Difference between revisions of "Prostate-specific antigen"
Jump to navigation
Jump to search
m (vauthors) |
|||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 7: | Line 7: | ||
===Serum PSA=== | ===Serum PSA=== | ||
*Normal - typically <= 4.0 ng/ | *Normal - typically <= 4.0 ng/ml. | ||
**[[Sensitivity]]: 82% (whites), 90% (blacks).<ref name=pmid8998182>{{Cite journal | last1 = Henderson | first1 = RJ. | last2 = Eastham | first2 = JA. | last3 = Culkin | first3 = DJ. | last4 = Kattan | first4 = MW. | last5 = Whatley | first5 = T. | last6 = Mata | first6 = J. | last7 = Venable | first7 = D. | last8 = Sartor | first8 = O. | title = Prostate-specific antigen (PSA) and PSA density: racial differences in men without prostate cancer. | journal = J Natl Cancer Inst | volume = 89 | issue = 2 | pages = 134-8 | month = Jan | year = 1997 | doi = | PMID = 8998182 }} | **[[Sensitivity]]: 82% (whites), 90% (blacks).<ref name=pmid8998182>{{Cite journal | last1 = Henderson | first1 = RJ. | last2 = Eastham | first2 = JA. | last3 = Culkin | first3 = DJ. | last4 = Kattan | first4 = MW. | last5 = Whatley | first5 = T. | last6 = Mata | first6 = J. | last7 = Venable | first7 = D. | last8 = Sartor | first8 = O. | title = Prostate-specific antigen (PSA) and PSA density: racial differences in men without prostate cancer. | journal = J Natl Cancer Inst | volume = 89 | issue = 2 | pages = 134-8 | month = Jan | year = 1997 | doi = | PMID = 8998182 }} | ||
</ref> | </ref> | ||
| Line 14: | Line 14: | ||
Age-normal: | Age-normal: | ||
*40s - 2.5. | *40s - 2.5 ng/ml. | ||
*50s - 3.5. | *50s - 3.5 ng/ml. | ||
*60s - 4.5. | *60s - 4.5 ng/ml. | ||
*70s - 6.5. | *70s - 6.5 ng/ml. | ||
====Prostate specific antigen density==== | |||
Note: | |||
*The units for PSA may also be μg/L; note that 1 μg/L = 1 ng/ml. | |||
====Prostate-specific antigen density==== | |||
:Abbreviated ''PSAD''. | :Abbreviated ''PSAD''. | ||
Normal is often considered to be: <0.15 ng/ml. | Normal is often considered to be: <0.15 ng/ml<sup>2</sup>. | ||
*Approximately 8% of individuals below the cut-point (0.15 ng/ml) have medium or high-grade cancer.<ref name=pmid12973074>{{Cite journal | last1 = Boulos | first1 = MT. | last2 = Rifkin | first2 = MD. | last3 = Ross | first3 = J. | title = Should prostate-specific antigen or prostate-specific antigen density be used as the determining factor when deciding which prostates should undergo biopsy during prostate ultrasound. | journal = Ultrasound Q | volume = 17 | issue = 3 | pages = 177-80 | month = Sep | year = 2001 | doi = | PMID = 12973074 }} | *Approximately 8% of individuals below the cut-point (0.15 ng/ml) have medium or high-grade cancer.<ref name=pmid12973074>{{Cite journal | last1 = Boulos | first1 = MT. | last2 = Rifkin | first2 = MD. | last3 = Ross | first3 = J. | title = Should prostate-specific antigen or prostate-specific antigen density be used as the determining factor when deciding which prostates should undergo biopsy during prostate ultrasound. | journal = Ultrasound Q | volume = 17 | issue = 3 | pages = 177-80 | month = Sep | year = 2001 | doi = | PMID = 12973074 }} | ||
</ref> | </ref> | ||
*In another series, 48% of individuals with cancer had a PSAD >0.15 ng/ml.<ref name=pmid22482342>{{Cite journal | last1 = Aganovic | first1 = D. | last2 = Prcic | first2 = A. | last3 = Kulovac | first3 = B. | last4 = Hadziosmanovic | first4 = O. | title = Influence of the prostate volume, prostate specific antigen density and number of biopsy samples on prostate cancer detection. | journal = Med Arh | volume = 66 | issue = 1 | pages = 41-4 | month = | year = 2012 | doi = | PMID = 22482342 }} | *In another series, 48% of individuals with cancer had a PSAD >0.15 ng/ml<sup>2</sup>.<ref name=pmid22482342>{{Cite journal | last1 = Aganovic | first1 = D. | last2 = Prcic | first2 = A. | last3 = Kulovac | first3 = B. | last4 = Hadziosmanovic | first4 = O. | title = Influence of the prostate volume, prostate specific antigen density and number of biopsy samples on prostate cancer detection. | journal = Med Arh | volume = 66 | issue = 1 | pages = 41-4 | month = | year = 2012 | doi = | PMID = 22482342 }} | ||
</ref> | </ref> | ||
*Differences between races have been noted in one study; in those without prostate cancer:<ref name=pmid8998182/> | *Differences between races have been noted in one study; in those without prostate cancer:<ref name=pmid8998182/> | ||
**0.19 +/- 0.03 ng/ml (blacks). | **0.19 +/- 0.03 ng/ml<sup>2</sup> (blacks). | ||
**0.11 +/- 0.01 ng/ml (whites). | **0.11 +/- 0.01 ng/ml<sup>2</sup> (whites). | ||
PSAD is a better predictor than (unadjusted) serum PSA for: | PSAD is a better predictor than (unadjusted) serum PSA for: | ||
| Line 47: | Line 51: | ||
:D1, D2, D3 are the major axes. | :D1, D2, D3 are the major axes. | ||
Notes: | |||
*The volume of an ellipsoid is: | *The volume of an ellipsoid is: | ||
::<math>\frac{4}{3}\pi D1 \times D1 \times D3</math>. | ::<math>\frac{4}{3}\pi D1 \times D1 \times D3</math>. | ||
*As 1 cm<sup>3</sup> is equal to 1 ml, the units of PSAD are (ng/ml)/cm<sup>3</sup> or ng/ml<sup>2</sup>. | |||
===Immunostain=== | ===Immunostain=== | ||
* | *Relatively specific for prostate | ||
*May be found in normal pancreatic, salivary gland, Skene's glands and lactating breast tissue.<ref name=pmid21979599>{{cite journal |authors=Kelly P, McBride HA, Kennedy K, Connolly LE, McCluggage WG |title=Misplaced Skene's glands: glandular elements in the lower female genital tract that are variably immunoreactive with prostate markers and that encompass vaginal tubulosquamous polyp and cervical ectopic prostatic tissue |journal=Int. J. Gynecol. Pathol. |volume=30 |issue=6 |pages=605–12 |date=November 2011 |pmid=21979599 |doi=10.1097/PGP.0b013e31821713b6 |url=}}</ref> | |||
*In women, positive in up to 30-40% of breast cancers and also in tubulo-squamous polyps of the vagina. | |||
==Microscopic== | ==Microscopic== | ||
| Line 70: | Line 77: | ||
==See also== | ==See also== | ||
*[[Prostate cancer]]. | *[[Prostate cancer]]. | ||
*[[Prostatic-specific acid phosphatase]]. | |||
==References== | ==References== | ||
Latest revision as of 17:18, 25 March 2021
Prostate-specific antigen, abbreviated PSA, is marker that is quite specific for the prostate.
General
- Quantity in the serum used to screen for prostate cancer and follow patients with a history of prostate cancer.
- PSA immunostain useful for classifying a carcinoma as prostate carcinoma.
Serum PSA
- Normal - typically <= 4.0 ng/ml.
- Sensitivity: 82% (whites), 90% (blacks).[1]
- Specificity: 52% (whites), 38% (blacks).[1]
- Increases with age.[2]
Age-normal:
- 40s - 2.5 ng/ml.
- 50s - 3.5 ng/ml.
- 60s - 4.5 ng/ml.
- 70s - 6.5 ng/ml.
Note:
- The units for PSA may also be μg/L; note that 1 μg/L = 1 ng/ml.
Prostate-specific antigen density
- Abbreviated PSAD.
Normal is often considered to be: <0.15 ng/ml2.
- Approximately 8% of individuals below the cut-point (0.15 ng/ml) have medium or high-grade cancer.[3]
- In another series, 48% of individuals with cancer had a PSAD >0.15 ng/ml2.[4]
- Differences between races have been noted in one study; in those without prostate cancer:[1]
- 0.19 +/- 0.03 ng/ml2 (blacks).
- 0.11 +/- 0.01 ng/ml2 (whites).
PSAD is a better predictor than (unadjusted) serum PSA for:
- Gleason score upgrading on prostatectomy.[5]
- Benign prostate gland versus prostate cancer.[6][7]
A forumla for PSAD
Benson et al.:[6]
Where:
- .[8]
- H, W, L are the height, width and length.
An alternate estimation of the volume is:
- .
- D1, D2, D3 are the major axes.
Notes:
- The volume of an ellipsoid is:
- .
- As 1 cm3 is equal to 1 ml, the units of PSAD are (ng/ml)/cm3 or ng/ml2.
Immunostain
- Relatively specific for prostate
- May be found in normal pancreatic, salivary gland, Skene's glands and lactating breast tissue.[9]
- In women, positive in up to 30-40% of breast cancers and also in tubulo-squamous polyps of the vagina.
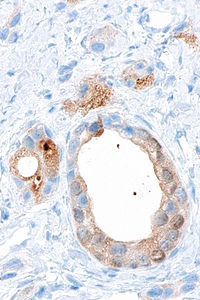
Microscopic
Features - PSA immunostain:
- Granular cytoplasmic staining.
Notes:
- May be very weak -- need to look at high power.
See also
References
- ↑ 1.0 1.1 1.2 Henderson, RJ.; Eastham, JA.; Culkin, DJ.; Kattan, MW.; Whatley, T.; Mata, J.; Venable, D.; Sartor, O. (Jan 1997). "Prostate-specific antigen (PSA) and PSA density: racial differences in men without prostate cancer.". J Natl Cancer Inst 89 (2): 134-8. PMID 8998182.
- ↑ Ku JH, Ahn JO, Lee CH, et al. (September 2002). "Distribution of serum prostate-specific antigen in healthy Korean men: influence of ethnicity". Urology 60 (3): 475–9. PMID 12350489.
- ↑ Boulos, MT.; Rifkin, MD.; Ross, J. (Sep 2001). "Should prostate-specific antigen or prostate-specific antigen density be used as the determining factor when deciding which prostates should undergo biopsy during prostate ultrasound.". Ultrasound Q 17 (3): 177-80. PMID 12973074.
- ↑ Aganovic, D.; Prcic, A.; Kulovac, B.; Hadziosmanovic, O. (2012). "Influence of the prostate volume, prostate specific antigen density and number of biopsy samples on prostate cancer detection.". Med Arh 66 (1): 41-4. PMID 22482342.
- ↑ Sfoungaristos S, Katafigiotis I, Perimenis P (2013). "The role of PSA density to predict a pathological tumour upgrade between needle biopsy and radical prostatectomy for low risk clinical prostate cancer in the modified Gleason system era". Can Urol Assoc J 7 (11-12): E722–7. doi:10.5489/cuaj.374. PMC 3840515. PMID 24282465. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3840515/.
- ↑ 6.0 6.1 Benson MC, Whang IS, Pantuck A, et al. (March 1992). "Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer". J. Urol. 147 (3 Pt 2): 815–6. PMID 1371554.
- ↑ Verma A, St Onge J, Dhillon K, Chorneyko A (June 2014). "PSA density improves prediction of prostate cancer". Can J Urol 21 (3): 7312–21. PMID 24978363.
- ↑ Eri, LM.; Thomassen, H.; Brennhovd, B.; Håheim, LL. (2002). "Accuracy and repeatability of prostate volume measurements by transrectal ultrasound.". Prostate Cancer Prostatic Dis 5 (4): 273-8. doi:10.1038/sj.pcan.4500568. PMID 12627211.
- ↑ Kelly P, McBride HA, Kennedy K, Connolly LE, McCluggage WG (November 2011). "Misplaced Skene's glands: glandular elements in the lower female genital tract that are variably immunoreactive with prostate markers and that encompass vaginal tubulosquamous polyp and cervical ectopic prostatic tissue". Int. J. Gynecol. Pathol. 30 (6): 605–12. doi:10.1097/PGP.0b013e31821713b6. PMID 21979599.