Difference between revisions of "Follicular lymphoma"
Jump to navigation
Jump to search
(redirect) |
(→IHC) |
||
| (18 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Follicular lymphoma -- low mag.jpg | |||
| Width = | |||
| Caption = Follicular lymphoma. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = Lymph node: abundant abnormally-shaped lymphoid follicles with some of the following: non-polarized mantle zone, non-polarized germinal center, loss of tingible body macrophages, sinuses effaced (lost) | |||
| Subtypes = | |||
| LMDDx = [[diffuse large B-cell lymphoma]], other [[small cell lymphomas]], reactive follicular hyperplasia | |||
| Stains = | |||
| IHC = CD20 +ve, CD10 +ve, BCL-6 +ve, BCL-2 +ve | |||
| EM = | |||
| Molecular = t(14;18)(q32;q21) / IGH-BCL2 | |||
| IF = | |||
| Gross = white lesions +/-subtle fine nodularity (fish flesh-like appearance) | |||
| Grossing = | |||
| Site = [[lymph node]], [[spleen]], [[bone marrow]], others | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = common | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = moderate to good | |||
| Other = | |||
| ClinDDx = other causes of lymphadenopathy - other [[lymphoma]]s, metastatic carcinoma | |||
| Tx = | |||
}} | |||
'''Follicular lymphoma''', abbreviated '''FL''', is a very common [[non-Hodgkin lymphoma]]. It is a [[small cell lymphoma]]. | |||
==General== | |||
*A very common type of lymphoma. | |||
*Moderate prognosis - overall five year survival ~ 66% in one cohort without transformation.<ref name=pmid23897955>{{Cite journal | last1 = Link | first1 = BK. | last2 = Maurer | first2 = MJ. | last3 = Nowakowski | first3 = GS. | last4 = Ansell | first4 = SM. | last5 = Macon | first5 = WR. | last6 = Syrbu | first6 = SI. | last7 = Slager | first7 = SL. | last8 = Thompson | first8 = CA. | last9 = Inwards | first9 = DJ. | title = Rates and outcomes of follicular lymphoma transformation in the immunochemotherapy era: a report from the University of Iowa/MayoClinic Specialized Program of Research Excellence Molecular Epidemiology Resource. | journal = J Clin Oncol | volume = 31 | issue = 26 | pages = 3272-8 | month = Sep | year = 2013 | doi = 10.1200/JCO.2012.48.3990 | PMID = 23897955 }} | |||
</ref> | |||
*May transform to a more aggressive lymphoma, e.g. [[diffuse large B-cell lymphoma]]. | |||
**Prognosis after transformation significantly worse - five year survival ~ 22%.<ref name=pmid23897955/> | |||
**Approximately 2% transform per year, or 10.7% in five years.<ref name=pmid23897955/> | |||
==Gross== | |||
*Lymph node enlargement. | |||
*Classically white and uniform - usually described as ''fish flesh-like''. | |||
**May have a vague nodularity. | |||
===Images=== | |||
<gallery> | |||
Image:Lymphoma_macro.jpg | FL in a lymph node. (WC) | |||
Image:Follicular_lymphoma,_spleen.jpg | FL in the [[spleen]]. (WC) | |||
</gallery> | |||
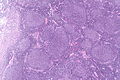
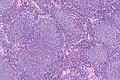
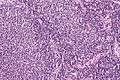
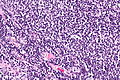
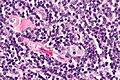
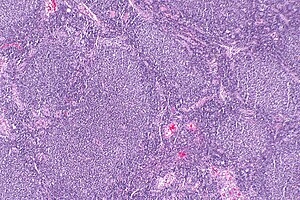
==Microscopic== | |||
Features (lymph node): | |||
*Abundant abnormally-shaped lymphoid follicles - '''key feature''' - including some of the following: | |||
**Non-polarized mantle zone (normal mantle zone is usu. thicker at capsular aspect). | |||
**Non-polarized germinal center (normal germinal center has dark & light area). | |||
**Loss of tingible body macrophages. | |||
**Sinuses effaced (lost). | |||
Note: | |||
*The intrafollicular component of the lymph node is compressed - follicles are often described as "kissing", as they nearly touch. | |||
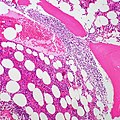
*In [[bone marrow]] specimens the neoplastic cells classically have a paratrabecular arrangement,<ref name=pmid17284114>{{Cite journal | last1 = Iancu | first1 = D. | last2 = Hao | first2 = S. | last3 = Lin | first3 = P. | last4 = Anderson | first4 = SK. | last5 = Jorgensen | first5 = JL. | last6 = McLaughlin | first6 = P. | last7 = Medeiros | first7 = LJ. | title = Follicular lymphoma in staging bone marrow specimens: correlation of histologic findings with the results of flow cytometry immunophenotypic analysis. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 282-7 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[282:FLISBM]2.0.CO;2 | PMID = 17284114 }}</ref> i.e. the lymphoma cells are found adjacent to the bone spicules. | |||
DDx: | |||
*Reactive follicular hyperplasia. | |||
*[[Diffuse large B-cell lymphoma]] - esp. for the grade 3B. | |||
===Images=== | |||
<gallery> | |||
Image: Follicular lymphoma -- very low mag.jpg | FL - very low mag. | |||
Image: Follicular lymphoma -- low mag.jpg | FL - low mag. | |||
Image: Follicular lymphoma -- intermed mag.jpg | FL - intermed. mag. | |||
Image: Follicular lymphoma -- high mag.jpg | FL - high mag. | |||
Image: Follicular lymphoma -- very high mag.jpg | FL - very high mag. | |||
</gallery> | |||
<gallery> | |||
Image:Follicular_Lymphoma,_Paratrabecular_Involvement_of_Bone_Marrow_(5691578596).jpg | FL - bone marrow. (WC/euthman) | |||
</gallery> | |||
www: | |||
*[http://www.flickr.com/photos/euthman/3311641845/ Follicular lymphoma - bone marrow (flickr.com)]. | |||
*[http://library.med.utah.edu/WebPath/HEMEHTML/HEME034.html Follicular lymphoma (utah.edu)]. | |||
===Grading=== | |||
*Grade 1-2: <= 22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective). | |||
*Grade 3A: >22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective). | |||
*Grade 3B: only centroblasts (within a nodular architecture). | |||
Notes: | |||
*Significant interobserver variability.<ref>Good, D. 17 August 2010.</ref> | |||
*Grade 1 & Grade 2 lumped together. | |||
*One should evaluate 10 HPFs. | |||
*''Only'' centroblasts ''without'' a nodular architecture is ''[[Diffuse large B cell lymphoma]]'' ([[DLBCL]]). | |||
The usual cut points mentioned by people with [[HPFitis]] are:<ref name=Ref_Sternberg4_813>{{Ref Sternberg4|813}}</ref> | |||
*Grade 1: 0-5 centroblasts / HPF. | |||
*Grade 2: 5-15 centroblasts / HPF. | |||
*Grade 3: >15 centroblasts / HPF. | |||
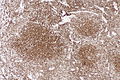
==IHC== | |||
Features:<ref name=pmid18359244/> | |||
*[[CD10]] +ve. | |||
*BCL6 +ve. | |||
Others: | |||
*CD5 -ve. | |||
**+ve in mantle cell lymphoma. | |||
*CD23 -ve/+ve. | |||
**+ve in CLL. | |||
*CD43 -ve. | |||
**+ve in mantle cell lymphoma, marginal zone lymphoma. | |||
*CD11c -ve -- flow cytometry only. | |||
*CD21 -ve in tumour cells; highlights follicular dendritic cells. | |||
*BCL2 +ve<ref name=pmid18359244>{{cite journal |author=Vitolo U, Ferreri AJ, Montoto S |title=Follicular lymphomas |journal=Crit. Rev. Oncol. Hematol. |volume=66 |issue=3 |pages=248–61 |year=2008 |month=June |pmid=18359244 |doi=10.1016/j.critrevonc.2008.01.014 |url=}}</ref> - like many other small cell lymphomas. | |||
**Usually negative in benign germinal centres. | |||
A panel to work-up: | |||
*BCL2, BCL6, CD3, CD5, CD10, CD20, CD23, cyclin D1. | |||
===Images=== | |||
<gallery> | |||
Image: Follicluar lymphoma - bcl2 -- low mag.jpg | FL - BCL2 - low mag. | |||
Image: Follicular lymphoma - control bcl2 -- low mag.jpg | FL - BCL2 control - low mag. | |||
</gallery> | |||
www: | |||
*[http://www.pathpedia.com/education/eatlas/histopathology/lymph_node/follicular_lymphoma/follicular-lymphoma-%5B16-ln021_cd21%5D.jpeg Follicular lymphoma - CD21 (pathpedia.com)]. | |||
==Molecular== | |||
*t(14;18)(q32;q21)/IGH-BCL2 in 70-95% of cases.<ref name=pmid18359244/> | |||
**Should not be confused with t(14;18)(q32;q21)/IGH-MALT1 seen in MALT lymphomas.<ref name=pmid16950858>{{cite journal |author=Bacon CM, Du MQ, Dogan A |title=Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists |journal=J. Clin. Pathol. |volume=60 |issue=4 |pages=361–72 |year=2007 |month=April |pmid=16950858 |pmc=2001121 |doi=10.1136/jcp.2005.031146 |url=}}</ref> | |||
==Sign out== | |||
<pre> | |||
RETROPERITONEAL MASS, RIGHT, CORE BIOPSIES: | |||
- NON-HODGKIN B-CELL LYMPHOMA, FAVOUR FOLLICULAR LYMPHOMA. | |||
COMMENT: | |||
Morphology: | |||
-Small cells: size ~ mature lymphocytes, quantity - many, angular and round. | |||
-Large cells (intermixed with small cells): size ~1.5-2x mature lymphocyte, | |||
small nucleoli, moderate quantity of grey/basophilic cytoplasm, moderate | |||
nuclear pleomorphism. | |||
-Architecture: no gland formation, discohesive, no follicles apparent, no sheets | |||
of large cells. | |||
-Mitoses are uncommon. | |||
Immunohistochemical stains (tumour cells): | |||
Positive: CD45 (strong, membranous/cytoplasmic), CD20 (strong, membranous/cytoplasmic), | |||
BCL-2 (strong, membranous/cytoplasmic), CD10 (strong, membranous), BCL-6 (moderate, | |||
patchy, nuclear). | |||
Negative: pankeratin, CD3, CD5, CD30, CD21 (follicular dendritic cells not apparent), | |||
CD23 (scattered, rare). | |||
Ki-67: highlights the large cells, primarily -- 5-35% of cells within the core. | |||
The findings favour a follicular lymphoma, based on the cellular morphology and | |||
immunostains; however, they are limited by the type of tissue sampling (core biopsy). | |||
Clinical correlation is suggested. | |||
</pre> | |||
==See also== | |||
*[[Small cell lymphomas]]. | |||
*[[Lymphoma]]. | |||
*[[Lymph node pathology]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | |||
[[Category:Small cell lymphomas]] | |||
Latest revision as of 17:34, 20 March 2015
| Follicular lymphoma | |
|---|---|
| Diagnosis in short | |
 Follicular lymphoma. H&E stain. | |
|
| |
| LM | Lymph node: abundant abnormally-shaped lymphoid follicles with some of the following: non-polarized mantle zone, non-polarized germinal center, loss of tingible body macrophages, sinuses effaced (lost) |
| LM DDx | diffuse large B-cell lymphoma, other small cell lymphomas, reactive follicular hyperplasia |
| IHC | CD20 +ve, CD10 +ve, BCL-6 +ve, BCL-2 +ve |
| Molecular | t(14;18)(q32;q21) / IGH-BCL2 |
| Gross | white lesions +/-subtle fine nodularity (fish flesh-like appearance) |
| Site | lymph node, spleen, bone marrow, others |
|
| |
| Prevalence | common |
| Prognosis | moderate to good |
| Clin. DDx | other causes of lymphadenopathy - other lymphomas, metastatic carcinoma |
Follicular lymphoma, abbreviated FL, is a very common non-Hodgkin lymphoma. It is a small cell lymphoma.
General
- A very common type of lymphoma.
- Moderate prognosis - overall five year survival ~ 66% in one cohort without transformation.[1]
- May transform to a more aggressive lymphoma, e.g. diffuse large B-cell lymphoma.
Gross
- Lymph node enlargement.
- Classically white and uniform - usually described as fish flesh-like.
- May have a vague nodularity.
Images
FL in the spleen. (WC)
Microscopic
Features (lymph node):
- Abundant abnormally-shaped lymphoid follicles - key feature - including some of the following:
- Non-polarized mantle zone (normal mantle zone is usu. thicker at capsular aspect).
- Non-polarized germinal center (normal germinal center has dark & light area).
- Loss of tingible body macrophages.
- Sinuses effaced (lost).
Note:
- The intrafollicular component of the lymph node is compressed - follicles are often described as "kissing", as they nearly touch.
- In bone marrow specimens the neoplastic cells classically have a paratrabecular arrangement,[2] i.e. the lymphoma cells are found adjacent to the bone spicules.
DDx:
- Reactive follicular hyperplasia.
- Diffuse large B-cell lymphoma - esp. for the grade 3B.
Images
www:
Grading
- Grade 1-2: <= 22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective).
- Grade 3A: >22 centroblasts / HPF; where 1 HPF ~= 0.2376 mm^2 (22 mm eye piece @ 40X objective).
- Grade 3B: only centroblasts (within a nodular architecture).
Notes:
- Significant interobserver variability.[3]
- Grade 1 & Grade 2 lumped together.
- One should evaluate 10 HPFs.
- Only centroblasts without a nodular architecture is Diffuse large B cell lymphoma (DLBCL).
The usual cut points mentioned by people with HPFitis are:[4]
- Grade 1: 0-5 centroblasts / HPF.
- Grade 2: 5-15 centroblasts / HPF.
- Grade 3: >15 centroblasts / HPF.
IHC
Features:[5]
- CD10 +ve.
- BCL6 +ve.
Others:
- CD5 -ve.
- +ve in mantle cell lymphoma.
- CD23 -ve/+ve.
- +ve in CLL.
- CD43 -ve.
- +ve in mantle cell lymphoma, marginal zone lymphoma.
- CD11c -ve -- flow cytometry only.
- CD21 -ve in tumour cells; highlights follicular dendritic cells.
- BCL2 +ve[5] - like many other small cell lymphomas.
- Usually negative in benign germinal centres.
A panel to work-up:
- BCL2, BCL6, CD3, CD5, CD10, CD20, CD23, cyclin D1.
Images
www:
Molecular
- t(14;18)(q32;q21)/IGH-BCL2 in 70-95% of cases.[5]
- Should not be confused with t(14;18)(q32;q21)/IGH-MALT1 seen in MALT lymphomas.[6]
Sign out
RETROPERITONEAL MASS, RIGHT, CORE BIOPSIES: - NON-HODGKIN B-CELL LYMPHOMA, FAVOUR FOLLICULAR LYMPHOMA. COMMENT: Morphology: -Small cells: size ~ mature lymphocytes, quantity - many, angular and round. -Large cells (intermixed with small cells): size ~1.5-2x mature lymphocyte, small nucleoli, moderate quantity of grey/basophilic cytoplasm, moderate nuclear pleomorphism. -Architecture: no gland formation, discohesive, no follicles apparent, no sheets of large cells. -Mitoses are uncommon. Immunohistochemical stains (tumour cells): Positive: CD45 (strong, membranous/cytoplasmic), CD20 (strong, membranous/cytoplasmic), BCL-2 (strong, membranous/cytoplasmic), CD10 (strong, membranous), BCL-6 (moderate, patchy, nuclear). Negative: pankeratin, CD3, CD5, CD30, CD21 (follicular dendritic cells not apparent), CD23 (scattered, rare). Ki-67: highlights the large cells, primarily -- 5-35% of cells within the core. The findings favour a follicular lymphoma, based on the cellular morphology and immunostains; however, they are limited by the type of tissue sampling (core biopsy). Clinical correlation is suggested.
See also
References
- ↑ 1.0 1.1 1.2 Link, BK.; Maurer, MJ.; Nowakowski, GS.; Ansell, SM.; Macon, WR.; Syrbu, SI.; Slager, SL.; Thompson, CA. et al. (Sep 2013). "Rates and outcomes of follicular lymphoma transformation in the immunochemotherapy era: a report from the University of Iowa/MayoClinic Specialized Program of Research Excellence Molecular Epidemiology Resource.". J Clin Oncol 31 (26): 3272-8. doi:10.1200/JCO.2012.48.3990. PMID 23897955.
- ↑ Iancu, D.; Hao, S.; Lin, P.; Anderson, SK.; Jorgensen, JL.; McLaughlin, P.; Medeiros, LJ. (Feb 2007). "Follicular lymphoma in staging bone marrow specimens: correlation of histologic findings with the results of flow cytometry immunophenotypic analysis.". Arch Pathol Lab Med 131 (2): 282-7. doi:10.1043/1543-2165(2007)131[282:FLISBM]2.0.CO;2. PMID 17284114.
- ↑ Good, D. 17 August 2010.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 813. ISBN 978-0781740517.
- ↑ 5.0 5.1 5.2 Vitolo U, Ferreri AJ, Montoto S (June 2008). "Follicular lymphomas". Crit. Rev. Oncol. Hematol. 66 (3): 248–61. doi:10.1016/j.critrevonc.2008.01.014. PMID 18359244.
- ↑ Bacon CM, Du MQ, Dogan A (April 2007). "Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists". J. Clin. Pathol. 60 (4): 361–72. doi:10.1136/jcp.2005.031146. PMC 2001121. PMID 16950858. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2001121/.