Difference between revisions of "Medullary colorectal carcinoma"
Jump to navigation
Jump to search
m (add gallery) |
|||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'''Medullary colorectal carcinoma''' is a rare type of [[colorectal carcinoma]]. | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Photomicrograph_of_colorectal_medullary_carcinoma_x20a.jpg | |||
| Width = | |||
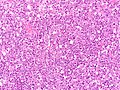
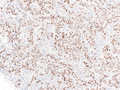
| Caption = Micrograph of a medullary colorectal carcinoma. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = Sheet-like architecture of malignant cells with vesicular nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm. Admixed inflammatory cells (lymphocytes and neutrophils) are common. | |||
| Subtypes = | |||
| LMDDx = Poorly differentiated adenocarcinoma, melanoma, poorly differentiated neuroendocrine tumours, high grade lymphoma | |||
| Stains = | |||
| IHC = May lose CK20 and CDX2. Frequent loss of MLH1/PMS2. SATB2 +ve, BRAF VE1 +ve, calretinin +ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Staging = | |||
| Site = Colorectum, most commonly right side of colon | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = 1-3% of all colorectal carcinomas | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = Some papers suggest better prognosis than conventional adenocarcinoma | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
'''Medullary colorectal carcinoma''' is a rare type of [[colorectal carcinoma]]. Precise incidence difficult to determine as there no strict criteria for diagnosis, especially if the tumour also contains conventional adenocarcinoma. Cases may not be recognised and diagnosed as poorly differentiated adenocarcinona instead.<ref name=pmid33247957>{{cite journal |vauthors=Scott N, West NP, Cairns A, Rotimi O |title=Is medullary carcinoma of the colon underdiagnosed? An audit of poorly differentiated colorectal carcinomas in a large national health service teaching hospital |journal=Histopathology |volume=78 |issue=7 |pages=963–969 |date=June 2021 |pmid=33247957 |doi=10.1111/his.14310 |url=}}</ref> | |||
==General== | ==General== | ||
*Rare subtype of colorectal carcinoma. | *Rare subtype of colorectal carcinoma. In these papers: 1.1%<ref name=pmid33247957/>, 2.8%<ref name=pmid25572685>{{cite journal |vauthors=Knox RD, Luey N, Sioson L, Kedziora A, Clarkson A, Watson N, Toon CW, Cussigh C, Pincott S, Pillinger S, Salama Y, Evans J, Percy J, Schnitzler M, Engel A, Gill AJ |title=Medullary colorectal carcinoma revisited: a clinical and pathological study of 102 cases |journal=Ann Surg Oncol |volume=22 |issue=9 |pages=2988–96 |date=September 2015 |pmid=25572685 |doi=10.1245/s10434-014-4355-5 |url=}}</ref>, and 3.6%<ref name=pmid10561306>{{cite journal |vauthors=Lanza G, Gafà R, Matteuzzi M, Santini A |title=Medullary-type poorly differentiated adenocarcinoma of the large bowel: a distinct clinicopathologic entity characterized by microsatellite instability and improved survival |journal=J Clin Oncol |volume=17 |issue=8 |pages=2429–38 |date=August 1999 |pmid=10561306 |doi=10.1200/JCO.1999.17.8.2429 |url=}}</ref> | ||
*Typically has [[MSI| | *Typically has [[MSI|microsatellite instability]].<ref name=pmid24815832 >{{cite journal |authors=Cunningham J, Kantekure K, Saif MW |title=Medullary carcinoma of the colon: a case series and review of the literature |journal=In Vivo |volume=28 |issue=3 |pages=311–4 |date=2014 |pmid=24815832 |doi= |url=}}</ref> | ||
*Prognostic significance dependent on study. | *Prognostic significance dependent on study. | ||
**A small series suggests the prognosis of medullary carcinoma with MSI is worse that conventional colorectal carcinoma without MSI.<ref>{{cite journal |authors=Gómez-Álvarez MA, Lino-Silva LS, Salcedo-Hernández RA, Padilla-Rosciano A, Ruiz-García EB, López-Basave HN, Calderillo-Ruiz G, Aguilar-Romero JM, Domínguez-Rodríguez JA, Herrera-Gómez Á, Meneses-García A |title=Medullary colonic carcinoma with microsatellite instability has lower survival compared with conventional colonic adenocarcinoma with microsatellite instability |journal=Prz Gastroenterol |volume=12 |issue=3 |pages=208–214 |date=2017 |pmid=29123583 |pmc=5672702 |doi=10.5114/pg.2016.64740 |url=}}</ref> | **A small series suggests the prognosis of medullary carcinoma with MSI is worse that conventional colorectal carcinoma without MSI.<ref>{{cite journal |authors=Gómez-Álvarez MA, Lino-Silva LS, Salcedo-Hernández RA, Padilla-Rosciano A, Ruiz-García EB, López-Basave HN, Calderillo-Ruiz G, Aguilar-Romero JM, Domínguez-Rodríguez JA, Herrera-Gómez Á, Meneses-García A |title=Medullary colonic carcinoma with microsatellite instability has lower survival compared with conventional colonic adenocarcinoma with microsatellite instability |journal=Prz Gastroenterol |volume=12 |issue=3 |pages=208–214 |date=2017 |pmid=29123583 |pmc=5672702 |doi=10.5114/pg.2016.64740 |url=}}</ref> | ||
**A series with 102 cases suggests a better prognosis when compared on the basis of other pathological characteristics.<ref name=pmid25572685 | **A series with 102 cases suggests a better prognosis when compared on the basis of other pathological characteristics.<ref name=pmid25572685/> | ||
==Gross== | ==Gross== | ||
| Line 21: | Line 53: | ||
DDx: | DDx: | ||
*Other (poorly differentiated) [[colorectal carcinoma]]s. | *Other (poorly differentiated) [[colorectal carcinoma]]s. | ||
**Colorectal cancer with loss of [[SMARCB1]] expression.<ref name=pmid32083567/> | |||
*Carcinomas with neuroendocrine differentiation. | *Carcinomas with neuroendocrine differentiation. | ||
*[[Lymphoepithelioma-like carcinoma]] of the colon.<ref>{{cite journal |authors=Delaney D, Chetty R |title=Lymphoepithelioma-like carcinoma of the colon |journal=Int J Clin Exp Pathol |volume=5 |issue=1 |pages=105–9 |date=2012 |pmid=22295155 |pmc=3267494 |doi= |url=}}</ref> | *[[Lymphoepithelioma-like carcinoma]] of the colon.<ref>{{cite journal |authors=Delaney D, Chetty R |title=Lymphoepithelioma-like carcinoma of the colon |journal=Int J Clin Exp Pathol |volume=5 |issue=1 |pages=105–9 |date=2012 |pmid=22295155 |pmc=3267494 |doi= |url=}}</ref> | ||
| Line 26: | Line 59: | ||
==IHC== | ==IHC== | ||
Features:<ref name=pmid24815832/> | Features:<ref name=pmid24815832/> | ||
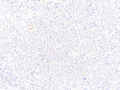
*CDX2 +ve | *CDX2 +ve (though can be lost) | ||
*Beta-catenin +ve. | *Beta-catenin +ve. | ||
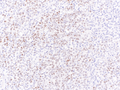
*MLH1 loss of staining. | *MLH1/PMS2 loss of staining. | ||
*Calretinin (67%-73%)<ref>{{cite journal |authors=Winn B, Tavares R, Fanion J, Noble L, Gao J, Sabo E, Resnick MB |title=Differentiating the undifferentiated: immunohistochemical profile of medullary carcinoma of the colon with an emphasis on intestinal differentiation |journal=Hum. Pathol. |volume=40 |issue=3 |pages=398–404 |date=March 2009 |pmid=18992917 |pmc=2657293 |doi=10.1016/j.humpath.2008.08.014 |url=}}</ref><ref>{{cite journal |authors=Lin F, Shi J, Zhu S, Chen Z, Li A, Chen T, Wang HL, Liu H |title=Cadherin-17 and SATB2 are sensitive and specific immunomarkers for medullary carcinoma of the large intestine |journal=Arch. Pathol. Lab. Med. |volume=138 |issue=8 |pages=1015–26 |date=August 2014 |pmid=24437456 |doi=10.5858/arpa.2013-0452-OA |url=}}</ref> | *Calretinin (67%-73%)<ref>{{cite journal |authors=Winn B, Tavares R, Fanion J, Noble L, Gao J, Sabo E, Resnick MB |title=Differentiating the undifferentiated: immunohistochemical profile of medullary carcinoma of the colon with an emphasis on intestinal differentiation |journal=Hum. Pathol. |volume=40 |issue=3 |pages=398–404 |date=March 2009 |pmid=18992917 |pmc=2657293 |doi=10.1016/j.humpath.2008.08.014 |url=}}</ref><ref>{{cite journal |authors=Lin F, Shi J, Zhu S, Chen Z, Li A, Chen T, Wang HL, Liu H |title=Cadherin-17 and SATB2 are sensitive and specific immunomarkers for medullary carcinoma of the large intestine |journal=Arch. Pathol. Lab. Med. |volume=138 |issue=8 |pages=1015–26 |date=August 2014 |pmid=24437456 |doi=10.5858/arpa.2013-0452-OA |url=}}</ref> | ||
Notes: | |||
*CDX2, beta-catenin, MLH1 useful for differentiating from poorly differentiated colorectal carcinoma. | *CDX2, beta-catenin, MLH1 useful for differentiating from poorly differentiated colorectal carcinoma. | ||
*SMARCB1 loss - reported in one case.<ref name=pmid32083567>{{cite journal |authors=Melloul S, Mosnier JF, Masliah-Planchon J, Lepage C, Le Malicot K, Gornet JM, Edeline J, Dansette D, Texereau P, Delattre O, Laurent Puig P, Taieb J, Emile JF |title=Loss of SMARCB1 expression in colon carcinoma |journal=Cancer Biomark |volume=27 |issue=3 |pages=399–406 |date=2020 |pmid=32083567 |doi=10.3233/CBM-190287 |url=}}</ref> | |||
===Images=== | |||
<gallery> | |||
Image:Photomicrograph of colorectal medullary carcinoma x20a.jpg | Note numerous interspersed inflammatory cells (WC) | |||
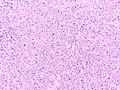
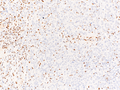
Image:Photomicrograph of colorectal medullary carcinoma x20d.jpg | Note numerous interspersed inflammatory cells (WC) | |||
</gallery> | |||
<gallery> | |||
Image: Photomicrograph of medullary carcinoma at anorectum x4a.jpg | Medullary carcinoma - low mag. (WC) | |||
Image: Photomicrograph of medullary carcinoma at anorectum x20a.jpg | Medullary carcinoma - medium/high mag. (WC) | |||
Image: Photomicrograph of medullary carcinoma CK7 immunohistochemistry x20.png | CK7 negative (WC) | |||
Image: Photomicrograph of medullary carcinoma CK20 immunohistochemistry x20.png | CK20 negative (WC) | |||
Image: Photomicrograph of medullary carcinoma CDX2 immunohistochemistry x20.png | CDX2 variably positive (WC) | |||
Image: Photomicrograph of medullary carcinoma SATB2 immunohistochemistry x20.png | SATB2 positive (WC) | |||
Image: Photomicrograph of medullary carcinoma MLH1 immunohistochemistry x20.png | Loss of MLH1 expression (WC) | |||
Image: Photomicrograph of medullary carcinoma PMS2 immunohistochemistry x20.png | Loss of PMS2 expression (WC) | |||
Image: Photomicrograph of medullary carcinoma BRAF-VE1 immunohistochemistry x20.png | BRAF VE1 positive (WC) | |||
</gallery> | |||
==See also== | ==See also== | ||
Latest revision as of 21:15, 1 June 2023
| Medullary colorectal carcinoma | |
|---|---|
| Diagnosis in short | |
 Micrograph of a medullary colorectal carcinoma. H&E stain. | |
|
| |
| LM | Sheet-like architecture of malignant cells with vesicular nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm. Admixed inflammatory cells (lymphocytes and neutrophils) are common. |
| LM DDx | Poorly differentiated adenocarcinoma, melanoma, poorly differentiated neuroendocrine tumours, high grade lymphoma |
| IHC | May lose CK20 and CDX2. Frequent loss of MLH1/PMS2. SATB2 +ve, BRAF VE1 +ve, calretinin +ve |
| Site | Colorectum, most commonly right side of colon |
|
| |
| Prevalence | 1-3% of all colorectal carcinomas |
| Prognosis | Some papers suggest better prognosis than conventional adenocarcinoma |
Medullary colorectal carcinoma is a rare type of colorectal carcinoma. Precise incidence difficult to determine as there no strict criteria for diagnosis, especially if the tumour also contains conventional adenocarcinoma. Cases may not be recognised and diagnosed as poorly differentiated adenocarcinona instead.[1]
General
- Rare subtype of colorectal carcinoma. In these papers: 1.1%[1], 2.8%[2], and 3.6%[3]
- Typically has microsatellite instability.[4]
- Prognostic significance dependent on study.
Gross
- Well-circumscribed.
Microscopic
Features:
- Poorly differentiated carcinoma:
- Noninfiltrative border.
- Solid pattern/nests.
- No gland formation.
- Lymphocytic infiltrate.
DDx:
- Other (poorly differentiated) colorectal carcinomas.
- Carcinomas with neuroendocrine differentiation.
- Lymphoepithelioma-like carcinoma of the colon.[7]
IHC
Features:[4]
- CDX2 +ve (though can be lost)
- Beta-catenin +ve.
- MLH1/PMS2 loss of staining.
- Calretinin (67%-73%)[8][9]
Notes:
- CDX2, beta-catenin, MLH1 useful for differentiating from poorly differentiated colorectal carcinoma.
- SMARCB1 loss - reported in one case.[6]
Images
See also
References
- ↑ 1.0 1.1 "Is medullary carcinoma of the colon underdiagnosed? An audit of poorly differentiated colorectal carcinomas in a large national health service teaching hospital". Histopathology 78 (7): 963–969. June 2021. doi:10.1111/his.14310. PMID 33247957.
- ↑ 2.0 2.1 "Medullary colorectal carcinoma revisited: a clinical and pathological study of 102 cases". Ann Surg Oncol 22 (9): 2988–96. September 2015. doi:10.1245/s10434-014-4355-5. PMID 25572685.
- ↑ "Medullary-type poorly differentiated adenocarcinoma of the large bowel: a distinct clinicopathologic entity characterized by microsatellite instability and improved survival". J Clin Oncol 17 (8): 2429–38. August 1999. doi:10.1200/JCO.1999.17.8.2429. PMID 10561306.
- ↑ 4.0 4.1 Cunningham J, Kantekure K, Saif MW (2014). "Medullary carcinoma of the colon: a case series and review of the literature". In Vivo 28 (3): 311–4. PMID 24815832.
- ↑ Gómez-Álvarez MA, Lino-Silva LS, Salcedo-Hernández RA, Padilla-Rosciano A, Ruiz-García EB, López-Basave HN, Calderillo-Ruiz G, Aguilar-Romero JM, Domínguez-Rodríguez JA, Herrera-Gómez Á, Meneses-García A (2017). "Medullary colonic carcinoma with microsatellite instability has lower survival compared with conventional colonic adenocarcinoma with microsatellite instability". Prz Gastroenterol 12 (3): 208–214. doi:10.5114/pg.2016.64740. PMC 5672702. PMID 29123583. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672702/.
- ↑ 6.0 6.1 Melloul S, Mosnier JF, Masliah-Planchon J, Lepage C, Le Malicot K, Gornet JM, Edeline J, Dansette D, Texereau P, Delattre O, Laurent Puig P, Taieb J, Emile JF (2020). "Loss of SMARCB1 expression in colon carcinoma". Cancer Biomark 27 (3): 399–406. doi:10.3233/CBM-190287. PMID 32083567.
- ↑ Delaney D, Chetty R (2012). "Lymphoepithelioma-like carcinoma of the colon". Int J Clin Exp Pathol 5 (1): 105–9. PMC 3267494. PMID 22295155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267494/.
- ↑ Winn B, Tavares R, Fanion J, Noble L, Gao J, Sabo E, Resnick MB (March 2009). "Differentiating the undifferentiated: immunohistochemical profile of medullary carcinoma of the colon with an emphasis on intestinal differentiation". Hum. Pathol. 40 (3): 398–404. doi:10.1016/j.humpath.2008.08.014. PMC 2657293. PMID 18992917. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2657293/.
- ↑ Lin F, Shi J, Zhu S, Chen Z, Li A, Chen T, Wang HL, Liu H (August 2014). "Cadherin-17 and SATB2 are sensitive and specific immunomarkers for medullary carcinoma of the large intestine". Arch. Pathol. Lab. Med. 138 (8): 1015–26. doi:10.5858/arpa.2013-0452-OA. PMID 24437456.