Difference between revisions of "Granulation tissue"
(create) |
(touch) |
||
| (16 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Granulation tissue''' forms when | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Granulation tissue in an infected wound, HE 3.JPG | |||
| Width = | |||
| Caption = Granulation tissue. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = blood vessel rich - '''key element''', proliferation of fibroblasts - '''key element''', inflammation - especially lymphocytes ([[plasma cell]]s common), +/- evidence of erosion/ulceration | |||
| Subtypes = | |||
| LMDDx = [[mucocele]], traumatized [[hemangioma]], [[pyogenic granuloma]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = granular appearance, erythematous | |||
| Grossing = | |||
| Site = [[skin]], [[gastrointestinal tract]], other | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = +/-trauma | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = common | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = | |||
| Tx = +/-debridement | |||
}} | |||
'''Granulation tissue''' forms when wounds heal. | |||
==Gross== | ==Gross== | ||
*Looks granular, ergo the name ''granulation tissue''. | *Looks granular, ergo the name ''granulation tissue''. | ||
Image | ===Image=== | ||
<gallery> | |||
Image:Finger_with_granulation_tissue.jpg | Granulation. (WC) | |||
</gallery> | |||
==Microscopic== | ==Microscopic== | ||
Features: | Features: | ||
*Blood | *Blood vessel rich - '''key element'''.<ref name=pmid11266270>{{cite journal |author=Howdieshell TR, Callaway D, Webb WL, ''et al.'' |title=Antibody neutralization of vascular endothelial growth factor inhibits wound granulation tissue formation |journal=J. Surg. Res. |volume=96 |issue=2 |pages=173–82 |year=2001 |month=April |pmid=11266270 |doi=10.1006/jsre.2001.6089 |url=}}</ref> | ||
**Small size ~ 25 micrometers in diameter.{{fact}} | |||
*Proliferation of fibroblasts - '''key element'''. | *Proliferation of fibroblasts - '''key element'''. | ||
*Inflammation | *Inflammation - especially lymphocytes. | ||
**[[Plasma cell]]s common. | |||
Images: | DDx: | ||
*[[Mucocele]]. | |||
*[[Pyogenic granuloma]]. | |||
*Traumatized [[hemangioma]]. | |||
*Prolapsed [[fallopian tube]] - rare complication following [[hysterectomy]].<ref>{{Cite journal | last1 = Fan | first1 = QB. | last2 = Liu | first2 = ZF. | last3 = Lang | first3 = JH. | last4 = Sun | first4 = DW. | last5 = Leng | first5 = JH. | last6 = Zhu | first6 = L. | last7 = Ning | first7 = L. | title = Fallopian tube prolapse following hysterectomy. | journal = Chin Med Sci J | volume = 21 | issue = 1 | pages = 20-3 | month = Mar | year = 2006 | doi = | PMID = 16615279 }}</ref> | |||
===Images=== | |||
<gallery> | |||
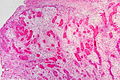
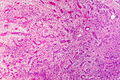
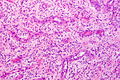
Granulation tissue in an infected wound, HE 1.JPG | GT. (WC/Patho) | |||
Granulation tissue in an infected wound, HE 2.JPG | GT. (WC/Patho) | |||
Granulation tissue in an infected wound, HE 3.JPG | GT. (WC/Patho) | |||
</gallery> | |||
www: | |||
*[http://oac.med.jhmi.edu/pathconcepts/ShowImage.cfm?TutorialID=8&ConceptID=47&ImageID=127 Granulation tissue with entrapped muscle (jhmi.edu)]. | *[http://oac.med.jhmi.edu/pathconcepts/ShowImage.cfm?TutorialID=8&ConceptID=47&ImageID=127 Granulation tissue with entrapped muscle (jhmi.edu)]. | ||
*[http://www.siumed.edu/~dking2/intro/skinbiop/images/GT1.jpg Granulation tissue (siumed.edu)].<ref>URL: [http://www.siumed.edu/~dking2/intro/inflskin.htm http://www.siumed.edu/~dking2/intro/inflskin.htm]. Accessed on: 17 January 2011.</ref> | *[http://www.siumed.edu/~dking2/intro/skinbiop/images/GT1.jpg Granulation tissue (siumed.edu)].<ref>URL: [http://www.siumed.edu/~dking2/intro/inflskin.htm http://www.siumed.edu/~dking2/intro/inflskin.htm]. Accessed on: 17 January 2011.</ref> | ||
==Sign out== | |||
<pre> | |||
Submitted as "Granulation Tissue - Vaginal", Excision: | |||
- Granulation tissue, see comment. | |||
- NEGATIVE for epithelium. | |||
- NEGATIVE for evidence of malignancy. | |||
Comment: | |||
Clinical correlation and follow-up is recommended. | |||
</pre> | |||
===Block letters=== | |||
<pre> | |||
URINARY BLADDER, BIOPSY: | |||
- REGENERATIVE EPITHELIUM, INFLAMED SUBEPITHELIAL TISSUE AND GRANULATION TISSUE. | |||
- NO MUSCULARIS PROPRIA. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
TISSUE, VAGINAL VAULT, BIOPSY: | |||
- GRANULATION TISSUE. | |||
- NEGATIVE FOR FALLOPIAN TUBE. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
===Micro=== | |||
The sections show vascular tissue with plump fibroblasts, reactive endothelial cells | |||
and a mixed inflammatory infiltrate (granulation tissue). Focally, a dense | |||
cluster of neutrophils is seen at the luminal aspect. | |||
A single layer of epithelium with pale, plump nuclei is present without apparent mitotic | |||
activity. Inflamed subepithelial tissue is present. No stratified urothelium is identified. No significant nuclear atypia is present. | |||
====Alternate==== | |||
The sections show a polypoid fragment of vascular and edematous tissue with a mixed | |||
inflammatory infiltrate consisting of plasma cells, neutrophils and lymphocytes. | |||
No epithelial component is readily identified. No elements of fallopian tube are identified. No significant nuclear atypia is identified. | |||
==See also== | |||
*[[Basics]]. | |||
*[[Cap polyposis]]. | |||
==References== | ==References== | ||
Latest revision as of 16:54, 6 February 2016
| Granulation tissue | |
|---|---|
| Diagnosis in short | |
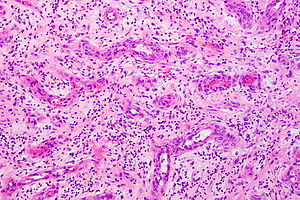 Granulation tissue. H&E stain. | |
|
| |
| LM | blood vessel rich - key element, proliferation of fibroblasts - key element, inflammation - especially lymphocytes (plasma cells common), +/- evidence of erosion/ulceration |
| LM DDx | mucocele, traumatized hemangioma, pyogenic granuloma |
| Gross | granular appearance, erythematous |
| Site | skin, gastrointestinal tract, other |
|
| |
| Clinical history | +/-trauma |
| Prevalence | common |
| Prognosis | benign |
| Treatment | +/-debridement |
Granulation tissue forms when wounds heal.
Gross
- Looks granular, ergo the name granulation tissue.
Image
Microscopic
Features:
- Blood vessel rich - key element.[1]
- Small size ~ 25 micrometers in diameter.[citation needed]
- Proliferation of fibroblasts - key element.
- Inflammation - especially lymphocytes.
- Plasma cells common.
DDx:
- Mucocele.
- Pyogenic granuloma.
- Traumatized hemangioma.
- Prolapsed fallopian tube - rare complication following hysterectomy.[2]
Images
www:
Sign out
Submitted as "Granulation Tissue - Vaginal", Excision: - Granulation tissue, see comment. - NEGATIVE for epithelium. - NEGATIVE for evidence of malignancy. Comment: Clinical correlation and follow-up is recommended.
Block letters
URINARY BLADDER, BIOPSY: - REGENERATIVE EPITHELIUM, INFLAMED SUBEPITHELIAL TISSUE AND GRANULATION TISSUE. - NO MUSCULARIS PROPRIA. - NEGATIVE FOR MALIGNANCY.
TISSUE, VAGINAL VAULT, BIOPSY: - GRANULATION TISSUE. - NEGATIVE FOR FALLOPIAN TUBE. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show vascular tissue with plump fibroblasts, reactive endothelial cells and a mixed inflammatory infiltrate (granulation tissue). Focally, a dense cluster of neutrophils is seen at the luminal aspect.
A single layer of epithelium with pale, plump nuclei is present without apparent mitotic activity. Inflamed subepithelial tissue is present. No stratified urothelium is identified. No significant nuclear atypia is present.
Alternate
The sections show a polypoid fragment of vascular and edematous tissue with a mixed inflammatory infiltrate consisting of plasma cells, neutrophils and lymphocytes.
No epithelial component is readily identified. No elements of fallopian tube are identified. No significant nuclear atypia is identified.
See also
References
- ↑ Howdieshell TR, Callaway D, Webb WL, et al. (April 2001). "Antibody neutralization of vascular endothelial growth factor inhibits wound granulation tissue formation". J. Surg. Res. 96 (2): 173–82. doi:10.1006/jsre.2001.6089. PMID 11266270.
- ↑ Fan, QB.; Liu, ZF.; Lang, JH.; Sun, DW.; Leng, JH.; Zhu, L.; Ning, L. (Mar 2006). "Fallopian tube prolapse following hysterectomy.". Chin Med Sci J 21 (1): 20-3. PMID 16615279.
- ↑ URL: http://www.siumed.edu/~dking2/intro/inflskin.htm. Accessed on: 17 January 2011.