Difference between revisions of "Chronic cholecystitis"
m (tweak) |
|||
| (12 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Chronic cholecystitis and cholesterolosis -- low mag.jpg | ||
| Width = | | Width = | ||
| Caption = | | Caption = Chronic cholecystitis with cholesterolosis. [[H&E stain]]. | ||
| Micro = entrapped epithelial crypts, fibrosis/muscular hypertrophy of gallbladder wall, +/-foamy macrophages | | Micro = entrapped epithelial crypts, fibrosis/muscular hypertrophy of gallbladder wall, +/-foamy macrophages | ||
| Subtypes = | | Subtypes = | ||
| Line 13: | Line 13: | ||
| IF = | | IF = | ||
| Gross = +/-strawberry-like appearance, yellow stones, fibrotic wall | | Gross = +/-strawberry-like appearance, yellow stones, fibrotic wall | ||
| Grossing = | | Grossing = [[gallbladder grossing]] | ||
| Site = [[gallbladder]] | | Site = [[gallbladder]] | ||
| Assdx = [[obesity]] | | Assdx = [[cholelithiasis]], [[gallbladder cholesterolosis]], [[obesity]] | ||
| Syndromes = | | Syndromes = | ||
| Clinicalhx = biliary colic, usu. fertile fat females forty years or less | | Clinicalhx = biliary colic, usu. fertile fat females forty years or less | ||
| Line 39: | Line 39: | ||
===Clinical (classic)=== | ===Clinical (classic)=== | ||
*Constant right upper quadrant pain after a fatty meal. | *Constant right upper quadrant pain after a fatty meal (biliary colic). | ||
*Positive Murphy's sign (physical exam, with ultrasound). | *Positive Murphy's sign (physical exam, with ultrasound). | ||
| Line 64: | Line 64: | ||
DDx: | DDx: | ||
*[[Gallbladder cholesterolosis]] and chronic cholecystitis. | |||
*[[Gallbladder adenomyoma]]. | *[[Gallbladder adenomyoma]]. | ||
*[[Acute cholecystitis]] - more inflammation, lack Rokitansky-Aschoff sinuses, +/-mucosal erosions. | *[[Acute cholecystitis]] - more inflammation, lack Rokitansky-Aschoff sinuses, +/-mucosal erosions. | ||
| Line 69: | Line 70: | ||
*[[Intestinal metaplasia of the gallbladder]] - goblet cells present, may be focal. | *[[Intestinal metaplasia of the gallbladder]] - goblet cells present, may be focal. | ||
*[[Gallbladder adenocarcinoma]]. | *[[Gallbladder adenocarcinoma]]. | ||
===Images=== | |||
<gallery> | |||
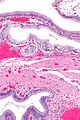
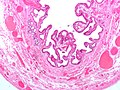
Image: Chronic cholecystitis and cholesterolosis -- intermed mag.jpg | CC - intermed. mag. (WC) | |||
Image:Gallbladder_cholesterolosis_micro.jpg | Cholesterolosis. (WC) | |||
</gallery> | |||
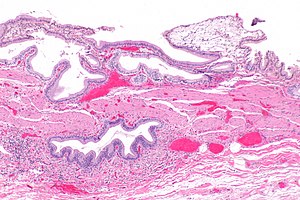
[[File:Reactive change in cholecystitis A sl 1.png| Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman]] | |||
[[File:Reactive change in cholecystitis A sl 2.png| Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman]] | |||
[[File:Reactive change in cholecystitis A sl 3.png| Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman]] | |||
[[File:Reactive change in cholecystitis A sl 4.png| Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman]]<br> | |||
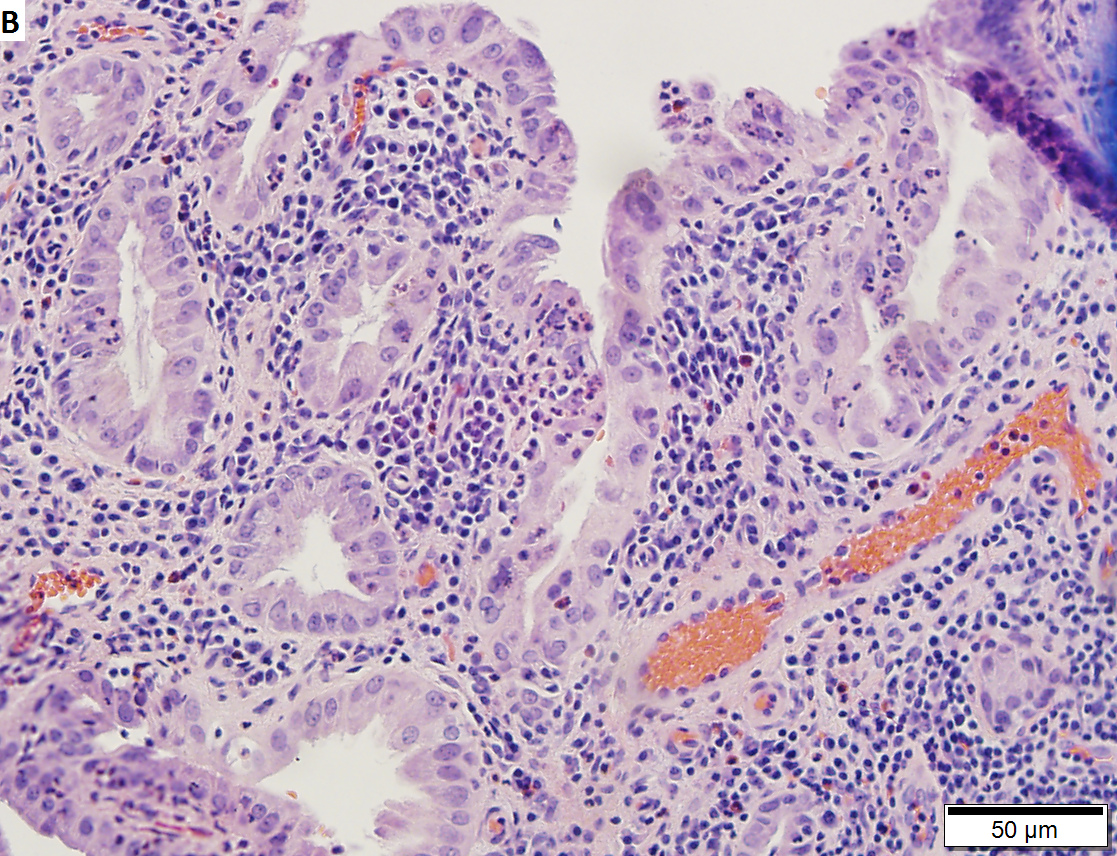
Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman. A. Extending from a benign, chronically inflamed plicae are Rikitansky-Aschoff sinuses. Note their travel in between muscle bundles can be recognized as continuity to the surface. B. In between the gall stone at lower left and the lymphoid aggregate at upper right lies the gallbladder wall. Note the longitudinal extensions of the Rokitansky-Aschoff sinuses, as well as the ballooning outside the wall at lower right. C. The mucosa shows extensive reactive branching. Note again the predominant extension between muscle bundles, recognizable by the stroma about the sinuses, some of which are branched, pushing the muscle wall aside. There is no desmoplasia, but some gallbladder adenocarcinomas show little recognizable desmoplasia. D. The focus on the right is difficult to identify as lying between muscle bundles. The triple parallel tubules argue against neoplasia. The lack of cancerous nuclear change is important as well. | |||
[[File:5gb41630891386282 sl 1.png| Chronic cholecystitis with reactive changes.]] | |||
[[File:5gb41630891386282 sl 2.png| Chronic cholecystitis with reactive changes.]] | |||
[[File:5gb41630891386282 sl 3.png| Chronic cholecystitis with reactive changes.]] | |||
[[File:5gb41630891386282 sl 4.png| Chronic cholecystitis with reactive changes.]]<br> | |||
Chronic cholecystitis with reactive epithelial atypia in a 92 year old. A. Lymphoid follicles are associated with chronically inflamed plicae. B. Neutrophils lie within cytoplasm of epithelium. Nuclei show variability in size and, to a lesser degree, shape. Some cells are multinucleated. Polarity is generally, but not always, preserved, with most nuclei at the base of the cell, with the longer nuclear dimension, when the nucleus is not round, being perpendicular to the luminal surface. C. Monoclonal CEA stains neutrophils, but not epithelial cells. D. CD10 stains the luminal surfaces of epithelial cells, a finding that militates against dysplasia. | |||
==Sign out== | ==Sign out== | ||
<pre> | |||
Gallbladder, Cholecystectomy: | |||
- Cholelithiasis. | |||
- Chronic cholecystitis, mild. | |||
- One benign lymph node. | |||
</pre> | |||
====Block letters==== | |||
<pre> | <pre> | ||
GALLBLADDER, CHOLECYSTECTOMY: | GALLBLADDER, CHOLECYSTECTOMY: | ||
- CHRONIC CHOLECYSTITIS. | - CHRONIC CHOLECYSTITIS. | ||
- CHOLELITHIASIS. | - CHOLELITHIASIS. | ||
</pre> | |||
===Without stones=== | |||
<pre> | |||
GALLBLADDER, CHOLECYSTECTOMY: | |||
- CHRONIC CHOLECYSTITIS. | |||
- NO GALLSTONES IDENTIFIED. | |||
</pre> | </pre> | ||
| Line 83: | Line 116: | ||
- CHOLELITHIASIS. | - CHOLELITHIASIS. | ||
- SMALL AMOUNT OF LIVER WITHOUT APPARENT PATHOLOGY. | - SMALL AMOUNT OF LIVER WITHOUT APPARENT PATHOLOGY. | ||
</pre> | |||
<pre> | |||
GALLBLADDER, CHOLECYSTECTOMY: | |||
- CHRONIC CHOLECYSTITIS WITH MILD CHOLESTEROLOSIS. | |||
- CHOLELITHIASIS. | |||
- SMALL AMOUNT OF LIVER WITH CAUTERY/CRUSH ARTIFACT. | |||
</pre> | </pre> | ||
| Line 88: | Line 128: | ||
The sections shows gallbladder wall with Rokitansky-Aschoff sinuses and a moderate mixed | The sections shows gallbladder wall with Rokitansky-Aschoff sinuses and a moderate mixed | ||
inflammatory infiltrate predominantly consisting of lymphocytes. No nuclear atypia is seen. | inflammatory infiltrate predominantly consisting of lymphocytes. No nuclear atypia is seen. | ||
====Post-cholecystostomy tube==== | |||
The sections shows gallbladder wall with edema, a moderate mixed inflammatory infiltrate | |||
(predominantly consisting of lymphocytes and plasma cells), and mucosal erosions. Reactive | |||
fibroblasts and hemosiderin-laden macrophages are present. No significant nuclear changes | |||
are seen. One benign lymph node is present. | |||
==See also== | ==See also== | ||
Latest revision as of 14:43, 15 August 2024
| Chronic cholecystitis | |
|---|---|
| Diagnosis in short | |
 Chronic cholecystitis with cholesterolosis. H&E stain. | |
|
| |
| LM | entrapped epithelial crypts, fibrosis/muscular hypertrophy of gallbladder wall, +/-foamy macrophages |
| LM DDx | acute cholecystitis, gallbladder adenocarcinoma, gallbladder adenomyoma, intestinal metaplasia of the gallbladder |
| Gross | +/-strawberry-like appearance, yellow stones, fibrotic wall |
| Grossing notes | gallbladder grossing |
| Site | gallbladder |
|
| |
| Associated Dx | cholelithiasis, gallbladder cholesterolosis, obesity |
| Clinical history | biliary colic, usu. fertile fat females forty years or less |
| Symptoms | constant right upper quadrant pain after a meal (biliary colic) |
| Prevalence | very common |
| Prognosis | good, benign |
Chronic cholecystitis, abbreviated CC, is a very common pathology of the gallbladder and increasing in prevalence with the expanding waist lines.
General
Epidemiology
- Female, fat, fertile, family history, forty (though now getting younger... as people get fatter).
Etiology
- Cholelithiasis.
- Thick bile (acalculous cholecystitis).
Clinical (classic)
- Constant right upper quadrant pain after a fatty meal (biliary colic).
- Positive Murphy's sign (physical exam, with ultrasound).
Gross
- +/-Cholelithiasis - strongly associated pathology.
- +/-Strawberry-like appearance - common (due to gallbladder cholesterolosis).
- Small ridges (microvillus architecture) + yellow.
- Normal gallbladder mucosa = smooth, green.
- Small ridges (microvillus architecture) + yellow.
- +/-Congestion/erythema.
- +/-Wall thickening - typically ~ 6-7 mm.[1]
Note:
- Wall thickening (due to congestion/edema) is the important gross finding in acute cholecystitis.
- Wall thickenss greater than 10 mm should raise the suspicion of malignancy.[1]
Microscopic
Features:[2]
- Thickening of the gallbladder wall - due to fibrosis/muscular hypertrophy - key feature.
- Chronic inflammatory cells - usu. "minimal".
- Lymphocytes - most common.
- Rokitansky-Aschoff sinuses - common.[3]
- Entrapped epithelial crypts -- pockets of epithelium in the wall of the gallbladder.
- +/-Foamy macrophages in the lamina propria (cholesterolosis of the gallbladder).
DDx:
- Gallbladder cholesterolosis and chronic cholecystitis.
- Gallbladder adenomyoma.
- Acute cholecystitis - more inflammation, lack Rokitansky-Aschoff sinuses, +/-mucosal erosions.
- Cholecystectomy for gallstone pancreatitis - intraepithelial neutrophil clusters common, history essential.
- Intestinal metaplasia of the gallbladder - goblet cells present, may be focal.
- Gallbladder adenocarcinoma.
Images

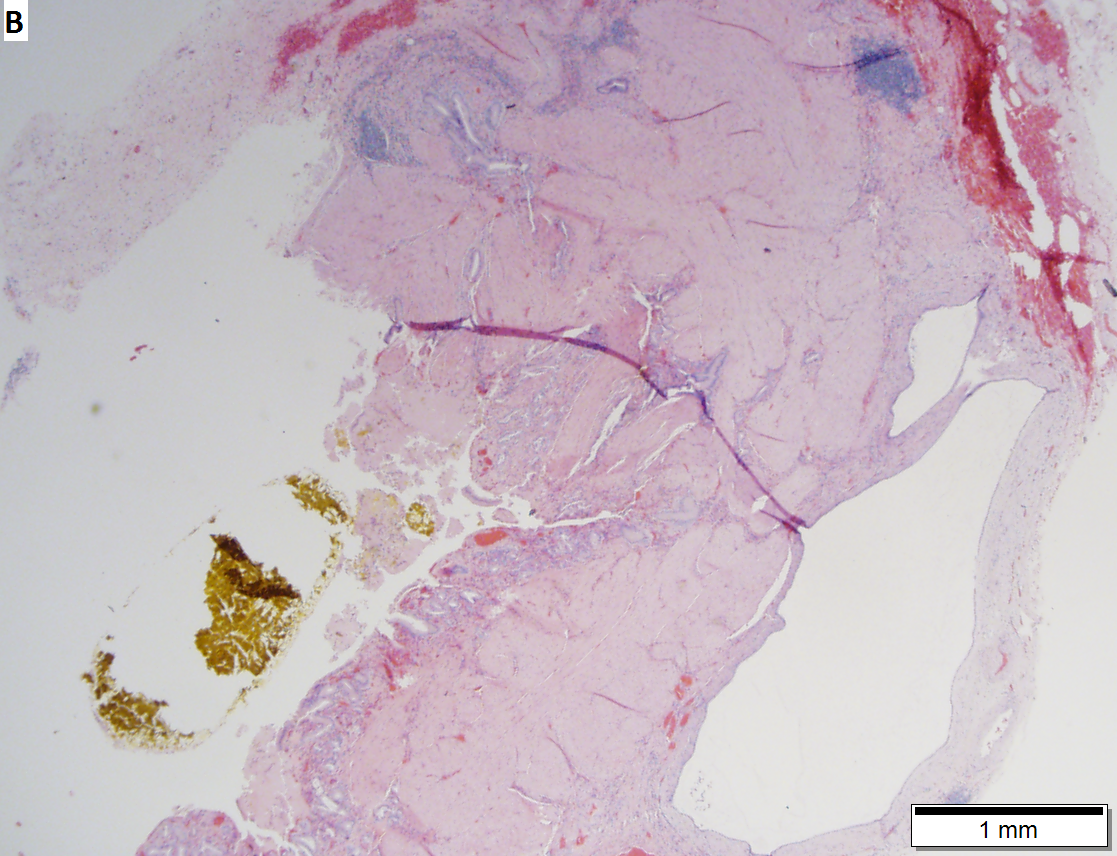


Extensive Rokitansky-Aschoff sinuses in a 64 year ood woman. A. Extending from a benign, chronically inflamed plicae are Rikitansky-Aschoff sinuses. Note their travel in between muscle bundles can be recognized as continuity to the surface. B. In between the gall stone at lower left and the lymphoid aggregate at upper right lies the gallbladder wall. Note the longitudinal extensions of the Rokitansky-Aschoff sinuses, as well as the ballooning outside the wall at lower right. C. The mucosa shows extensive reactive branching. Note again the predominant extension between muscle bundles, recognizable by the stroma about the sinuses, some of which are branched, pushing the muscle wall aside. There is no desmoplasia, but some gallbladder adenocarcinomas show little recognizable desmoplasia. D. The focus on the right is difficult to identify as lying between muscle bundles. The triple parallel tubules argue against neoplasia. The lack of cancerous nuclear change is important as well.

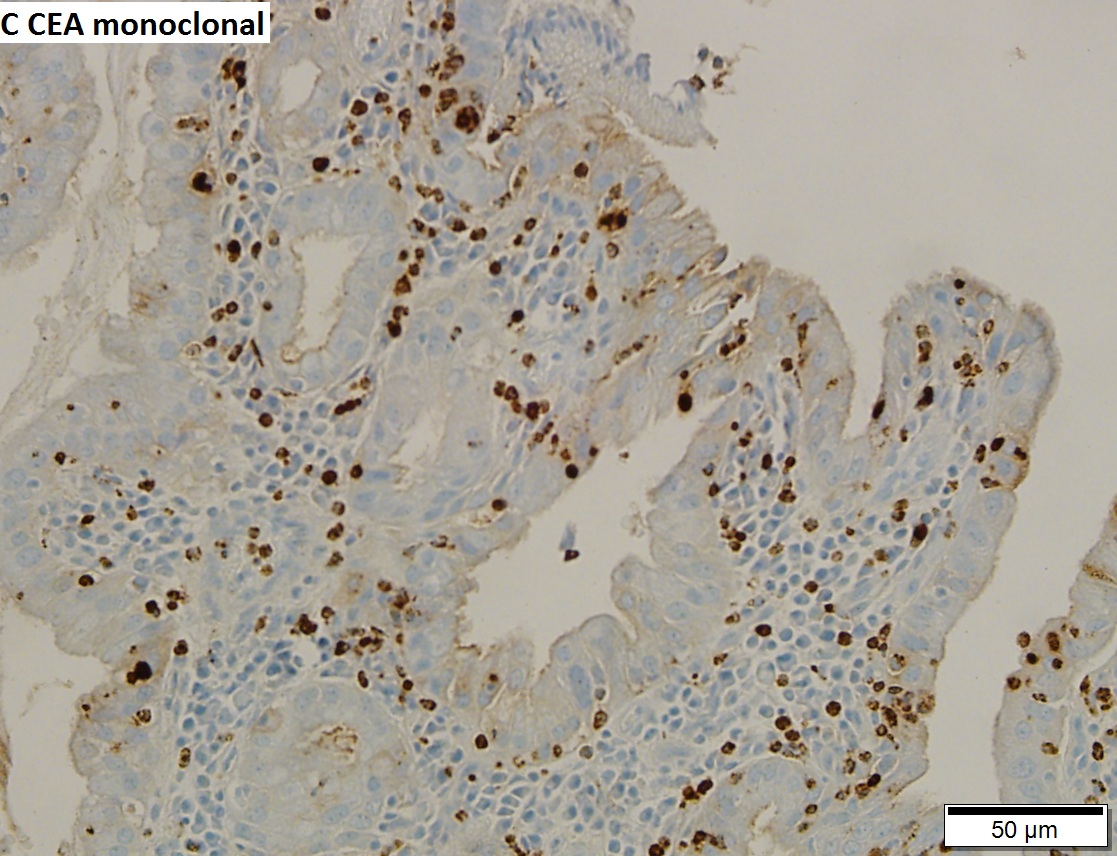

Chronic cholecystitis with reactive epithelial atypia in a 92 year old. A. Lymphoid follicles are associated with chronically inflamed plicae. B. Neutrophils lie within cytoplasm of epithelium. Nuclei show variability in size and, to a lesser degree, shape. Some cells are multinucleated. Polarity is generally, but not always, preserved, with most nuclei at the base of the cell, with the longer nuclear dimension, when the nucleus is not round, being perpendicular to the luminal surface. C. Monoclonal CEA stains neutrophils, but not epithelial cells. D. CD10 stains the luminal surfaces of epithelial cells, a finding that militates against dysplasia.
Sign out
Gallbladder, Cholecystectomy: - Cholelithiasis. - Chronic cholecystitis, mild. - One benign lymph node.
Block letters
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS. - CHOLELITHIASIS.
Without stones
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS. - NO GALLSTONES IDENTIFIED.
Liver present
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS. - CHOLELITHIASIS. - SMALL AMOUNT OF LIVER WITHOUT APPARENT PATHOLOGY.
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH MILD CHOLESTEROLOSIS. - CHOLELITHIASIS. - SMALL AMOUNT OF LIVER WITH CAUTERY/CRUSH ARTIFACT.
Micro
The sections shows gallbladder wall with Rokitansky-Aschoff sinuses and a moderate mixed inflammatory infiltrate predominantly consisting of lymphocytes. No nuclear atypia is seen.
Post-cholecystostomy tube
The sections shows gallbladder wall with edema, a moderate mixed inflammatory infiltrate (predominantly consisting of lymphocytes and plasma cells), and mucosal erosions. Reactive fibroblasts and hemosiderin-laden macrophages are present. No significant nuclear changes are seen. One benign lymph node is present.
See also
References
- ↑ 1.0 1.1 Kim, HJ.; Park, JH.; Park, DI.; Cho, YK.; Sohn, CI.; Jeon, WK.; Kim, BI.; Choi, SH. (Feb 2012). "Clinical usefulness of endoscopic ultrasonography in the differential diagnosis of gallbladder wall thickening.". Dig Dis Sci 57 (2): 508-15. doi:10.1007/s10620-011-1870-0. PMID 21879282.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 439. ISBN 978-0443066573.
- ↑ URL: http://www.whonamedit.com/synd.cfm/983.html. Accessed on: 29 October 2011.