Difference between revisions of "Urothelial dysplasia"
Jump to navigation
Jump to search
(create) |
(→IHC) |
||
| (30 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
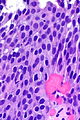
| Image = Urothelial dysplasia - alt -- high mag.jpg | |||
| Width = | |||
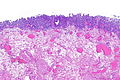
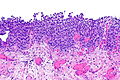
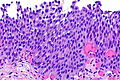
| Caption = Urothelial dysplasia. [[H&E stain]]. | |||
| Synonyms = low-grade urothelial dysplasia | |||
| Micro = mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia, mild disorganization of the architecture (some maturation), occasional mitotic figures - none atypical | |||
| Subtypes = | |||
| LMDDx = reactive changes, urothelial atypia of unknown significance, [[urothelial carcinoma in situ]] | |||
| Stains = | |||
| IHC = CK20 +ve/-ve (esp. non-umbrella cells), Ki-67 +ve/-ve (>10%), p53 +ve/-ve (>20%) | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[urothelium]] (renal pelvis, [[urinary bladder]], [[ureters]], [[urethra]]) | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = common | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = pre-malignant | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
'''Urothelial dysplasia''', also '''low-grade (urothelial) dysplasia''', is a lesion of the [[urothelium]] in the ISUP/WHO 2004 classification.<ref name=pmid19762067>{{Cite journal | last1 = Hodges | first1 = KB. | last2 = Lopez-Beltran | first2 = A. | last3 = Davidson | first3 = DD. | last4 = Montironi | first4 = R. | last5 = Cheng | first5 = L. | title = Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features. | journal = Hum Pathol | volume = 41 | issue = 2 | pages = 155-62 | month = Feb | year = 2010 | doi = 10.1016/j.humpath.2009.07.002 | PMID = 19762067 }}</ref> | '''Urothelial dysplasia''', also '''low-grade (urothelial) dysplasia''', is a lesion of the [[urothelium]] in the ISUP/WHO 2004 classification.<ref name=pmid19762067>{{Cite journal | last1 = Hodges | first1 = KB. | last2 = Lopez-Beltran | first2 = A. | last3 = Davidson | first3 = DD. | last4 = Montironi | first4 = R. | last5 = Cheng | first5 = L. | title = Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features. | journal = Hum Pathol | volume = 41 | issue = 2 | pages = 155-62 | month = Feb | year = 2010 | doi = 10.1016/j.humpath.2009.07.002 | PMID = 19762067 }}</ref> | ||
It is precursor lesion to [[urothelial carcinoma]] that is less worrisome than [[urothelial carcinoma in situ]]. | |||
It is precursor lesion to [[urothelial carcinoma]] that is less worrisome than [[urothelial carcinoma in situ]] (also known as ''high-grade (urothelial) dysplasia''). | |||
==General== | ==General== | ||
The ISUP/WHO classification of flat urothelial lesions is:<ref name=pmid19762067>{{Cite journal | last1 = Hodges | first1 = KB. | last2 = Lopez-Beltran | first2 = A. | last3 = Davidson | first3 = DD. | last4 = Montironi | first4 = R. | last5 = Cheng | first5 = L. | title = Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features. | journal = Hum Pathol | volume = 41 | issue = 2 | pages = 155-62 | month = Feb | year = 2010 | doi = 10.1016/j.humpath.2009.07.002 | PMID = 19762067 }}</ref> | The [[ISUP]]/WHO classification of flat urothelial lesions is:<ref name=pmid19762067>{{Cite journal | last1 = Hodges | first1 = KB. | last2 = Lopez-Beltran | first2 = A. | last3 = Davidson | first3 = DD. | last4 = Montironi | first4 = R. | last5 = Cheng | first5 = L. | title = Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features. | journal = Hum Pathol | volume = 41 | issue = 2 | pages = 155-62 | month = Feb | year = 2010 | doi = 10.1016/j.humpath.2009.07.002 | PMID = 19762067 }}</ref> | ||
*Reactive urothelial atypia. | *Reactive urothelial atypia. | ||
*Flat urothelial hyperplasia. | *Flat urothelial hyperplasia. | ||
*Urothelial atypia of unknown significance. | *Urothelial atypia of unknown significance. | ||
* | *Urothelial dysplasia (low-grade dysplasia). | ||
*Urothelial carcinoma in situ (high-grade dysplasia). | *[[Urothelial carcinoma in situ]] (high-grade dysplasia). | ||
*Invasive urothelial carcinoma. | *Invasive urothelial carcinoma. | ||
| Line 15: | Line 47: | ||
*Mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia. | *Mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia. | ||
*Slight disorganization of the architecture. | *Slight disorganization of the architecture. | ||
**Some maturation to the surface. | **Some maturation to the surface - '''important'''. | ||
*Mitotic figures - occasional, none atypical. | *Mitotic figures - occasional, none atypical. | ||
Notes: | |||
*It is probably not a good idea to make this diagnosis without immunohistochemistry. | |||
*This diagnosis '''not''' made on [[frozen section]]. | |||
DDx: | DDx: | ||
*[[Urothelial carcinoma in situ]]. | *Benign urothelium with reactive changes. | ||
*[[Urothelial carcinoma in situ]] - no maturation to the surface or marked atypia - as in pagetoid [[UCIS]] and undermining UCIS.<ref name=pmid11224606>{{Cite journal | last1 = McKenney | first1 = JK. | last2 = Gomez | first2 = JA. | last3 = Desai | first3 = S. | last4 = Lee | first4 = MW. | last5 = Amin | first5 = MB. | title = Morphologic expressions of urothelial carcinoma in situ: a detailed evaluation of its histologic patterns with emphasis on carcinoma in situ with microinvasion. | journal = Am J Surg Pathol | volume = 25 | issue = 3 | pages = 356-62 | month = Mar | year = 2001 | doi = | PMID = 11224606 }}</ref> | |||
===Images=== | ===Images=== | ||
<gallery> | |||
Image: Urothelial dysplasia -- low mag.jpg | UD - low mag. (WC) | |||
Image: Urothelial dysplasia -- intermed mag.jpg | UD - intermed. mag. (WC) | |||
Image: Urothelial dysplasia -- high mag.jpg | UD - high mag. (WC) | |||
Image: Urothelial dysplasia - alt -- high mag.jpg | UD - high mag. (WC) | |||
Image: Urothelial dysplasia -- very high mag.jpg | UD - very high mag. (WC) | |||
Image: Urothelial dysplasia - CK20 -- intermed mag.jpg | UD - intermed. mag. (WC) | |||
Image: Urothelial dysplasia - CK20 -- high mag.jpg | UD - high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://pathology.jhu.edu/bladder/image1.cfm?case_number=10&image_number=1 Urothelial dysplasia (jhu.edu)]. | *[http://pathology.jhu.edu/bladder/image1.cfm?case_number=10&image_number=1 Urothelial dysplasia (jhu.edu)]. | ||
==IHC== | |||
A comparison between benign, dysplasia and [[UCIS]]:<ref name=pmid12640096>{{Cite journal | last1 = Mallofré | first1 = C. | last2 = Castillo | first2 = M. | last3 = Morente | first3 = V. | last4 = Solé | first4 = M. | title = Immunohistochemical expression of CK20, p53, and Ki-67 as objective markers of urothelial dysplasia. | journal = Mod Pathol | volume = 16 | issue = 3 | pages = 187-91 | month = Mar | year = 2003 | doi = 10.1097/01.MP.0000056628.38714.5D | PMID = 12640096 }}</ref> | |||
{| class="wikitable sortable" | |||
! Diagnosis | |||
! CK20 | |||
! Ki-67 | |||
! p53 | |||
! p63 ‡ | |||
|- | |||
| Benign (reactive) | |||
| umbrella cells +ve only | |||
| -ve <=10% of cells (+/-rare basal cells) | |||
| -ve <20% of cells (+/-weak staining) | |||
| -ve surface cells | |||
|- | |||
| Urothelial dysplasia | |||
| +ve non-umbrella cells +ve (~30% of cases) | |||
| +ve >10% of cells (~40% of cases) | |||
| +ve >=20% of cells (~70% of cases) | |||
| -ve surface cells<ref name=pmid19690775>{{Cite journal | last1 = Stepan | first1 = A. | last2 = Mărgăritescu | first2 = C. | last3 = Simionescu | first3 = C. | last4 = Ciurea | first4 = R. | title = E-cadherin and p63 immunoexpression in dysplastic lesions and urothelial carcinomas of the bladder. | journal = Rom J Morphol Embryol | volume = 50 | issue = 3 | pages = 461-5 | month = | year = 2009 | doi = | PMID = 19690775 }}</ref><ref name=OJP>{{Cite journal | last1 = Raheem| first1 = Sayad A.| last2 = Saied | first2 = Abdel N. | last3 = Al Shaer | first3 = Rabee | last4 = Mustafa | first4 = Osama | last5 = Ali | first5 = Ali H. | title = The Role of CK20, p53 and p63 in Differentiation of Some Urothelial Lesions of Urinary Bladder, Immunohistochemical Study | journal = [http://www.scirp.org/journal/ojpathology Open Journal of Pathology] | volume = | issue = 4| pages = 181-193 | month = | year = 2014 | doi = 10.4236/ojpathology.2014.44024 | PMID = | PMC = | url = }}</ref> | |||
|- | |||
| [[Urothelial carcinoma in situ|Urothelial carcinoma in situ]] (UCIS) | |||
| +ve non-umbrella cells (~70% of cases) | |||
| +ve >10% of cells (~95% of cases) | |||
| +ve >=20% of cells (~80% of cases) | |||
| +ve surface cells<ref name=pmid19690775/><ref name=OJP/> | |||
|} | |||
Note: | |||
*‡ Morphology is considered the gold standard for UCIS versus urothelial dysplasia;<ref name=pmid25029121>{{cite journal |authors=Amin MB, Trpkov K, Lopez-Beltran A, Grignon D |title=Best practices recommendations in the application of immunohistochemistry in the bladder lesions: report from the International Society of Urologic Pathology consensus conference |journal=Am J Surg Pathol |volume=38 |issue=8 |pages=e20–34 |date=August 2014 |pmid=25029121 |doi=10.1097/PAS.0000000000000240 |url=}}</ref> however, there is a small literature on [[p63]] for dysplasia versus UCIS that is published in lesser known journals. | |||
==Sign out== | |||
<pre> | |||
Urinary Bladder, Biopsy: | |||
- Urothelial dysplasia, see comment. | |||
- Giant cell reaction and chronic inflammation. | |||
Comment: | |||
The urothelium has moderate CK20 staining that extends to the basement membrane. A p53 stain is negative (<10% staining). A Ki-67 stain shows increased staining (marks 20% of urothelium). A p63 stain shows weak/negative surface staining. | |||
</pre> | |||
===Block letters=== | |||
<pre> | |||
RIGHT URETER (MARGIN), EXCISION: | |||
- UROTHELIAL DYSPLASIA, SEE COMMENT. | |||
- NEGATIVE FOR UROTHELIAL CARCINOMA. | |||
COMMENT: | |||
There is focal non-umbrella cell CK20 staining, 10% (focal) urothelial | |||
p53 staining, and 30% (focal) urothelial Ki-67 staining. The findings | |||
are that of (low-grade) urothelial dysplasia. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Urothelium]]. | *[[Urothelium]]. | ||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Genitourinary pathology]] | [[Category:Genitourinary pathology]] | ||
Latest revision as of 19:38, 31 December 2020
| Urothelial dysplasia | |
|---|---|
| Diagnosis in short | |
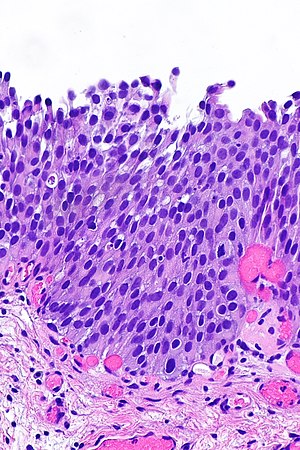 Urothelial dysplasia. H&E stain. | |
|
| |
| Synonyms | low-grade urothelial dysplasia |
|
| |
| LM | mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia, mild disorganization of the architecture (some maturation), occasional mitotic figures - none atypical |
| LM DDx | reactive changes, urothelial atypia of unknown significance, urothelial carcinoma in situ |
| IHC | CK20 +ve/-ve (esp. non-umbrella cells), Ki-67 +ve/-ve (>10%), p53 +ve/-ve (>20%) |
| Site | urothelium (renal pelvis, urinary bladder, ureters, urethra) |
|
| |
| Prevalence | common |
| Prognosis | pre-malignant |
Urothelial dysplasia, also low-grade (urothelial) dysplasia, is a lesion of the urothelium in the ISUP/WHO 2004 classification.[1]
It is precursor lesion to urothelial carcinoma that is less worrisome than urothelial carcinoma in situ (also known as high-grade (urothelial) dysplasia).
General
The ISUP/WHO classification of flat urothelial lesions is:[1]
- Reactive urothelial atypia.
- Flat urothelial hyperplasia.
- Urothelial atypia of unknown significance.
- Urothelial dysplasia (low-grade dysplasia).
- Urothelial carcinoma in situ (high-grade dysplasia).
- Invasive urothelial carcinoma.
Microscopic
Features:[2]
- Mild nuclear enlargement (~3x a resting lymphocyte) and hyperchromasia.
- Slight disorganization of the architecture.
- Some maturation to the surface - important.
- Mitotic figures - occasional, none atypical.
Notes:
- It is probably not a good idea to make this diagnosis without immunohistochemistry.
- This diagnosis not made on frozen section.
DDx:
- Benign urothelium with reactive changes.
- Urothelial carcinoma in situ - no maturation to the surface or marked atypia - as in pagetoid UCIS and undermining UCIS.[3]
Images
www:
IHC
A comparison between benign, dysplasia and UCIS:[4]
| Diagnosis | CK20 | Ki-67 | p53 | p63 ‡ |
|---|---|---|---|---|
| Benign (reactive) | umbrella cells +ve only | -ve <=10% of cells (+/-rare basal cells) | -ve <20% of cells (+/-weak staining) | -ve surface cells |
| Urothelial dysplasia | +ve non-umbrella cells +ve (~30% of cases) | +ve >10% of cells (~40% of cases) | +ve >=20% of cells (~70% of cases) | -ve surface cells[5][6] |
| Urothelial carcinoma in situ (UCIS) | +ve non-umbrella cells (~70% of cases) | +ve >10% of cells (~95% of cases) | +ve >=20% of cells (~80% of cases) | +ve surface cells[5][6] |
Note:
- ‡ Morphology is considered the gold standard for UCIS versus urothelial dysplasia;[7] however, there is a small literature on p63 for dysplasia versus UCIS that is published in lesser known journals.
Sign out
Urinary Bladder, Biopsy:
- Urothelial dysplasia, see comment.
- Giant cell reaction and chronic inflammation.
Comment:
The urothelium has moderate CK20 staining that extends to the basement membrane. A p53 stain is negative (<10% staining). A Ki-67 stain shows increased staining (marks 20% of urothelium). A p63 stain shows weak/negative surface staining.
Block letters
RIGHT URETER (MARGIN), EXCISION:
- UROTHELIAL DYSPLASIA, SEE COMMENT.
- NEGATIVE FOR UROTHELIAL CARCINOMA.
COMMENT:
There is focal non-umbrella cell CK20 staining, 10% (focal) urothelial
p53 staining, and 30% (focal) urothelial Ki-67 staining. The findings
are that of (low-grade) urothelial dysplasia.
See also
References
- ↑ 1.0 1.1 Hodges, KB.; Lopez-Beltran, A.; Davidson, DD.; Montironi, R.; Cheng, L. (Feb 2010). "Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features.". Hum Pathol 41 (2): 155-62. doi:10.1016/j.humpath.2009.07.002. PMID 19762067.
- ↑ URL: http://pathology.jhu.edu/bladder/image1.cfm?case_number=10&image_number=1. Accessed on: 31 December 2013.
- ↑ McKenney, JK.; Gomez, JA.; Desai, S.; Lee, MW.; Amin, MB. (Mar 2001). "Morphologic expressions of urothelial carcinoma in situ: a detailed evaluation of its histologic patterns with emphasis on carcinoma in situ with microinvasion.". Am J Surg Pathol 25 (3): 356-62. PMID 11224606.
- ↑ Mallofré, C.; Castillo, M.; Morente, V.; Solé, M. (Mar 2003). "Immunohistochemical expression of CK20, p53, and Ki-67 as objective markers of urothelial dysplasia.". Mod Pathol 16 (3): 187-91. doi:10.1097/01.MP.0000056628.38714.5D. PMID 12640096.
- ↑ 5.0 5.1 Stepan, A.; Mărgăritescu, C.; Simionescu, C.; Ciurea, R. (2009). "E-cadherin and p63 immunoexpression in dysplastic lesions and urothelial carcinomas of the bladder.". Rom J Morphol Embryol 50 (3): 461-5. PMID 19690775.
- ↑ 6.0 6.1 Raheem, Sayad A.; Saied, Abdel N.; Al Shaer, Rabee; Mustafa, Osama; Ali, Ali H. (2014). "The Role of CK20, p53 and p63 in Differentiation of Some Urothelial Lesions of Urinary Bladder, Immunohistochemical Study". Open Journal of Pathology (4): 181-193. doi:10.4236/ojpathology.2014.44024.
- ↑ Amin MB, Trpkov K, Lopez-Beltran A, Grignon D (August 2014). "Best practices recommendations in the application of immunohistochemistry in the bladder lesions: report from the International Society of Urologic Pathology consensus conference". Am J Surg Pathol 38 (8): e20–34. doi:10.1097/PAS.0000000000000240. PMID 25029121.