Difference between revisions of "Myeloproliferative neoplasms"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (→Essential thrombocythaemia: added) |
m |
||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Myeloproliferative neoplasms''', also '''myeloproliferative disorders''', are a group of indolent hematologic neoplasms characterized by clonal expansion of pluripotent hematopoietic progenitor. | '''Myeloproliferative neoplasms''', also '''myeloproliferative disorders''', are a group of indolent hematologic neoplasms characterized by clonal expansion of pluripotent hematopoietic progenitor. | ||
These should '''not''' be confused with ''[[myelodysplastic syndromes]]'' (MDS). | These should '''not''' be confused with ''[[myelodysplastic syndromes]]'' (MDS), the main difference is that MPNs produce functional haematological cells detectable on a complete blood count, whereas in MDS, hematopoisis is ineffective and is characterised by cytopenias. | ||
==Grouping== | ==Grouping== | ||
They include the following:<ref name=pmid15781101>{{cite journal |author=Baxter EJ, Scott LM, Campbell PJ, ''et al.'' |title=Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders |journal=Lancet |volume=365 |issue=9464 |pages=1054–61 |year=2005 |pmid=15781101 |doi=10.1016/S0140-6736(05)71142-9 |url=}}</ref> | They include the following:<ref name=pmid15781101>{{cite journal |author=Baxter EJ, Scott LM, Campbell PJ, ''et al.'' |title=Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders |journal=Lancet |volume=365 |issue=9464 |pages=1054–61 |year=2005 |pmid=15781101 |doi=10.1016/S0140-6736(05)71142-9 |url=}}</ref> | ||
*Polycythemia vera | *[[Chronic myeloid leukemia]] | ||
*Essential thrombocythemia. | *[[Polycythemia vera]] | ||
*Idiopathic myelofibrosis. | *[[Essential thrombocythemia]]. | ||
*[[Idiopathic myelofibrosis]]. | |||
==Clinic== | ==Clinic== | ||
* | * increase in blood count(s), dependent on type of MPN | ||
* anemia may occur in late stage disease or due leukemic transformation | |||
* pale skin | * pale skin | ||
* fatigue | * fatigue | ||
* enlarged spleen | * enlarged spleen | ||
* increased clotting | * increased clotting (i.e. thrombosis) | ||
==Polycythemia vera== | ==Polycythemia vera== | ||
| Line 23: | Line 24: | ||
*Typical course: | *Typical course: | ||
**Prodromal stadium: Mild erythrocytosis. | **Prodromal stadium: Mild erythrocytosis. | ||
**Polycythemic phase: | **Polycythemic phase: Increased RBC count. | ||
**Post-polycythemic ("spent") phase: Ineffective hematopoiesis, bone marrow fibrosis. | **Post-polycythemic ("spent") phase: Ineffective hematopoiesis, bone marrow fibrosis. | ||
*Transformation | *Transformation to [[AML]] possible (2-3%). | ||
===Morphology=== | ===Morphology=== | ||
| Line 31: | Line 32: | ||
*Many megakaryocytes in bone marrow section. | *Many megakaryocytes in bone marrow section. | ||
*Increased cellularity of bone marrow (35-100%). | *Increased cellularity of bone marrow (35-100%). | ||
*Teardrop-RBC cells ( | *Teardrop-RBC cells (dacrocytes) in late stage. | ||
*Fibrosis (reticulin stain). | *Fibrosis (reticulin stain). | ||
| Line 38: | Line 39: | ||
*Median age: 55 years. | *Median age: 55 years. | ||
*Mostly asymptomatic. | *Mostly asymptomatic. | ||
*Indolent course, long-term survival. Life-threatening | *Indolent course, long-term survival. Life-threatening thromboembolic epsisodes. | ||
===Morphology=== | ===Morphology=== | ||
*Thrombocytosis. | *Thrombocytosis. | ||
*Bone marrow normo- to slightly hypercellular. | *Bone marrow normo- to slightly hypercellular. | ||
*Large megakaryocytes in bone-marrow. | *Large hypersegmented megakaryocytes in bone-marrow. | ||
*Usually no BM fibrosis. | *Usually no BM fibrosis. | ||
Latest revision as of 16:44, 26 May 2018
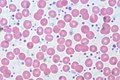
Myeloproliferative neoplasms, also myeloproliferative disorders, are a group of indolent hematologic neoplasms characterized by clonal expansion of pluripotent hematopoietic progenitor.
These should not be confused with myelodysplastic syndromes (MDS), the main difference is that MPNs produce functional haematological cells detectable on a complete blood count, whereas in MDS, hematopoisis is ineffective and is characterised by cytopenias.
Grouping
They include the following:[1]
Clinic
- increase in blood count(s), dependent on type of MPN
- anemia may occur in late stage disease or due leukemic transformation
- pale skin
- fatigue
- enlarged spleen
- increased clotting (i.e. thrombosis)
Polycythemia vera
- ICD-O: 9950/3
- Median age: 60 years.
- Median survival: >10years.
- Typical course:
- Prodromal stadium: Mild erythrocytosis.
- Polycythemic phase: Increased RBC count.
- Post-polycythemic ("spent") phase: Ineffective hematopoiesis, bone marrow fibrosis.
- Transformation to AML possible (2-3%).
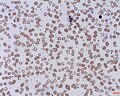
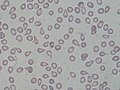
Morphology
- Panmyelosis.
- Many megakaryocytes in bone marrow section.
- Increased cellularity of bone marrow (35-100%).
- Teardrop-RBC cells (dacrocytes) in late stage.
- Fibrosis (reticulin stain).
Essential thrombocythaemia
- ICD-O: 9962/3
- Median age: 55 years.
- Mostly asymptomatic.
- Indolent course, long-term survival. Life-threatening thromboembolic epsisodes.
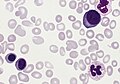
Morphology
- Thrombocytosis.
- Bone marrow normo- to slightly hypercellular.
- Large hypersegmented megakaryocytes in bone-marrow.
- Usually no BM fibrosis.
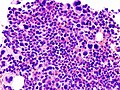
Images
Molecular
- BCR-ABL1 negative (DDx: Leukemia (BCR-ABL1 positive))
- A specific JAK2 mutation (Val617Phe) in seen in a group of patients.[1][2]
- In JAK2-negative cases, CALR or MPL-Mutations are often found.[3]
See also
References
- ↑ 1.0 1.1 Baxter EJ, Scott LM, Campbell PJ, et al. (2005). "Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders". Lancet 365 (9464): 1054–61. doi:10.1016/S0140-6736(05)71142-9. PMID 15781101.
- ↑ Steensma DP, Dewald GW, Lasho TL, et al. (August 2005). "The JAK2 V617F activating tyrosine kinase mutation is an infrequent event in both "atypical" myeloproliferative disorders and myelodysplastic syndromes". Blood 106 (4): 1207–9. doi:10.1182/blood-2005-03-1183. PMC 1895198. PMID 15860661. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1895198/.
- ↑ Nangalia, J.; Green, TR. (Dec 2014). "The evolving genomic landscape of myeloproliferative neoplasms.". Hematology Am Soc Hematol Educ Program 2014 (1): 287-96. doi:10.1182/asheducation-2014.1.287. PMID 25696868.