia small bowel -- high mag.jpg | Giardia - high mag. | |||
Giardia small bowel - alt -- high mag.jpg | Giardia - high mag. | |||
Giardia small bowel -- very high mag.jpg | Giardia - very high mag. | |||
</gallery> | |||
====www==== | |||
*[http://path.upmc.edu/cases/case278.html Giardiasis - several images (upmc.edu)]. | |||
==Stains== | ==Stains== | ||
Latest revision as of 21:32, 14 July 2019
| Giardiasis | |
|---|---|
| Diagnosis in short | |
 Giardiasis. H&E stain. | |
|
| |
| LM | flagellate protozoa - pale/transluence on H&E, 12-15 micrometers (long axis) x 6-10 micrometers (short axis); +/-loss of villi, intraepithelial lymphocytes, inflammatory cells - especially close to the luminal surface |
| LM DDx | celiac disease |
| Stains | methylene blue +ve |
| IHC | CD117 +ve (microorganisms) |
| Site | duodenum |
|
| |
| Signs | diarrhea x5 days, foul smelling feces, flatulence |
| Symptoms | fatigue, abdominal cramps, nausea |
| Prevalence | uncommon |
| Endoscopy | +/-white spots, diffuse changes |
| Prognosis | good, benign |
| Clin. DDx | celiac disease, other causes of diarrhea |
| Treatment | antibiotics |
Giardiasis is a rare infection, classically found in the duodenum. It can mimic celiac disease. It is also known as beaver fever.
General
Clinical features - usually two or more of the following:[1]
- Diarrhea - x5 days.
- Flatulence.
- Foul smelling feces.
- Nausea.
- Abdominal cramps.
- Excessive tiredness.
Epidemiology:
- Uncommon.
Etiology:
- Flagellate protozoan Giardia lamblia.
Treatment
- Antibiotics, e.g. metronidazole (Flagyl).
Gross
- Diffuse changes.
- May have scattered white spots.[2]
Microscopic
Features:
- +/-Loss of villi.
- Intraepithelial lymphocytes.
- +Other inflammatory cells, especially PMNs, close to the luminal surface.
- Flagellate protozoa -- diagnostic feature.
- Organisms often at site of bad inflammation.
- Pale/translucent on H&E.
- Size: 12-15 micrometers (long axis) x 6-10 micrometers (short axis) -- if seen completely.[3]
- Often look like a crescent moon (image of crescent moon) or semicircular[4] -- as the long axis of the organism is rarely in the plane of the (histologic) section.
Note:
- Changes are typically diffuse, i.e. if multiple biopsies are done the changes are present in all fragments.[5]
DDx:
- Celiac disease - near perfect mimic; missing giardia organisms.
Images
Case 1
Case 2
www
Stains
- Methylene blue +ve.[6]
IHC
- CD117 +ve.[7]
Sign out
A. Duodenum, Biopsy: - Abundant micro-organisms consistent with GIARDIA and small bowel mucosa with increased intraepithelial lymphocytes, see comment. - NEGATIVE for dysplasia. B. Stomach, Biopsy: - Body and antral-type mucosa with mild chronic inactive inflammation. - NEGATIVE for Helicobacter-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: The increased intraepithelial lymphocytes are likely to due to the Giardia; however, other causes cannot be excluded.
Block letters
DUODENUM, BIOPSY: - SMALL BOWEL MUCOSA WITH BRUNNER'S GLANDS AND MICROORGANISMS CONSISTENT WITH GIARDIA.
See also
References
- ↑ Hopkins, RS.; Juranek, DD. (Feb 1991). "Acute giardiasis: an improved clinical case definition for epidemiologic studies.". Am J Epidemiol 133 (4): 402-7. PMID 1994703.
- ↑ Biyikoğlu, I.; Babali, A.; Cakal, B.; Köklü, S.; Filik, L.; Astarci, MH.; Ustün, H.; Ustündağ, Y. et al. (Nov 2009). "Do scattered white spots in the duodenum mark a specific gastrointestinal pathology?". J Dig Dis 10 (4): 300-4. doi:10.1111/j.1751-2980.2009.00399.x. PMID 19906109.
- ↑ http://www.water-research.net/Giardia.htm
- ↑ http://en.wikipedia.org/wiki/Semicircle
- ↑ Freeman, HJ. (Mar 2008). "Pearls and pitfalls in the diagnosis of adult celiac disease.". Can J Gastroenterol 22 (3): 273-80. PMID 18354756.
- ↑ Rajurkar, MN.; Lall, N.; Basak, S.; Mallick, SK. (Nov 2012). "A simple method for demonstrating the giardia lamblia trophozoite.". J Clin Diagn Res 6 (9): 1492-4. doi:10.7860/JCDR/2012/4358.2541. PMID 23285438.
- ↑ Sinelnikov, I.; Sion-Vardy, N.; Shaco-Levy, R. (Mar 2009). "C-kit (CD117) immunostain is useful for the diagnosis of Giardia lamblia in duodenal biopsies.". Hum Pathol 40 (3): 323-5. doi:10.1016/j.humpath.2008.07.015. PMID 18835628.