Difference between revisions of "Parathyroid glands"
Jump to navigation
Jump to search
(→IHC) |
|||
| Line 175: | Line 175: | ||
===IHC=== | ===IHC=== | ||
*GATA3 +ve (>98% | *GATA3 +ve (>98%<ref name=pmid27097544>{{Cite journal | last1 = Takada | first1 = N. | last2 = Hirokawa | first2 = M. | last3 = Suzuki | first3 = A. | last4 = Higuchi | first4 = M. | last5 = Kuma | first5 = S. | last6 = Miyauchi | first6 = A. | title = Diagnostic value of GATA-3 in cytological identification of parathyroid tissues. | journal = Endocr J | volume = 63 | issue = 7 | pages = 621-6 | month = Jul | year = 2016 | doi = 10.1507/endocrj.EJ15-0700 | PMID = 27097544 }}</ref>). | ||
*PTH -ve/+ve (~33%<ref name=pmid27097544/>). | *PTH -ve/+ve (~33%<ref name=pmid27097544/>). | ||
*Chromogranin A +ve (~80% <ref name=pmid27097544/>). | *Chromogranin A +ve (~80% <ref name=pmid27097544/>). | ||
Revision as of 19:09, 18 November 2019
The parathyroid glands are an endocrine organ that is important in calcium regulation. They often make an appearance in the context of thyroid surgery.
They produce parathyroid hormone (PTH). PTH acts to increase serum calcium and is important in the regulation of the calcium balance.
Clinical
Hyperparathyroidism
- Definition: increased secretion of parathyroid hormone (PTH).[1]
What PTH does:[1]
- Increase serum calcium.
- Decrease serum phosphate.
Classification
- Primary.
- Secondary.
- Tertiary.
Overview in a table
| Type | PTH | Calcium | Common causes |
|---|---|---|---|
| Primary hyperparathyroidism | high | high | parathyroid adenoma (~85-90% of cases), parathyroid hyperplasia (~10-15% of cases) |
| Secondary hyperparathyroidism | high | low or normal | chronic renal failure, vitamin D deficiency[2] |
| Tertiary hyperparathyroidism | high | high | persistent hyperparathyroidism after renal transplant;[3] arises in the context of secondary hyperparathyroidism[4] |
Genetics
Genes implicated in hyperparathyroidism:[5][6]
- MEN1.
- CASR.
- HRPT2/CDC73.
- CDKN1B.
- RET.
Hypercalcemia DDx
Mnemonic GRIMED:[7]
- Granulomatous disease (tuberculosis, sarcoidosis).
- Renal disease.
- Immobility.
- Malignancy (esp. squamous cell carcinoma, plasmacytoma).
- Endocrine (primary hyperparathyroidism, tertiary hyperparathyroidism, familial hypocalciuric hypercalcemia (FHH)).
- Drugs (thiazides ... others).
Note:
- Hyperparathyroidism and FHH are assoc. with an increased PTH.[8]
- Other causes are assoc. with a decreased PTH.
Primary hyperparathyroidism
Cause:[9]
- Parathyroid adenoma ~90%.
- Parathyroid hyperplasia ~10%.
- Parathyroid carcinoma ~1%.
Familial causes of primary hyperparathyroidism:
- MEN 1.
- MEN 2A.
- Familial hypocalciuric hypercalcemia.
- Autosomal dominant.
- CASR (calcium sensing receptor) gene defect.[10]
Classic manifestations moans, stones, bones, (abdominal) groans, psychiatric overtones.[11][12]
- Moans = bone pain.
- Stones = nephrolithiasis (kidney stones).
- Bones = bone pathology, e.g. osteitis fibrosa cystica.[13]
- Groans = constipation.
- Psychiatric overtones = CNS pathology.
- Can include: lethargy, fatigue, depression, memory loss, psychosis, ataxia, delirium, and coma.
Hypoparathyroidism
- Rare vis-à-vis hyperparathyroidism.
- Classically iatrogenic, i.e. the surgeon removing 'em.[8]
Other causes:[14]
- Autoimmune hypoparathyroidism.
- Autosomal dominat hypoparathyroidism.
- Familial isolated hypoparathyroidism.
- Congenital absence (DiGeorge syndrome).
- Drugs - proton pump inhibitors.[15][16]
Normal parathyroid glands
- The cytology is dealt with in normal parathyroid cytology.
General
- Identification of normal can be tricky.
Gross
- No distinctive features - surgeons thus send 'em to pathologists.
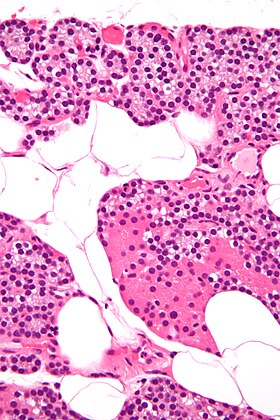
Microscopic
Features:[17]
- Low power:
- May vaguely resemble lymphoid tissue - may have hyperchromatic cytoplasm.
- Does not have follicular centres like a lymph node.
- May form gland-like structure and vaguely resemble the thyroid at low power.
- Cytoplasm may be clear[18] - key feature.
- Surrounded by a thin fibrous capsule.
- May vaguely resemble lymphoid tissue - may have hyperchromatic cytoplasm.
- High power:
- Mixed cell population:[19]
- Chief cells - predominant cell type, small, cytoplasm has variable staining (hyperchromatic-clear-eosinophilic).
- Oxyphil cells (acid staining cells[20]) - abundant cytoplasm.
- Adipocytes - dependent on age, body habitus, PT hormone, size of gland.[21]
- Increased with age, may be used to help differentiate from thyroid - key feature.
- Mixed cell population:[19]
Images
www:
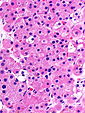
Parathyroid cell types
| Name | Staining (cytoplasm) | Quantity of cells | Cytoplasm (quantity) | Function | Image |
|---|---|---|---|---|---|
| (parathyroid) chief cells | intense hyperchromatic to eosinophilic (see note) | abundant | moderate | manufacture parathyroid hormone (PTH) |
|
| oxyphil cells | moderate/light hyperchromatic to eosinophilic | rare | abundant | ? |
Notes:
- Cytoplasmic staining varies considerably on H&E preparations - it may vary from hyperchromatic[22] to clear to eosinophilic.[23]
- Chief cells tend to stain more intensely than oxyphil cells.
Thyroid versus parathyroid
- Parathyroid cytoplasm:
- Hyperchromatic.
See: Parathyroid image (okstate.edu).
Parathyroid versus lymphoid tissue
- Parathyroid:
- No germinal centres.
- Gland-like/follicular-like arrangement may be present but usually much smaller than normal thyroid follicles.
- May be confused with thyroid microfollicules.
- Occasional cell with rim of clear cytoplasm (oxyphil?).
- Nuclei are different:
- Slightly larger than in lymphocytes (1.2-1.5x the size)
- Stippled chromatin (unlike lymphocytes).
Images:
IHC
Specific entities
Parathyroid hyperplasia
Main article: Parathyroid hyperplasia
Parathyroid adenoma
Main article: Parathyroid adenoma
Parathyroid carcinoma
Main article: Parathyroid carcinoma
See also
References
- ↑ 1.0 1.1 URL: http://emedicine.medscape.com/article/127351-overview. Accessed on: 24 January 2013.
- ↑ URL: http://emedicine.medscape.com/article/127351-overview#aw2aab6b5. Accessed on: 24 January 2013.
- ↑ URL: http://emedicine.medscape.com/article/127351-overview#aw2aab6b6. Accessed on: 24 January 2013.
- ↑ Duan, K.; Gomez Hernandez, K.; Mete, O. (Oct 2015). "Clinicopathological correlates of hyperparathyroidism.". J Clin Pathol 68 (10): 771-87. doi:10.1136/jclinpath-2015-203186. PMID 26163537.
- ↑ Starker, LF.; Akerström, T.; Long, WD.; Delgado-Verdugo, A.; Donovan, P.; Udelsman, R.; Lifton, RP.; Carling, T. (Apr 2012). "Frequent germ-line mutations of the MEN1, CASR, and HRPT2/CDC73 genes in young patients with clinically non-familial primary hyperparathyroidism.". Horm Cancer 3 (1-2): 44-51. doi:10.1007/s12672-011-0100-8. PMID 22187299.
- ↑ Hendy, GN.; Cole, DE. (2013). "Genetic defects associated with familial and sporadic hyperparathyroidism.". Front Horm Res 41: 149-65. doi:10.1159/000345675. PMID 23652676.
- ↑ Shiau, Carolyn; Toren, Andrew (2006). Toronto Notes 2006: Comprehensive Medical Reference (Review for MCCQE 1 and USMLE Step 2) (22nd edition (2006) ed.). Toronto Notes for Medical Students, Inc.. pp. Emerg.. ISBN 978-0968592861.
- ↑ 8.0 8.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1129. ISBN 978-1416031215.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1127. ISBN 978-1416031215.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 601199
- ↑ Lienert, D.; Rege, S. (Feb 2008). "Moans, stones, groans, bones and psychiatric overtones: lithium-induced hyperparathyroidism.". Aust N Z J Psychiatry 42 (2): 171-3. PMID 18350681.
- ↑ URL: http://www.usmleforum.com/files/forum/2010/1/505388.php. Accessed on: 4 December 2011.
- ↑ França, TC.; Griz, L.; Pinho, J.; Diniz, ET.; Andrade, LD.; Lucena, CS.; Beserra, SR.; Asano, NM. et al. (Apr 2011). "Bisphosphonates can reduce bone hunger after parathyroidectomy in patients with primary hyperparathyroidism and osteitis fibrosa cystica.". Rev Bras Reumatol 51 (2): 131-7. PMID 21584419.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1130. ISBN 978-1416031215.
- ↑ Deroux, A.; Khouri, C.; Chabre, O.; Bouillet, L.; Casez, O. (Oct 2014). "Severe acute neurological symptoms related to proton pump inhibitors induced hypomagnesemia responsible for profound hypoparathyroidism with hypocalcemia.". Clin Res Hepatol Gastroenterol 38 (5): e103-5. doi:10.1016/j.clinre.2014.03.005. PMID 24736034.
- ↑ Toh, JW.; Ong, E.; Wilson, R. (Aug 2014). "Hypomagnesaemia associated with long-term use of proton pump inhibitors.". Gastroenterol Rep (Oxf). doi:10.1093/gastro/gou054. PMID 25138239.
- ↑ http://www.medicalhistology.us/twiki/pub/Main/ChapterFourteenSlides/b56b_parathyroid_40x_he_labeled.jpg
- ↑ http://pathology.mc.duke.edu/research/Histo_course/parathyroid2.jpg
- ↑ http://www.bu.edu/histology/p/15002loa.htm
- ↑ http://dictionary.reference.com/search?q=oxyphil%20cell
- ↑ Iwasaki, A.; Shan, L.; Kawano, I.; Nakamura, M.; Utsuno, H.; Kobayashi, A.; Kuma, K.; Kakudo, K. (Jul 1995). "Quantitative analysis of stromal fat content of human parathyroid glands associated with thyroid diseases using computer image analysis.". Pathol Int 45 (7): 483-6. PMID 7551007.
- ↑ http://www.deltagen.com/target/histologyatlas/atlas_files/endocrine/parathyroid_and_thyroid_glands_20x.jpg
- ↑ http://instruction.cvhs.okstate.edu/Histology/HistologyReference/hrendo.htm
- ↑ Johnson, SJ.; Sheffield, EA.; McNicol, AM. (Apr 2005). "Best practice no 183. Examination of parathyroid gland specimens.". J Clin Pathol 58 (4): 338-42. doi:10.1136/jcp.2002.002550. PMC 1770637. PMID 15790694. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770637/.
- ↑ 25.0 25.1 25.2 Takada, N.; Hirokawa, M.; Suzuki, A.; Higuchi, M.; Kuma, S.; Miyauchi, A. (Jul 2016). "Diagnostic value of GATA-3 in cytological identification of parathyroid tissues.". Endocr J 63 (7): 621-6. doi:10.1507/endocrj.EJ15-0700. PMID 27097544.