Ulcerative colitis
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Ulcerative colitis | |
|---|---|
| Diagnosis in short | |
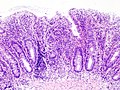
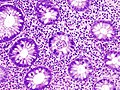
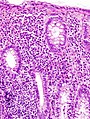
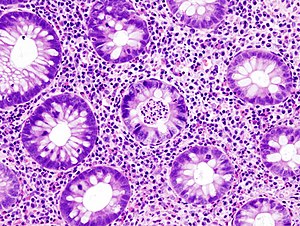 Active colitis in a case of ulcerative colitis. H&E stain. | |
|
| |
| LM | active changes (cryptitis, crypt abscesses, erosions), chronic changes (architectural distortion, basal plasmacytosis, foveolar metaplasia, Paneth cell metaplasia), lack of granulomas, mucin depletion (common) |
| LM DDx | Crohn's disease, infectious colitis, ischemic colitis, diversion colitis |
| Site | colon |
|
| |
| Associated Dx | primary sclerosing cholangitis, toxic megacolon |
| Clinical history | +/-FHx of IBD |
| Symptoms | +/-diarrhea +/-blood per rectum |
| Prevalence | uncommon |
| Clin. DDx | other types colitis (infectious, Crohn's disease, ischemic) |
| Treatment | medical and/or surgical |
Ulcerative colitis, abbreviated UC, is a type of inflammatory bowel disease.
General
- May be associated with toxic megacolon.
Epidemiology:
- Associated with primary sclerosing cholangitis.
- Appendicitis is considered protective against UC.[1][2]
- Smoking is protective; the opposite is true for Crohn's disease.[2]
Gross
- Conventionally considered to be contiguous, i.e. no "skip lesions", with rectal involvement being most severe.
- Dependent on the study one reads... rectal sparing may be seen in 15% of UC patients.[3]
Microscopic
Features:
- Inflammation:
- Active:
- Neutrophils:
- Intraepithelial (cryptitis).†
- Clusters in crypts (crypt abscesses).
- Erosions.
- Neutrophils:
- Chronic:
- Architectural distortion.
- Basal plasmacytosis.
- Foveolar metaplasia.
- Paneth cell metaplasia (distal).
- Lack of granulomas.
- Active:
- Mucin depletion - common in UC.[4]
Notes:
- †Neutrophils are usually numerous in the lamina propria in minimal/mild active inflammation.
- No full wall-thickness inflammation.
- Epithelial apoptosis correlated with inflammation.[5]
DDx:
- Crohn's disease.
- Infectious colitis.
- Ischemic colitis.
- Diversion colitis.
- Diverticular disease-associated colitis[6] restricted to areas with diverticular disease.
Images
Sign out
SIGMOID COLON, BIOPSY: - MODERATE ACTIVE COLITIS WITH CHRONIC CHANGES, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomata are identified. The sampled mucosa is diffusely inflamed. Crypt drop-out and architectural distortion are present. The findings are consistent with inflammatory bowel disease; however, an infectious etiology should be considered as a possibility.
SIGMOID COLON, BIOPSY: - MILD ACTIVE COLITIS, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomata are identified.
A. RIGHT COLON, BIOPSY: - MODERATE ACTIVE COLITIS, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. B. LEFT COLON, BIOPSY: - MODERATE-TO-SEVERE CHRONIC ACTIVE COLITIS, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomata are identified. The mucosa is diffusely inflamed. Architectural distortion is present in the left colon. The findings are consistent with ulcerative colitis; however, an infectious etiology should be considered as a possibility.
RECTUM, BIOPSY: - MODERATE DIFFUSE CHRONIC ACTIVE PROCTITIS. - NEGATIVE FOR DYSPLASIA. COMMENT: No definite granulomata are identified. Crypt drop-out is present. Within the proper clinical context, these are findings of inflammatory bowel disease.
Inactive disease
SIGMOID COLON, BIOPSY: - CHRONIC COLITIS, SEE COMMENT. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA. COMMENT: The sections show chronic changes (basal plasmacytosis, marked crypt architectural distortion, crypt branching); however, no active colitis is present. Also, lamina propria neutrophils, which are often easy to identify in an active colitis, are not apparent. Appreciable numbers of lamina propria eosinophils are present and focally intraepithelial. No granulomas are identified. Clinical correlation is required.
Surveillance
A. ASCENDING COLON, BIOPSY: - COLONIC MUCOSA WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA. B. TRANSVERSE COLON, BIOPSY: - COLONIC MUCOSA WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA. C. DESCENDING COLON, BIOPSY: - COLONIC MUCOSA WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA. D. SIGMOID COLON, BIOPSY: - COLONIC MUCOSA WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ACTIVE COLITIS. - NEGATIVE FOR DYSPLASIA. E. RECTUM, BIOPSY: - RECTAL MUCOSA WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ACTIVE PROCTITIS. - NEGATIVE FOR DYSPLASIA. COMMENT: Morphologically benign lymphoid aggregates are found focally. No granulomas are identified. Minimal architectural changes are seen focally.
A. CECUM, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. B. ASCENDING COLON, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. C. COLON, HEPATIC FLEXURE, BIOPSY, - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. D. TRANSVERSE COLON, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. E. COLON, SPLENIC FLEXURE, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. F. DESCENDING COLON, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. G. SIGMOID COLON, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. H. RECTUM, BIOPSY: - QUIESCENT INFLAMMATORY BOWEL DISEASE. - NEGATIVE FOR DYSPLASIA. COMMENT: No granulomas are identified. Mild architectural distortion is present. No active inflammation is identified. Scattered mucosal lymphoid nodules with germinal center formation are present.
Granulomas and inflamed crypts - clinically UC
A. CECUM, BIOPSY: - ACTIVE CECITIS, MILD. - SMALL MUCOSAL GRANULOMAS, SUPERFICIAL, SEE COMMENT. - NEGATIVE FOR DYSPLASIA. ... COMMENT - PART A: The small granulomas are mucosal and near, but not all adjacent to, inflamed crypts; this finding raises the possibility of Crohn's disease. It should be noted that mucosal granulomas may be seen in ulcerative colitis beside inflamed crypts. COMMENT - GENERAL: The inflammation is diffuse and chronic changes are seen throughout. Distal paneth cell metaplasia is present. The diffuse nature of the inflammation would be more in keeping with ulcerative colitis. Clinical correlation is required.
Micro
The sections show focal intraepithelial neutrophils (cryptitis). No crypt abscesses are identified. Granulation tissue is present. There is focal Paneth cell metaplasia and foveolar metaplasia. No granulomata are identified.
See also
References
- ↑ Beaugerie, L.; Sokol, H. (Aug 2009). "Appendicitis, not appendectomy, is protective against ulcerative colitis, both in the general population and first-degree relatives of patients with IBD.". Inflamm Bowel Dis. doi:10.1002/ibd.21064. PMID 19685454.
- ↑ 2.0 2.1 Timmer, A.; Obermeier, F. (2009). "Reduced risk of ulcerative colitis after appendicectomy.". BMJ 338: b225. PMID 19273505.
- ↑ Bernstein CN, Shanahan F, Anton PA, Weinstein WM (September 1995). "Patchiness of mucosal inflammation in treated ulcerative colitis: a prospective study". Gastrointest. Endosc. 42 (3): 232-7. PMID 7498688.
- ↑ McCormick, DA.; Horton, LW.; Mee, AS. (Feb 1990). "Mucin depletion in inflammatory bowel disease.". J Clin Pathol 43 (2): 143-6. PMID 2318990.
- ↑ Seidelin, JB.; Nielsen, OH. (2009). "Epithelial apoptosis: cause or consequence of ulcerative colitis?". Scand J Gastroenterol 44 (12): 1429-34. doi:10.3109/00365520903301212. PMID 19958058.
- ↑ Ludeman, L.; Warren, BF.; Shepherd, NA. (Aug 2002). "The pathology of diverticular disease.". Best Pract Res Clin Gastroenterol 16 (4): 543-62. PMID 12406450.