Difference between revisions of "Nodular fasciitis"
Jump to navigation
Jump to search
(tweak) |
|||
| (9 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = Nodular_fasciitis_-_intermed_mag.jpg | | Image = Nodular_fasciitis_-_intermed_mag.jpg | ||
| Width = | | Width = | ||
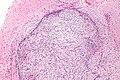
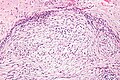
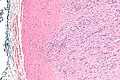
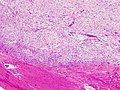
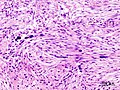
| Caption = Nodular fasciitis. [[H&E stain]]. | | Caption = Nodular fasciitis. [[H&E stain]]. | ||
| Micro = usu. well-circumscribed, clusters of (non-pleomorphic) spindle cells, inflammation (lymphocytes), microcysts in cellular regions - uncommon, mitoses - common, [[extravasated RBC]]s. | | Micro = usu. well-circumscribed, clusters of (non-pleomorphic) spindle cells, inflammation (lymphocytes), microcysts in cellular regions - uncommon, mitoses - common, [[extravasated RBC]]s. | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = | | LMDDx = myxoid [[dermatofibrosarcoma protuberans]], cellular [[dermatofibroma]], [[desmoid-type fibromatosis]], other [[spindle cell lesions of the skin]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = CD34 -ve, desmin -ve, SMA -ve, S-100 -ve, AE1/AE3 -ve. | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = t(15;15) ? | ||
| IF = | | IF = | ||
| Gross = | | Gross = usu. upper extremity ~45% of cases | ||
| Grossing = | | Grossing = | ||
| Site = [[soft tissue lesions|soft tissue]] - [[fibroblastic/myofibroblastic tumours]] | | Site = [[soft tissue lesions|soft tissue]] - [[fibroblastic/myofibroblastic tumours]] | ||
| Line 20: | Line 20: | ||
| Signs = | | Signs = | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = common soft tissue lesion | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = | ||
| Line 28: | Line 28: | ||
| ClinDDx = | | ClinDDx = | ||
}} | }} | ||
'''Nodular fasciitis''' is | '''Nodular fasciitis''' is a benign [[soft tissue lesion]]. | ||
It should '''not''' to be confused with [[necrotizing fasciitis]]. | |||
==General== | |||
*Benign. | *Benign. | ||
*All age groups. | *All age groups - though typically 20-40 years old. | ||
*Associated with trauma. | *Associated with trauma. | ||
*Often rapidily growing - clinically concerning for malignancy.<ref name=pmid14569327>{{Cite journal | last1 = Chi | first1 = CC. | last2 = Kuo | first2 = TT. | last3 = Wang | first3 = SH. | title = Nodular fasciitis: clinical characteristics and preoperative diagnosis. | journal = J Formos Med Assoc | volume = 102 | issue = 8 | pages = 586-9 | month = Aug | year = 2003 | doi = | PMID = 14569327 }}</ref> | |||
*Commonly misdiagnosed as malignant.<ref name=pmid17235006 >{{Cite journal | last1 = Dinauer | first1 = PA. | last2 = Brixey | first2 = CJ. | last3 = Moncur | first3 = JT. | last4 = Fanburg-Smith | first4 = JC. | last5 = Murphey | first5 = MD. | title = Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. | journal = Radiographics | volume = 27 | issue = 1 | pages = 173-87 | month = | year = | doi = 10.1148/rg.271065065 | PMID = 17235006 | URL = http://radiographics.rsna.org/content/27/1/173.long }}</ref> | |||
Subtypes - location:<ref name=pmid17235006/> | |||
*Subcutaneous. | |||
*Intramuscular. | |||
*Fascial | |||
*Dermal - rare. | |||
*Intravascular - rare. | |||
==Gross== | |||
*Usually upper extremity ~45% of cases.<ref name=pmid17235006/> | |||
**Other locations in order: trunk (~20%), head and neck (~20%), and lower extremities (~15%). | |||
==Microscopic== | |||
Features:<ref name=Ref_WMSP606>{{Ref WMSP|606}}</ref><ref>{{cite journal |author=de Feraudy S, Fletcher CD |title=Intradermal nodular fasciitis: a rare lesion analyzed in a series of 24 cases |journal=Am. J. Surg. Pathol. |volume=34 |issue=9 |pages=1377–81 |year=2010 |month=September |pmid=20716998 |doi=10.1097/PAS.0b013e3181ed7374 |url=}}</ref> | Features:<ref name=Ref_WMSP606>{{Ref WMSP|606}}</ref><ref>{{cite journal |author=de Feraudy S, Fletcher CD |title=Intradermal nodular fasciitis: a rare lesion analyzed in a series of 24 cases |journal=Am. J. Surg. Pathol. |volume=34 |issue=9 |pages=1377–81 |year=2010 |month=September |pmid=20716998 |doi=10.1097/PAS.0b013e3181ed7374 |url=}}</ref> | ||
*Usu. well-circumscribed. | *Usu. well-circumscribed. | ||
| Line 56: | Line 71: | ||
DDx:<ref>URL: [http://www.mckeedermpath.com/SPOT%20DIAGNOSIS%20CASE%20268.html http://www.mckeedermpath.com/SPOT%20DIAGNOSIS%20CASE%20268.html]. Accessed on: 11 November 2011.</ref> | DDx:<ref>URL: [http://www.mckeedermpath.com/SPOT%20DIAGNOSIS%20CASE%20268.html http://www.mckeedermpath.com/SPOT%20DIAGNOSIS%20CASE%20268.html]. Accessed on: 11 November 2011.</ref> | ||
*Myxoid [[ | *Myxoid [[dermatofibrosarcoma protuberans]]. | ||
*Cellular [[dermatofibroma]]. | *Cellular [[dermatofibroma]]. | ||
*[[Desmoid-type fibromatosis]]. | *[[Desmoid-type fibromatosis]]. | ||
*Other [[spindle cell lesions of the skin]]. | |||
===Images=== | ===Images=== | ||
| Line 73: | Line 89: | ||
www: | www: | ||
*[http://www.humpath.com/nodular-fasciitis NF (humpath.com)]. | *[http://www.humpath.com/nodular-fasciitis NF (humpath.com)]. | ||
==IHC== | |||
Routine spindle cell panel: | Routine spindle cell panel: | ||
*CD34 -ve. | *CD34 -ve. | ||
*Desmin -ve. | *Desmin -ve. | ||
*SMA - | *SMA +ve -- strong.{{fact}} | ||
* | *S-100 -ve. | ||
*AE1/AE3 -ve. | *AE1/AE3 -ve. | ||
| Line 86: | Line 102: | ||
*Vimentin +ve. | *Vimentin +ve. | ||
==Molecular== | |||
*Evolving - case reports. | *Evolving - case reports. | ||
**t(15;15)(q13;q25).<ref name=pmid12606136>{{cite journal |author=Velagaleti GV, Tapper JK, Panova NE, Miettinen M, Gatalica Z |title=Cytogenetic findings in a case of nodular fasciitis of subclavicular region |journal=Cancer Genet. Cytogenet. |volume=141 |issue=2 |pages=160–3 |year=2003 |month=March |pmid=12606136 |doi= |url=}}</ref> | **t(15;15)(q13;q25).<ref name=pmid12606136>{{cite journal |author=Velagaleti GV, Tapper JK, Panova NE, Miettinen M, Gatalica Z |title=Cytogenetic findings in a case of nodular fasciitis of subclavicular region |journal=Cancer Genet. Cytogenet. |volume=141 |issue=2 |pages=160–3 |year=2003 |month=March |pmid=12606136 |doi= |url=}}</ref> | ||
Latest revision as of 16:17, 18 June 2017
| Nodular fasciitis | |
|---|---|
| Diagnosis in short | |
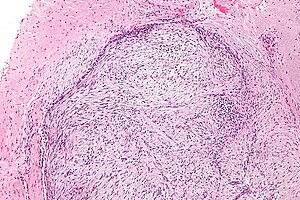 Nodular fasciitis. H&E stain. | |
|
| |
| LM | usu. well-circumscribed, clusters of (non-pleomorphic) spindle cells, inflammation (lymphocytes), microcysts in cellular regions - uncommon, mitoses - common, extravasated RBCs. |
| LM DDx | myxoid dermatofibrosarcoma protuberans, cellular dermatofibroma, desmoid-type fibromatosis, other spindle cell lesions of the skin |
| IHC | CD34 -ve, desmin -ve, SMA -ve, S-100 -ve, AE1/AE3 -ve. |
| Molecular | t(15;15) ? |
| Gross | usu. upper extremity ~45% of cases |
| Site | soft tissue - fibroblastic/myofibroblastic tumours |
|
| |
| Clinical history | associated with trauma |
| Prevalence | common soft tissue lesion |
| Prognosis | benign |
Nodular fasciitis is a benign soft tissue lesion.
It should not to be confused with necrotizing fasciitis.
General
- Benign.
- All age groups - though typically 20-40 years old.
- Associated with trauma.
- Often rapidily growing - clinically concerning for malignancy.[1]
- Commonly misdiagnosed as malignant.[2]
Subtypes - location:[2]
- Subcutaneous.
- Intramuscular.
- Fascial
- Dermal - rare.
- Intravascular - rare.
Gross
- Usually upper extremity ~45% of cases.[2]
- Other locations in order: trunk (~20%), head and neck (~20%), and lower extremities (~15%).
Microscopic
- Usu. well-circumscribed.
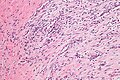
- Clusters of (non-pleomorphic) spindle cells.
- Inflammation (lymphocytes).
- Microcysts in cellular regions - uncommon - discriminatory.
- Mitoses - common.
- Extravasated RBCs.
- Tissue culture-like/CNS-like morphology.
- Thick (keloid-like) collagen bundles - key feature.
- Extravasated RBCs.
- Inflammation.
- +/-Giant cells.
Notes:
- No significant nuclear atypia.
- No atypical mitoses.
- May be cellular.
DDx:[7]
- Myxoid dermatofibrosarcoma protuberans.
- Cellular dermatofibroma.
- Desmoid-type fibromatosis.
- Other spindle cell lesions of the skin.
Images
www:
IHC
Routine spindle cell panel:
- CD34 -ve.
- Desmin -ve.
- SMA +ve -- strong.[citation needed]
- S-100 -ve.
- AE1/AE3 -ve.
Others:
- H-caldesmon -ve.
- EMA -ve.
- Vimentin +ve.
Molecular
- Evolving - case reports.
- t(15;15)(q13;q25).[8]
See also
References
- ↑ Chi, CC.; Kuo, TT.; Wang, SH. (Aug 2003). "Nodular fasciitis: clinical characteristics and preoperative diagnosis.". J Formos Med Assoc 102 (8): 586-9. PMID 14569327.
- ↑ 2.0 2.1 2.2 Dinauer, PA.; Brixey, CJ.; Moncur, JT.; Fanburg-Smith, JC.; Murphey, MD.. "Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults.". Radiographics 27 (1): 173-87. doi:10.1148/rg.271065065. PMID 17235006.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 606. ISBN 978-0781765275.
- ↑ de Feraudy S, Fletcher CD (September 2010). "Intradermal nodular fasciitis: a rare lesion analyzed in a series of 24 cases". Am. J. Surg. Pathol. 34 (9): 1377–81. doi:10.1097/PAS.0b013e3181ed7374. PMID 20716998.
- ↑ Dickson, B. 26 April 2011.
- ↑ URL: http://anvita.info/wiki/Nodular_Fasciitis. Accessed on: 11 November 2011.
- ↑ URL: http://www.mckeedermpath.com/SPOT%20DIAGNOSIS%20CASE%20268.html. Accessed on: 11 November 2011.
- ↑ Velagaleti GV, Tapper JK, Panova NE, Miettinen M, Gatalica Z (March 2003). "Cytogenetic findings in a case of nodular fasciitis of subclavicular region". Cancer Genet. Cytogenet. 141 (2): 160–3. PMID 12606136.