Urine cytopathology
Revision as of 23:47, 25 March 2015 by Michael (talk | contribs) (→Proposed Paris system for urinary cytology)
Urine cytopathology is a large part of cytopathology.
This article deals only with urine cytopathology. An introduction to cytopathology is in the cytopathology article.
DDx
Common
- Negative for malignancy.
- Urothelial carcinoma.
- Urothelial carcinoma with squamous features.
- Polyomavirus infection.
- Acute inflammation.
- Chronic inflammation.
Rare
Usually not reported
- Candida.
- Quite common.
- Large (benign) squamous component.
- Usually contamination from gential tract (in females).
Proposed Paris system for urinary cytology
Proposed in 2013:[1]
- Nondiagnostic/unsatisfactory
- Negative for HGPUC.
- Atypical urothelial cells.
- Suspicous for HGPUC.
- HGPUC.
- Low grade urothelial neoplasm.
- Other malignancy - includes both primary and secondary.
Normal
General
- Benign cells are often in small clumps.
Cell types
Practical cell typing:[2]
| Nucleus | Cell border | |
|---|---|---|
| Urothelium | Larger | Smooth/elliptical |
| Squamous epithelium | Smaller | Irregular/jagged |
Degenerative cells
Features:
- Nucleus protrudes through cell membrane.
- Chromatin degeration:
- "Cobweb" appearance - white holes/pale staining.
- White holes/frayed appearance.
- Small clumps of chromatin at the edge of nuclear membrane.
- Frayed cell membrane/irregular cell membrane.
- Vacuolated cytoplasm - "moth-eaten" appearance.
- Normal urothelial cytoplasm is dense and has no vacuoles.
Tabular DDx
Urothelial carcinoma versus benign urothelium
| Urothelial carcinoma | Benign urothelium | Use of feature | Utility | |
|---|---|---|---|---|
| Nuclear hyperchromasia | Present | Absent | r/i & r/o UC | Strong |
| Nuclear-to-cytoplasmic (NC) ratio | ~1:1.2 | ~1:2 | r/i & r/o UC; 1:>=2 suggests benign | Strong |
| Nuclear membrane irregularity (NMI) | +/- | Absent | r/i UC; presence strong predictor of malignancy (absence of NMI of little value) | Moderate |
| Cytoplasm | Green/grey | Green or grey & granular | r/o UC; granular (suggests degeneration) | Moderate |
| Coarse chromatin (CC) | Present | +/- | r/o UC; absence of CC suggest benign | Moderate |
| Nucleoli | In scattered cells | +/- in reactive | Not useful | Nil for diagnosing UC |
| Nuclear size | >2.5X normal | Usu. <=2X normal | Alone not much value, many large cells benign, many small cells malignant | Limited value, NC ratio much better measure |
Degeneration versus UC[3]
| Urothelial carcinoma | Degeneration | |
|---|---|---|
| Architecture | Usually single cells | Often small clusters |
| Cell borders | Sharp | Fuzzy/frayed |
| Cytoplasm | Green, solid | Grey, lacy/moth eaten |
| Nuclear membrane | Irregular | Usually regular |
| Chromatin | Granular/coarse | Granular/coarse |
Polyomavirus versus urothelial carcinoma
| Urothelial carcinoma | Polyoma virus | |
|---|---|---|
| Architecture | Often single cells | Single cells |
| Nucleus size | Often 3-4X normal urothelial cell | 2X normal urothelial cell nucleus (should not be larger) |
| Chromatin | Clumped or "dancing" | Ground glass inclusions/smudged |
| Nuclear membrane | Usually irregular | Regular |
Urothelial carcinoma vs adenocarcinoma
The default diagnosis is urothelial carcinoma as this is the most likely if there is no prior history of malignancy.
| Urothelial carcinoma | Adenocarcinoma | |
|---|---|---|
| Vacuoles | None | Present - mucin filled |
| Cytoplasm | Dense appearing | Fluffy |
| Chromatin | Coarse - clumped or "dancing" | Fine |
| History | None | History of adenocarcinoma |
| Nucleoli | Often present, multiple | Usually only one - every tumour cell |
Notes:
- Both have eccentric nuclei.
Human polyomavirus infection
Main article: Polyomavirus nephropathy
General
- Caused by Human polyomavirus, AKA BK virus.[4]
- Associated with immunosuppression/immunodeficiency.
- BK virus related to JC virus.
DDx:
- Urothelial carcinoma.
- May exist together with urothelial carcinoma ~ nuclei 2-4x the size of not infected malignant cells.[5]
Cytology
- "Decoy cells":
- Usually 2x the size of a normal urothelial cell nucleus.
- Single cells - important feature.
- Scant "degenerative-appearing" cytoplasm.
- High NC ratio.
- Intranuclear inclusions - key feature.
- Central smudging (or "wash-out") of the chromatin/"Ground glass" chromatin.
- Surrounded by clear halo just deep to the nuclear membrane.
- Nuclear membrane clumping.
Notes:
- Normal urothelial cell nucleus ~ 1.5X the size of a lymphocyte.
Image
IHC
- JC/BK virus.[8]
"Inflammation" in urine specimens
- One should resist the temptation to call "inflammation" in urine specimens, as processing concentrates the WBCs.
- If the quantity of WBCs is truly "excessive"... then it ought to be called.
Urothelial cell carcinoma
Main article: Urothelial cell carcinoma
- Abbreviated UCC.
General
- Very hard/impossible to diagnose low-grade UCC on cytology.
- The diagnosis of low-grade UCC is based on architecture (papillae).
Cytology
Features:[9]
- "Large nuclei" (3-4X the size of a normal urothelial cell) - low power feature.
- Hyperchromasia - low power feature.
- Irregular nuclear membrane - key feature.
- Increased NC ratio.
- Often uniform - when comparing malignant cells.
- Nuclear size variation, >=2X other malign. looking cells - very useful.
- +/-Large irregular nucleoli - common.
Minimal criteria:
- Criteria #2-4.
Notes:
- Coarse chromatin may be benign.
- Fine/non-granular chromatin suggests benign.
- One does not usually call squamous cell carcinoma on cytology.
- If features of squamous differentiation are present one calls urothelial carcinoma with squamous features.
DDx:
- Degeneration.
- Polyomavirus.
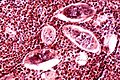
Schistosoma
- Associated with squamous cell carcinoma of the bladder.
Histology
Features of ova:
- Elliptical ~80 micrometres max dimension.
- S. haematobium has a "spike" approx. the size of a PMN.
Image
See also
References
- ↑ URL: https://paris.soc.wisc.edu/categories.htm. Accessed on: 25 March 2015.
- ↑ SM. 7 January 2010.
- ↑ Adapted from GS. 2 February 2010.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q26). ISBN 978-1416025887.
- ↑ Loghavi, S.; Bose, S. (Jul 2011). "Polyomavirus infection and urothelial carcinoma.". Diagn Cytopathol 39 (7): 531-5. doi:10.1002/dc.21490. PMID 20891007.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681-2 (Q26). ISBN 978-1416025887.
- ↑ SB. 27 January 2010.
- ↑ http://www.acta-cytol.com/toc/auto_abstract.php?id=22895
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.
- ↑ SM. 12 January 2010.