Difference between revisions of "Usual interstitial pneumonia"
Jump to navigation
Jump to search
(→Micro) |
m (→Alternate) |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 84: | Line 84: | ||
==Sign out== | ==Sign out== | ||
<pre> | |||
A. Lung, Right Lower Lobe, Wedge Biopsy: | |||
- Usual interstitial pneumonia, see comment and microscopic. | |||
B. Lung, Right Middle Lobe, Wedge Biopsy: | |||
- Usual interstitial pneumonia, see comment and microscopic. | |||
C. Lung, Right Upper Lobe, Wedge Biopsy: | |||
- Usual interstitial pneumonia, see comment and microscopic. | |||
Comment: | |||
There are no findings to specifically suggest hypersensitivity. Clinical and radiologic | |||
correlation is suggested. | |||
</pre> | |||
===Alternate=== | |||
<pre> | |||
Right Lower Lobe of Lung, Wedge Resection: | |||
- Usual interstitial pneumonia (UIP) pattern (fibroblast foci, bronchiolization, | |||
extensive fibroelastotic scarring and focal calcification/bone formation), see comment. | |||
Comment: | |||
UIP pattern may be idiopathic. It is also be seen in the context of collagen vascular diseases, hypersensitivity reactions, and drugs; these need to be considered in clinical context along with the imaging findings. | |||
</pre> | |||
===Micro=== | ===Micro=== | ||
<pre> | <pre> | ||
Sections show lung parenchyma with: | Sections show lung parenchyma with: | ||
Fibrosis: present | Fibrosis (severity; lobar location): present (moderate-to-severe; peripheral predominant). | ||
Fibrosis - lung field predominance: lower lobe > middle lobe > upper lobe. | |||
Fibroblast foci: present. | Fibroblast foci: present. | ||
Temporal heterogeneity: present. | |||
Spatial heterogeneity: present. | |||
Peripheral cyst formation: present. | Peripheral cyst formation: present. | ||
Inflammation: present - patchy, lymphocyte predominant. | Inflammation: present - patchy, lymphocyte predominant. | ||
Granulomatous inflammation: absent. | Granulomatous inflammation: absent. | ||
Blood vessel changes: | Blood vessel changes: present, moderate-to-severe. | ||
Airspace changes: mucous plugs. | Airspace changes: mucous plugs. | ||
</pre> | </pre> | ||
Latest revision as of 22:32, 7 February 2022
| Usual interstitial pneumonia | |
|---|---|
| Diagnosis in short | |
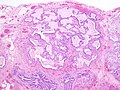
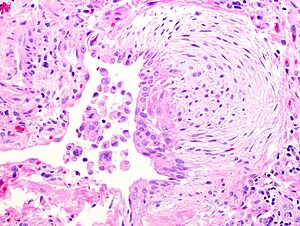 Fibroblast focus in usual interstitial pneumonia. H&E stain. | |
|
| |
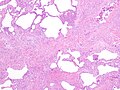
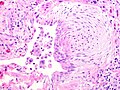
| LM | fibroblast foci, interstitial inflammation, microscopic honeycombing (typically peripheral & lined by ciliated epithelium), spatial heterogeneity - patchy lesional distribution (areas of abnormal and normal lung may appear beside one another), temporal heterogeneity - lesions of differing age side-by-side |
| LM DDx | asbestosis, chronic hypersensitivity pneumonitis, collagen vascular disease (e.g. systemic lupus erythematosus, rheumatoid arthritis, scleroderma), chronic drug toxicity |
| Stains | iron stain -ve |
| Gross | lower lobe & periperal predominant: fibrosis, peripheral cysts |
| Site | lung - see diffuse lung diseases |
|
| |
| Signs | signs of right heart failure |
| Symptoms | shortness of breath |
| Prevalence | uncommon |
| Radiology | interstitial pattern, lower lobe predominant, peripheral cysts |
| Prognosis | usually poor, dependent on amount of fibrosis |
| Other | histologic correlate of idiopathic pulmonary fibrosis |
| Clin. DDx | asbestosis, chronic hypersensitivity pneumonitis, collagen vascular disease (history missing), chronic drug toxicity (history missing), idiopathic pulmonary fibrosis |
| Treatment | lung transplantation |
Usual interstitial pneumonia, abbreviated UIP, is a relatively common pattern in diffuse lung diseases. Overall, it is an uncommon pathology.
Idiopathic pulmonary fibrosis (abbreviated IPF) redirects here.
General
- It is sometimes used incorrectly as a synonym for idiopathic pulmonary fibrosis. It is a histomorphologic pattern and has a DDx (see below).
- UIP cannot be diagnosed via bronchoscopic or transbronchial biopsy,[1] as it is peripheral.
Epidemiology
- Disease of the old - rare in under 50 years old.[2]
- Dismal prognosis - mean survival after diagnosis ~ 2.8 years.[3]
Radiology
- Honeycombing - multiple defects that obliterate the normal lung architecture - multiple spherical voids in the lung parenchyma; radiologically these are seen as lucencies.[4]
- Usually subplural, i.e. peripheral lung.
- Classically lower lobe predominant.
- Traction bronchiectasis.
Note:
- Cysts - have thin walls (think of emphysema, lymphangioleiomyomatosis et cetera).
- Cysts may be isolated/not close to a neighbour.
- Medcyclopaedia defines it as: thin-walled, well-demarcated and >1 cm.[5]
Microscopic
Features:[6]
- Fibroblast foci:
- Interstitial inflammation.
- Microscopic honeycombing.
- Typically peripheral - cysts lined by ciliated epithelium.
- Spatial heterogeneity - patchy lesional distribution (areas of abnormal and normal lung may appear beside one another).
- Temporal heterogeneity - lesions of differing age side-by-side.[9]
Notes:
- Disease worse distant from large airways: lower lung field predominance, typically worse at periphery of lobule and lung.[10]
- Heterogeneity of inflammation: airspace macrophages & inflammation minimal in honeycombed foci.
DDx of UIP:[11]
- Idiopathic pulmonary fibrosis (UIP not otherwise specified).
- Asbestosis = UIP-like pattern + ferruginous bodies with asbestos fibers.
- Chronic hypersensitivity pneumonitis (AKA extrinsic allergic alveolitis) - classically centrilobular predominant +/- granulomas.
- Collagen vascular disease - includes systemic lupus erythematosus, rheumatoid arthritis, scleroderma.[12]
- Chronic drug toxicity.[13]
Images
Sign out
A. Lung, Right Lower Lobe, Wedge Biopsy: - Usual interstitial pneumonia, see comment and microscopic. B. Lung, Right Middle Lobe, Wedge Biopsy: - Usual interstitial pneumonia, see comment and microscopic. C. Lung, Right Upper Lobe, Wedge Biopsy: - Usual interstitial pneumonia, see comment and microscopic. Comment: There are no findings to specifically suggest hypersensitivity. Clinical and radiologic correlation is suggested.
Alternate
Right Lower Lobe of Lung, Wedge Resection:
- Usual interstitial pneumonia (UIP) pattern (fibroblast foci, bronchiolization,
extensive fibroelastotic scarring and focal calcification/bone formation), see comment.
Comment:
UIP pattern may be idiopathic. It is also be seen in the context of collagen vascular diseases, hypersensitivity reactions, and drugs; these need to be considered in clinical context along with the imaging findings.
Micro
Sections show lung parenchyma with: Fibrosis (severity; lobar location): present (moderate-to-severe; peripheral predominant). Fibrosis - lung field predominance: lower lobe > middle lobe > upper lobe. Fibroblast foci: present. Temporal heterogeneity: present. Spatial heterogeneity: present. Peripheral cyst formation: present. Inflammation: present - patchy, lymphocyte predominant. Granulomatous inflammation: absent. Blood vessel changes: present, moderate-to-severe. Airspace changes: mucous plugs.
See also
References
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 186. ISBN 978-0443066313.
- ↑ AC UBC S.102.
- ↑ Bjoraker, JA.; Ryu, JH.; Edwin, MK.; Myers, JL.; Tazelaar, HD.; Schroeder, DR.; Offord, KP. (Jan 1998). "Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis.". Am J Respir Crit Care Med 157 (1): 199-203. PMID 9445300.
- ↑ http://www.medcyclopaedia.com/library/topics/volume_v_1/h/honeycombing.aspx
- ↑ http://www.medcyclopaedia.com/library/topics/volume_v_1/l/lung_cyst.aspx
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 186-9. ISBN 978-0443066313.
- ↑ http://www.epler.com/IPFWhat%27sIPFDiseaseInformation2.htm
- ↑ Leslie, Kevin O.; Wick, Mark R. (2004). Practical Pulmonary Pathology: A Diagnostic Approach (1st ed.). Churchill Livingstone. pp. 189. ISBN 978-0443066313.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 92. ISBN 978-0781765275.
- ↑ A. Churg. UBC S.103.
- ↑ Wick, Mark R.; Leslie, Kevin (2005). Practical pulmonary pathology: a diagnostic approach. Edinburgh: Churchill Livingstone. ISBN 0-443-06631-0. OCLC 156861539.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 374. ISBN 978-1416054542.
- ↑ Rossi SE, Erasmus JJ, McAdams HP, Sporn TA, Goodman PC (2000). "Pulmonary drug toxicity: radiologic and pathologic manifestations". Radiographics : a review publication of the Radiological Society of North America, Inc 20 (5): 1245-59. PMID 10992015.