Difference between revisions of "Parathyroid adenoma"
Jump to navigation
Jump to search
(+infobox) |
|||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Parathyroid adenoma intermed mag.jpg | |||
| Width = | |||
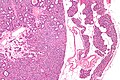
| Caption = Chief cell parathyroid adenoma (left of image) and unremarkable parathyroid gland (right of image). [[H&E stain]]. (WC) | |||
| Synonyms = | |||
| Micro = | |||
| Subtypes = | |||
| LMDDx = [[parathyroid hyperplasia]], [[parathyroid carcinoma]], [[lymph node]], [[thyroid gland]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[parathyroid gland]] ([[head and neck pathology|neck]]/[[mediastinum]]) | |||
| Assdx = | |||
| Syndromes = [[MEN 1|multiple endocrine neoplasia 1]], [[MEN 2A|multiple endocrine neoplasia 2A]] | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = increased parathyroid hormone, serum calcium increased | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = nodule (lymph node, other tumours), hyperparathyroidism ([[parathyroid hyperplasia]], [[parathyroid carcinoma]]), DDx of [[hypercalcemia]] | |||
| Tx = removal | |||
}} | |||
'''Parathyroid adenoma''' is a common benign pathology of the [[parathyroid gland]]. | '''Parathyroid adenoma''' is a common benign pathology of the [[parathyroid gland]]. | ||
| Line 4: | Line 35: | ||
*[[Clinical diagnosis]]. | *[[Clinical diagnosis]]. | ||
*Most common cause of [[primary hyperparathyroidism]].<ref name=Ref_PBoD8_1127>{{Ref PBoD8|1127}}</ref> | *Most common cause of [[primary hyperparathyroidism]].<ref name=Ref_PBoD8_1127>{{Ref PBoD8|1127}}</ref> | ||
*May be associated with [[MEN 1]] and [[MEN 2A]]. | *May be associated with [[MEN 1]] and [[MEN 2A]]. | ||
| Line 24: | Line 54: | ||
#*Uncommon.<ref name=pmid15579742>{{Cite journal | last1 = Fleischer | first1 = J. | last2 = Becker | first2 = C. | last3 = Hamele-Bena | first3 = D. | last4 = Breen | first4 = TL. | last5 = Silverberg | first5 = SJ. | title = Oxyphil parathyroid adenoma: a malignant presentation of a benign disease. | journal = J Clin Endocrinol Metab | volume = 89 | issue = 12 | pages = 5948-51 | month = Dec | year = 2004 | doi = 10.1210/jc.2004-1597 | PMID = 15579742 }}</ref> | #*Uncommon.<ref name=pmid15579742>{{Cite journal | last1 = Fleischer | first1 = J. | last2 = Becker | first2 = C. | last3 = Hamele-Bena | first3 = D. | last4 = Breen | first4 = TL. | last5 = Silverberg | first5 = SJ. | title = Oxyphil parathyroid adenoma: a malignant presentation of a benign disease. | journal = J Clin Endocrinol Metab | volume = 89 | issue = 12 | pages = 5948-51 | month = Dec | year = 2004 | doi = 10.1210/jc.2004-1597 | PMID = 15579742 }}</ref> | ||
#Mixed. | #Mixed. | ||
==Gross== | |||
*One parathyroid is big... the others are small. | |||
==Microscopic== | ==Microscopic== | ||
Revision as of 03:19, 11 September 2015
| Parathyroid adenoma | |
|---|---|
| Diagnosis in short | |
 Chief cell parathyroid adenoma (left of image) and unremarkable parathyroid gland (right of image). H&E stain. (WC) | |
| LM DDx | parathyroid hyperplasia, parathyroid carcinoma, lymph node, thyroid gland |
| Site | parathyroid gland (neck/mediastinum) |
|
| |
| Syndromes | multiple endocrine neoplasia 1, multiple endocrine neoplasia 2A |
|
| |
| Blood work | increased parathyroid hormone, serum calcium increased |
| Prognosis | benign |
| Clin. DDx | nodule (lymph node, other tumours), hyperparathyroidism (parathyroid hyperplasia, parathyroid carcinoma), DDx of hypercalcemia |
| Treatment | removal |
Parathyroid adenoma is a common benign pathology of the parathyroid gland.
General
- Clinical diagnosis.
- Most common cause of primary hyperparathyroidism.[1]
- May be associated with MEN 1 and MEN 2A.
MEN 1:
- Parathyroid adenoma.
- Pancreatic neuroendocrine tumour.
- Pituitary adenoma.
MEN 2A:
- Parathyroid adenoma.
- Medullary thyroid carcinoma.
- Pheochromocytoma.
Subtypes
Histologic subtyping:[2]
- Chief cell parathyroid adenoma.
- Common.
- Oxyphil parathyroid adenoma.
- Uncommon.[3]
- Mixed.
Gross
- One parathyroid is big... the others are small.
Microscopic
Features - general:
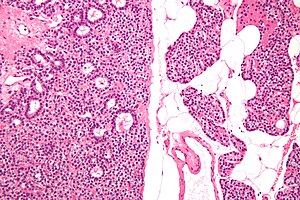
- Proliferation of parathyroid cells (chief cells, oxyphils or both) lacking adipose tissue.
- Classically have a rim of normal parathyroid gland around it[4] with adipose tissue.
Note:
- Generally, it is impossible to discern between parathyroid adenomas and parathyroid hyperplasias by histology alone.[4]
- One requires information of the size of the other glands to make the diagnosis.
DDx:
- Parathyroid hyperplasia - differentiated by clinical history.
- Parathyroid carcinoma - destructive invasion of surrounding tissue or far away mets, increased proliferative activity.
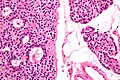
Chief cell parathyroid adenoma
Features:[1]
- Chief cells - key feature:
- Small central nucleus.
- Round with stippled chromatin - important.
- Moderate cytoplasm.
- Small central nucleus.
- +/-Scattered oxyphil cells:
- Large cells.
- Abundant cytoplasm.
- Architecture:
- Nests.
- Circular formations - often around capillaries (perivascular pseudorosettes).
Images
Oxyphil parathyroid adenoma
Features:[1]
- Oxyphil cells:
- Large cells.
- Abundant cytoplasm.
DDx:
- Hürthle cell adenoma of the thyroid gland.
Image:
Sign out
Note:
- One should not say "negative for malignancy".
Parathyroid Gland, Excision: - Chief cell parathyroid adenoma.
Parathyroid Gland, Excision: - Chief cell parathyroid adenoma with adjacent normal parathyroid tissue.
Parathyroid Gland (Submitted as "Right Superior Parathyroid Adenoma"), Excision: - Parathyroid adenoma with adjacent normal parathyroid tissue.
Block letters
PARATHRYOID GLAND, EXCISION: - CHIEF CELL PARATHYROID ADENOMA.
Micro
The section shows an adenoma consisting predominantly of chief cells. A rim of normal parathyroid is seen adjacent to the adenoma. A small amount of unremarkable adipose tissue is present.
See also
References
- ↑ 1.0 1.1 1.2 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1127. ISBN 978-1416031215.
- ↑ Moran, CA.; Suster, S. (Nov 2005). "Primary parathyroid tumors of the mediastinum: a clinicopathologic and immunohistochemical study of 17 cases.". Am J Clin Pathol 124 (5): 749-54. doi:10.1309/WJEL-N05L-9A06-9DU0. PMID 16203274.
- ↑ Fleischer, J.; Becker, C.; Hamele-Bena, D.; Breen, TL.; Silverberg, SJ. (Dec 2004). "Oxyphil parathyroid adenoma: a malignant presentation of a benign disease.". J Clin Endocrinol Metab 89 (12): 5948-51. doi:10.1210/jc.2004-1597. PMID 15579742.
- ↑ 4.0 4.1 Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 191. ISBN 978-0781767798.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/enfrm.html. Accessed on: 6 December 2010.