Difference between revisions of "Spermatocytic tumour"
Jump to navigation
Jump to search
(tweak) |
(tweak) |
||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
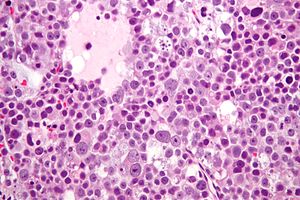
| Image = Spermatocytic_seminoma_high_mag.jpg | | Image = Spermatocytic_seminoma_high_mag.jpg | ||
| Width = | | Width = | ||
| Caption = Spermatocytic seminoma | | Caption = Spermatocytic tumour | ||
| Micro = three cell | | Synonyms = spermatocytic seminoma (old term) | ||
| Micro = three cell populations: (1) small cells (6-8 µm) - with a large NC ratio, (2) medium cells (15-18 µm) with prominent nucleoli and spireme chromatin, (3) Large cells (50-100 µm) with spireme chromatin; mucoid lakes, intratubular spread | |||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[DLBCL]], [[seminoma]] | | LMDDx = [[DLBCL]], [[seminoma]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = SALL4 +ve, OCT3/4 -ve, CD117 +ve/-ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| Line 20: | Line 21: | ||
| Signs = mass lesion | | Signs = mass lesion | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = rare | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = | ||
| Line 27: | Line 28: | ||
| Other = | | Other = | ||
| ClinDDx = other [[germ cell tumours]], [[lymphoma]] | | ClinDDx = other [[germ cell tumours]], [[lymphoma]] | ||
| Tx = excision to exclude malignancy | |||
}} | }} | ||
''' | '''Spermatocytic tumour''' is a rare benign testicular tumour. | ||
It was previously known as '''spermatocytic seminoma'''. It should ''not'' be confused with [[seminoma]] which is an unrelated tumour. | |||
==General== | ==General== | ||
| Line 38: | Line 42: | ||
===Epidemiology=== | ===Epidemiology=== | ||
*Does | *Does ''not'' arise from ''[[germ cell neoplasia in situ]]'' (previously known as ''intratubular germ cell neoplasia'')<ref name=pmid3583416>{{cite journal |author=Müller J, Skakkebaek NE, Parkinson MC |title=The spermatocytic seminoma: views on pathogenesis |journal=Int. J. Androl. |volume=10 |issue=1 |pages=147–56 |year=1987 |month=February |pmid=3583416 |doi= 10.1111/j.1365-2605.1987.tb00176.x|url=}}</ref> - '''not''' considered a subtype of [[seminoma]]. | ||
==Microscopic== | ==Microscopic== | ||
| Line 64: | Line 68: | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
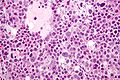
Image:Spermatocytic_seminoma_high_mag.jpg | Spermatocytic | Image:Spermatocytic_seminoma_high_mag.jpg | Spermatocytic tumour - high mag. (WC) | ||
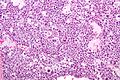
Image:Spermatocytic_seminoma_intermed_mag.jpg | Spermatocytic | Image:Spermatocytic_seminoma_intermed_mag.jpg | Spermatocytic tumour - intermed. mag. (WC) | ||
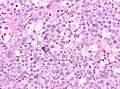
Image:testicular spermatocytic tumour high mag.jpg | Spermatocytic tumour - high mag. (WC) | |||
</gallery> | </gallery> | ||
==IHC== | ==IHC== | ||
Features:<ref name=pmid10223302>{{Cite journal | last1 = Kraggerud | first1 = SM. | last2 = Berner | first2 = A. | last3 = Bryne | first3 = M. | last4 = Pettersen | first4 = EO. | last5 = Fossa | first5 = SD. | title = Spermatocytic seminoma as compared to classical seminoma: an immunohistochemical and DNA flow cytometric study. | journal = APMIS | volume = 107 | issue = 3 | pages = 297-302 | month = Mar | year = 1999 | doi = | PMID = 10223302 }}</ref> | Features:<ref name=pmid10223302>{{Cite journal | last1 = Kraggerud | first1 = SM. | last2 = Berner | first2 = A. | last3 = Bryne | first3 = M. | last4 = Pettersen | first4 = EO. | last5 = Fossa | first5 = SD. | title = Spermatocytic seminoma as compared to classical seminoma: an immunohistochemical and DNA flow cytometric study. | journal = APMIS | volume = 107 | issue = 3 | pages = 297-302 | month = Mar | year = 1999 | doi = | PMID = 10223302 }}</ref> | ||
*PLAP -ve (0 positive/17). | *[[PLAP]] -ve (0 positive/17). | ||
*CD117 -ve (7 positive/17). | *CD117 -ve (7 positive/17). | ||
*CAM5.2 -ve (1 positive/17). | *CAM5.2 -ve (1 positive/17). | ||
Others:<ref>{{Ref WHOGU2022|289}}</ref> | |||
*SALL4 +ve. | |||
*OCT3/4 -ve. | |||
*AFP -ve. | |||
*CD30 -ve. | |||
*Beta-hCG -ve. | |||
==Sign out== | |||
<pre> | |||
Left Testis, Radical Orchiectomy: | |||
- Spermatocytic tumour, see comment. | |||
- NEGATIVE for germ cell neoplasia in situ. | |||
- Background testis with spermatogenesis and atrophy. | |||
Comment: | |||
Spermatocytic tumours are rare. They are not associated with germ cell neoplasia in situ (GCNIS) and typically not seen together with other germ cell types. | |||
The tumour stains as follows: | |||
POSITIVE: CD117 (moderate, patchy), SALL4 (moderate, diffuse), BCL2 (scattered cells, moderate membranous). | |||
NEGATIVE: AE1/AE3, AFP, CD31, CD34, calretinin, hCG, CD3, CD10, CD20, CD30, CD45, GATA3, PLAP, PSA, OCT3/4, CAM5.2, D2-40. | |||
This tumour (spermatoctyic tumour) was previously known as "spermatocytic seminoma". The term "spermatocytic seminoma" is no longer recommended by the World Health Organization, presumably as the name may: (1) create confusion with "seminoma" and (2) falsely raise the possibility of a mixed tumour (that develops in the context of GCNIS). | |||
</pre> | |||
===Micro=== | |||
This tumour has three cell types with spireme chromatin in the larger and intermediate cell type. Infiltrating lymphocytes are absent. | |||
The background testis has some spermatogenesis and atrophic change. Germ cell neoplasia in situ (GCNIS) is ABSENT. The seminiferous tubules adjacent to the tumour, where visualized, are atrophic. | |||
==See also== | ==See also== | ||
Latest revision as of 21:00, 31 October 2024
| Spermatocytic tumour | |
|---|---|
| Diagnosis in short | |
 Spermatocytic tumour | |
|
| |
| Synonyms | spermatocytic seminoma (old term) |
|
| |
| LM | three cell populations: (1) small cells (6-8 µm) - with a large NC ratio, (2) medium cells (15-18 µm) with prominent nucleoli and spireme chromatin, (3) Large cells (50-100 µm) with spireme chromatin; mucoid lakes, intratubular spread |
| LM DDx | DLBCL, seminoma |
| IHC | SALL4 +ve, OCT3/4 -ve, CD117 +ve/-ve |
| Site | testis |
|
| |
| Signs | mass lesion |
| Prevalence | rare |
| Prognosis | benign, good |
| Clin. DDx | other germ cell tumours, lymphoma |
| Treatment | excision to exclude malignancy |
Spermatocytic tumour is a rare benign testicular tumour.
It was previously known as spermatocytic seminoma. It should not be confused with seminoma which is an unrelated tumour.
General
- Rare tumour.
- Only one case of metastases in 200 cases.[1]
- Orchiectomy is curative.
- Not reported/found in females.[1]
- Typically older - mean age 50s.[1]
Epidemiology
- Does not arise from germ cell neoplasia in situ (previously known as intratubular germ cell neoplasia)[2] - not considered a subtype of seminoma.
Microscopic
Features:[3]
- Population of three cells.
- Mucoid lakes.
- Intratubular spread.
Notes:
- Spireme = the tangle of filaments in prophase portion of mitosis.[4]
- May have eosinophilic cytoplasm (dependent on lab).
- Usually larger than Leydig cell tumour.
DDx:
Images
IHC
Features:[5]
- PLAP -ve (0 positive/17).
- CD117 -ve (7 positive/17).
- CAM5.2 -ve (1 positive/17).
Others:[6]
- SALL4 +ve.
- OCT3/4 -ve.
- AFP -ve.
- CD30 -ve.
- Beta-hCG -ve.
Sign out
Left Testis, Radical Orchiectomy: - Spermatocytic tumour, see comment. - NEGATIVE for germ cell neoplasia in situ. - Background testis with spermatogenesis and atrophy. Comment: Spermatocytic tumours are rare. They are not associated with germ cell neoplasia in situ (GCNIS) and typically not seen together with other germ cell types. The tumour stains as follows: POSITIVE: CD117 (moderate, patchy), SALL4 (moderate, diffuse), BCL2 (scattered cells, moderate membranous). NEGATIVE: AE1/AE3, AFP, CD31, CD34, calretinin, hCG, CD3, CD10, CD20, CD30, CD45, GATA3, PLAP, PSA, OCT3/4, CAM5.2, D2-40. This tumour (spermatoctyic tumour) was previously known as "spermatocytic seminoma". The term "spermatocytic seminoma" is no longer recommended by the World Health Organization, presumably as the name may: (1) create confusion with "seminoma" and (2) falsely raise the possibility of a mixed tumour (that develops in the context of GCNIS).
Micro
This tumour has three cell types with spireme chromatin in the larger and intermediate cell type. Infiltrating lymphocytes are absent.
The background testis has some spermatogenesis and atrophic change. Germ cell neoplasia in situ (GCNIS) is ABSENT. The seminiferous tubules adjacent to the tumour, where visualized, are atrophic.
See also
References
- ↑ 1.0 1.1 1.2 1.3 Eble JN (October 1994). "Spermatocytic seminoma". Hum. Pathol. 25 (10): 1035–42. PMID 7927308.
- ↑ Müller J, Skakkebaek NE, Parkinson MC (February 1987). "The spermatocytic seminoma: views on pathogenesis". Int. J. Androl. 10 (1): 147–56. doi:10.1111/j.1365-2605.1987.tb00176.x. PMID 3583416.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-0187-1.
- ↑ URL: http://www.thefreedictionary.com/spireme. Accessed on: 4 June 2010.
- ↑ Kraggerud, SM.; Berner, A.; Bryne, M.; Pettersen, EO.; Fossa, SD. (Mar 1999). "Spermatocytic seminoma as compared to classical seminoma: an immunohistochemical and DNA flow cytometric study.". APMIS 107 (3): 297-302. PMID 10223302.
- ↑ WHO Classification of Tumours Editorial Board (2022). Urinary and Male Genital Tumours (5th ed.). Lyon: World Health Organization. pp. 289. ISBN 978-9283245124.