Difference between revisions of "Small bowel pseudomelanosis"
Jump to navigation
Jump to search
(create) |
|||
| (18 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
''' | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Small bowel pseudomelanosis - alt -- intermed mag.jpg | |||
| Width = | |||
| Caption = Small bowel pseudomelanosis. [[H&E stain]]. | |||
| Synonyms = pseudomelanosis duodeni (for [[duodenum]]) | |||
| Micro = dark pigment in the lamina propria macrophages | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = iron stain +ve | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Staging = | |||
| Site = [[small bowel]], [[stomach]] | |||
| Assdx = iron deficiency [[anemia]], [[end-stage renal disease]], [[hypertension]] | |||
| Syndromes = | |||
| Clinicalhx = iron supplementation | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = rare | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = +/-dark spots | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
'''Small bowel pseudomelanosis''' is benign change of the [[small bowel]] that mimics melanin deposition. | |||
In the [[duodenum]] it is known as ''' pseudomelanosis duodeni'''. | |||
Pseudomelanosis is described in the [[stomach]], [[duodenum]] and [[jejunum]].<ref name=pmid24492404>{{Cite journal | last1 = Rustagi | first1 = T. | last2 = Mansoor | first2 = MS. | last3 = Gibson | first3 = JA. | last4 = Kapadia | first4 = CR. | title = Pseudomelanosis of stomach, duodenum, and jejunum. | journal = J Clin Gastroenterol | volume = 49 | issue = 2 | pages = 124-6 | month = Feb | year = 2015 | doi = 10.1097/MCG.0000000000000081 | PMID = 24492404 }}</ref> | |||
==General== | ==General== | ||
*Rare. | *Rare and benign.<ref name=pmid22493558>{{Cite journal | last1 = de Magalhães Costa | first1 = MH. | last2 = Fernandes Pegado | first2 = Mda G. | last3 = Vargas | first3 = C. | last4 = Castro | first4 = ME. | last5 = Madi | first5 = K. | last6 = Nunes | first6 = T. | last7 = Zaltman | first7 = C. | title = Pseudomelanosis duodeni associated with chronic renal failure. | journal = World J Gastroenterol | volume = 18 | issue = 12 | pages = 1414-6 | month = Mar | year = 2012 | doi = 10.3748/wjg.v18.i12.1414 | PMID = 22493558 }}</ref> | ||
*Consists of iron and lipofuscin.<ref name=pmid2458404>{{Cite journal | last1 = Lin | first1 = HJ. | last2 = Tsay | first2 = SH. | last3 = Chiang | first3 = H. | last4 = Tsai | first4 = YT. | last5 = Lee | first5 = SD. | last6 = Yeh | first6 = YS. | last7 = Lo | first7 = GH. | title = Pseudomelanosis duodeni. Case report and review of literature. | journal = J Clin Gastroenterol | volume = 10 | issue = 2 | pages = 155-9 | month = Apr | year = 1988 | doi = | PMID = 2458404 }} | *Consists of iron and lipofuscin.<ref name=pmid2458404>{{Cite journal | last1 = Lin | first1 = HJ. | last2 = Tsay | first2 = SH. | last3 = Chiang | first3 = H. | last4 = Tsai | first4 = YT. | last5 = Lee | first5 = SD. | last6 = Yeh | first6 = YS. | last7 = Lo | first7 = GH. | title = Pseudomelanosis duodeni. Case report and review of literature. | journal = J Clin Gastroenterol | volume = 10 | issue = 2 | pages = 155-9 | month = Apr | year = 1988 | doi = | PMID = 2458404 }} | ||
</ref> | </ref> | ||
Associations:<ref name=pmid18253910/> | Associations in a series of 17 individuals:<ref name=pmid18253910/> | ||
*[[Hypertension]] ~90% of cases. | *[[Hypertension]] ~90% of cases. | ||
*Iron supplementation ~75% of cases. | *Iron supplementation ~75% of cases. | ||
| Line 21: | Line 57: | ||
*Dark pigment in the lamina propria macrophages. | *Dark pigment in the lamina propria macrophages. | ||
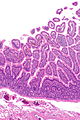
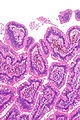
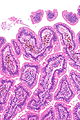
Images: | ===Images=== | ||
====Case 1==== | |||
<gallery> | |||
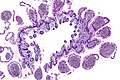
Image: Small bowel pseudomelanosis -- low mag.jpg | SBP - low mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis -- intermed mag.jpg | SBP - intermed. mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis - alt -- intermed mag.jpg | SBP - intermed. mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis -- high mag.jpg | SBP - high mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis -- very high mag.jpg | SBP - very high mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis - iron -- intermed mag.jpg | SBP - intermed. mag. (WC/Nephron) | |||
Image: Small bowel pseudomelanosis - iron -- high mag.jpg | SBP - high mag. (WC/Nephron) | |||
</gallery> | |||
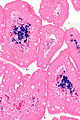
====Case 2==== | |||
<gallery> | |||
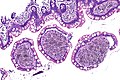
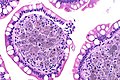
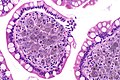
Image: Pseudomelanosis ileum -- very low mag.jpg | PI - very low mag. (WC) | |||
Image: Pseudomelanosis ileum -- low mag.jpg | PI - low mag. (WC) | |||
Image: Pseudomelanosis ileum -- intermed mag.jpg | PI - intermed. mag. (WC) | |||
Image: Pseudomelanosis ileum -- high mag.jpg | PI - high mag. (WC) | |||
Image: Pseudomelanosis ileum - alt -- high mag.jpg | PI - high mag. (WC) | |||
Image: Pseudomelanosis ileum -- very high mag.jpg | PI - very high mag. (WC) | |||
</gallery> | |||
====www==== | |||
*[http://path.upmc.edu/cases/case616.html Pseudomelanosis duodeni - several images (upmc.edu)]. | *[http://path.upmc.edu/cases/case616.html Pseudomelanosis duodeni - several images (upmc.edu)]. | ||
==Stains== | ==Stains== | ||
*Prussian blue +ve ~80% of cases.<ref name=pmid18253910/> | *Prussian blue +ve ~80% of cases.<ref name=pmid18253910/> | ||
==Sign out== | |||
===Small bowel=== | |||
<pre> | |||
A. Stomach, Partial Excision as Part of a Sleeve Gastrectomy: | |||
- Stomach wall within normal limits. | |||
B. Small Bowel Wall, Partial Excision as Part of a Sleeve Gastrectomy: | |||
- Small bowel wall with iron containing macrophages in the mucosa, | |||
known as "pseudomelanosis", see comment. | |||
- NEGATIVE for active inflammation. | |||
- NEGATIVE for dysplasia and NEGATIVE for malignancy. | |||
Comment: | |||
Pseudomelanosis may be seen in the context of iron supplementation, hypertension | |||
or chronic renal failure. | |||
The macrophages are positive with an iron stain. | |||
</pre> | |||
===Duodenum=== | |||
<pre> | |||
Duodenum, Biopsy: | |||
- Small bowel mucosa with pseudomelanosis, otherwise within | |||
normal limits, see comment. | |||
Comment: | |||
Pseudomelanosis of the duodenum (pseudomelanosis duodeni) may be seen in the context of iron supplementation, hypertension or chronic renal failure. Endoscopically, it may manifest as dark spots. | |||
The pigmented cells are POSITIVE with an iron stain, NEGATIVE with a PAS stain and NEGATIVE with a Fontana-Masson stain; these findings are in keeping pseudomelanosis duodeni. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Pseudomelanosis coli]]. | *[[Pseudomelanosis coli]]. | ||
*[[Melanocytic lesions]]. | |||
==References== | ==References== | ||
Latest revision as of 01:40, 15 July 2019
| Small bowel pseudomelanosis | |
|---|---|
| Diagnosis in short | |
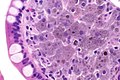
 Small bowel pseudomelanosis. H&E stain. | |
|
| |
| Synonyms | pseudomelanosis duodeni (for duodenum) |
|
| |
| LM | dark pigment in the lamina propria macrophages |
| Stains | iron stain +ve |
| Site | small bowel, stomach |
|
| |
| Associated Dx | iron deficiency anemia, end-stage renal disease, hypertension |
| Clinical history | iron supplementation |
| Prevalence | rare |
| Endoscopy | +/-dark spots |
| Prognosis | benign |
Small bowel pseudomelanosis is benign change of the small bowel that mimics melanin deposition.
In the duodenum it is known as pseudomelanosis duodeni.
Pseudomelanosis is described in the stomach, duodenum and jejunum.[1]
General
Associations in a series of 17 individuals:[4]
- Hypertension ~90% of cases.
- Iron supplementation ~75% of cases.
- End-stage renal disease ~60% of cases.
Note:
- The associations are different than for melanosis coli.
Gross/endoscopic
- Dark spots ~35% of cases.[4]
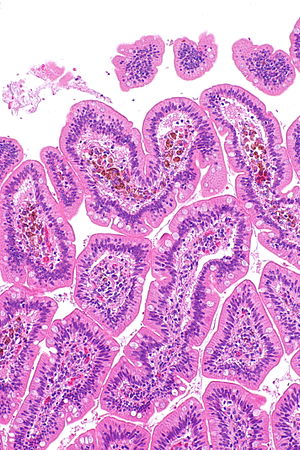
Microscopic
Features:
- Dark pigment in the lamina propria macrophages.
Images
Case 1
Case 2
www
Stains
- Prussian blue +ve ~80% of cases.[4]
Sign out
Small bowel
A. Stomach, Partial Excision as Part of a Sleeve Gastrectomy: - Stomach wall within normal limits. B. Small Bowel Wall, Partial Excision as Part of a Sleeve Gastrectomy: - Small bowel wall with iron containing macrophages in the mucosa, known as "pseudomelanosis", see comment. - NEGATIVE for active inflammation. - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: Pseudomelanosis may be seen in the context of iron supplementation, hypertension or chronic renal failure. The macrophages are positive with an iron stain.
Duodenum
Duodenum, Biopsy: - Small bowel mucosa with pseudomelanosis, otherwise within normal limits, see comment. Comment: Pseudomelanosis of the duodenum (pseudomelanosis duodeni) may be seen in the context of iron supplementation, hypertension or chronic renal failure. Endoscopically, it may manifest as dark spots. The pigmented cells are POSITIVE with an iron stain, NEGATIVE with a PAS stain and NEGATIVE with a Fontana-Masson stain; these findings are in keeping pseudomelanosis duodeni.
See also
References
- ↑ Rustagi, T.; Mansoor, MS.; Gibson, JA.; Kapadia, CR. (Feb 2015). "Pseudomelanosis of stomach, duodenum, and jejunum.". J Clin Gastroenterol 49 (2): 124-6. doi:10.1097/MCG.0000000000000081. PMID 24492404.
- ↑ de Magalhães Costa, MH.; Fernandes Pegado, Mda G.; Vargas, C.; Castro, ME.; Madi, K.; Nunes, T.; Zaltman, C. (Mar 2012). "Pseudomelanosis duodeni associated with chronic renal failure.". World J Gastroenterol 18 (12): 1414-6. doi:10.3748/wjg.v18.i12.1414. PMID 22493558.
- ↑ Lin, HJ.; Tsay, SH.; Chiang, H.; Tsai, YT.; Lee, SD.; Yeh, YS.; Lo, GH. (Apr 1988). "Pseudomelanosis duodeni. Case report and review of literature.". J Clin Gastroenterol 10 (2): 155-9. PMID 2458404.
- ↑ 4.0 4.1 4.2 Giusto, D.; Jakate, S. (Feb 2008). "Pseudomelanosis duodeni: associated with multiple clinical conditions and unpredictable iron stainability - a case series.". Endoscopy 40 (2): 165-7. doi:10.1055/s-2007-995472. PMID 18253910.