Difference between revisions of "Lymph node metastasis"
Jump to navigation
Jump to search
| Line 13: | Line 13: | ||
| Molecular = | | Molecular = | ||
| IF = | | IF = | ||
| Gross = enlarged lymph node, esp. spherical, white mass | | Gross = enlarged lymph node, esp. spherical, white mass with an irregular border +/-extension into surround adipose tissue | ||
| Grossing = | | Grossing = | ||
| Site = [[lymph node]] - see ''[[lymph node pathology]]'' | | Site = [[lymph node]] - see ''[[lymph node pathology]]'' | ||
Revision as of 03:24, 10 January 2014
| Lymph node metastasis | |
|---|---|
| Diagnosis in short | |
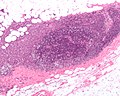
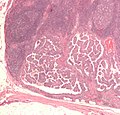
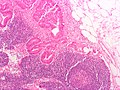
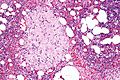
 Lymph node metastasis (colorectal carcinoma). H&E stain. | |
|
| |
| LM | malignant cells foreign to the lymph node - dependent on specific cancer |
| Subtypes | micrometastasis, macrometastasis |
| LM DDx | endometriosis, ectopic decidua, endosalpingiosis, melanocytic nevus, dermatopathic lymphadenopathy, sinus histiocytosis, tumour deposit (dependent on site), isolated tumour cells, pathology of the lymph node - see lymph node pathology and lymphoma |
| Stains | dependent on tumour |
| IHC | dependent on tumour |
| Gross | enlarged lymph node, esp. spherical, white mass with an irregular border +/-extension into surround adipose tissue |
| Site | lymph node - see lymph node pathology |
|
| |
| Clinical history | +/-suspicion of cancer |
| Signs | +/-nodule at site of a lymph node |
| Prognosis | dependent on specific type of cancer, +/-number of nodes affected |
| Clin. DDx | reactive lymphadenopathy, lymphoma, other benign causes of lymphadenopathy - see lymph node pathology |
| Treatment | dependent on underlying cancer |
Lymph node metastasis is cancer that has spread to a lymph node.
General
- Determination of lymph node status is one of the most common indications for the examination of lymph nodes.
- It is a good idea to look at the tumour (if available) ...before looking at the LNs for mets.
- Lymph node metastasis, in the absence of other metastases, often up-stage a cancer from stage II to stage III.
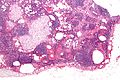
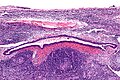
Gross
- Outside:
- "Large" - size varies by site.
- Neck >10 mm.[1]
- Shape - round more suspicious than oval.
- "Large" - size varies by site.
- Sectioned:
- White firm lesion with irregular border - classic appearance.
- Non-fatty hilum.[1]
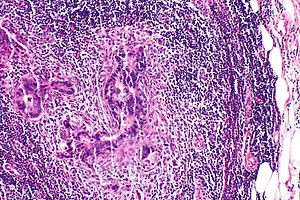
Microscopic
Features:
- Foreign cell population - key feature.
- Classic location: subcapsular sinuses.
- +/-Cells with cytologic features of malignancy.
- Nuclear pleomorphism (variation in size, shape and staining).
- Nuclear atypia:
- Nuclear enlargement.
- Irregular nuclear membrane.
- Irregular chromatin pattern, esp. asymmetry.
- Large or irregular nucleolus.
- Abundant mitotic figures.
- +/-Cells in architectural arrangements seen in malignancy; highly variable - dependent on tumour type and differentiation.
- +/-Gland formation.
- +/-Single cells.
- +/-Small clusters of cells.
Notes:
- Cytologic features of malignancy may not be present; some tumours, e.g. gallbladder carcinoma, do not always have overt cytologic features of malignancy.
- The diagnosis is based on the fact that they are foreign to the lymph node and architecturally consistent with a well-differentiated malignancy.
- Lymph node metastases in sarcomas are uncommon; they are seen in <3% of cases.[2]
- Fatty lymph nodes (esp. fatty hilus[1]) are less likely to harbor metastases.[3]
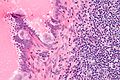
DDx - mimics of metastatic disease:
- Endometriosis.
- Ectopic decidua.[4]
- Endosalpingiosis.[5]
- Melanocytic nevus - intracapsular or within the trabeculae.[6]
- Dermatopathic lymphadenopathy.[citation needed]
- Sinus histiocytosis - especially for the junior resident.
- Tumour deposit (discoutinuous extramural extension) - definition dependent on primary tumour (e.g. in the head & neck they are tumour replaced lymph nodes, in the colon they are considered separate and not counted as lymph nodes).
Images
Mimics
See also
References
- ↑ 1.0 1.1 1.2 Mack, MG.; Rieger, J.; Baghi, M.; Bisdas, S.; Vogl, TJ. (Jun 2008). "Cervical lymph nodes.". Eur J Radiol 66 (3): 493-500. doi:10.1016/j.ejrad.2008.01.019. PMID 18337039.
- ↑ Fong, Y.; Coit, DG.; Woodruff, JM.; Brennan, MF. (Jan 1993). "Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients.". Ann Surg 217 (1): 72-7. PMC 1242736. PMID 8424704. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242736/.
- ↑ Korteweg, MA.; Veldhuis, WB.; Mali, WP.; Diepstraten, SC.; Luijten, PR.; van den Bosch, MA.; Eijkemans, RM.; van Diest, PJ. et al. (Feb 2012). "Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy.". J Magn Reson Imaging 35 (2): 387-92. doi:10.1002/jmri.22820. PMID 21972135.
- ↑ Wu, DC.; Hirschowitz, S.; Natarajan, S. (May 2005). "Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall.". Arch Pathol Lab Med 129 (5): e117-20. doi:10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2. PMID 15859655.
- ↑ Corben, AD.; Nehhozina, T.; Garg, K.; Vallejo, CE.; Brogi, E. (Aug 2010). "Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma.". Am J Surg Pathol 34 (8): 1211-6. doi:10.1097/PAS.0b013e3181e5e03e. PMID 20631604.
- ↑ Biddle, DA.; Evans, HL.; Kemp, BL.; El-Naggar, AK.; Harvell, JD.; White, WL.; Iskandar, SS.; Prieto, VG. (May 2003). "Intraparenchymal nevus cell aggregates in lymph nodes: a possible diagnostic pitfall with malignant melanoma and carcinoma.". Am J Surg Pathol 27 (5): 673-81. PMID 12717252.