Difference between revisions of "Meningioma"
Jensflorian (talk | contribs) (→Molecular: update) |
Jensflorian (talk | contribs) (→IHC: update) |
||
| Line 370: | Line 370: | ||
*PR +ve (approx. 75%, expression decreases from grade I to III). | *PR +ve (approx. 75%, expression decreases from grade I to III). | ||
*SSTR2A +ve (approx. 95%). | *SSTR2A +ve (approx. 95%). | ||
*S100 variable (up to 35% cases, usually patchy). | *S100 variable (up to 35% cases, usually patchy).<ref>{{cite journal |vauthors=Behling F, Fodi C, Skardelly M, Paulsen F, Tabatabai G, Honegger J, Tatagiba M, Schittenhelm J |title=The prognostic role of the immunohistochemical expression of S100 in meningiomas |journal=J Cancer Res Clin Oncol |volume= |issue= |pages= |date=July 2022 |pmid=35838837 |doi=10.1007/s00432-022-04186-9 |url=}}</ref> | ||
*SOX10 -ve. | *SOX10 -ve. | ||
*GFAP -ve. | *GFAP -ve. | ||
*CD34 usu. -ve (approx 8% cases positive). | *CD34 usu. -ve (approx 8% cases positive). | ||
*CD13 +ve.<ref>{{cite journal |vauthors=Marletta S, Luchini C, Sperandio N, Torresani E, Sorio A, Girolami I, Scarpa A, Eccher A, Ghimenton C |title=CD13 is a useful tool in the differential diagnosis of meningiomas with potential biological and prognostic implications |journal=Virchows Arch |volume=480 |issue=6 |pages=1223–1230 |date=June 2022 |pmid=35212813 |pmc=9184408 |doi=10.1007/s00428-022-03304-9 |url=}}</ref> | |||
*Other CKs usually -ve (approx 6% cases positive, mostly secretory meningiomas). | *Other CKs usually -ve (approx 6% cases positive, mostly secretory meningiomas). | ||
Latest revision as of 14:13, 19 September 2022
| Meningioma | |
|---|---|
| Diagnosis in short | |
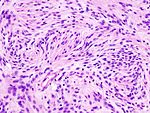
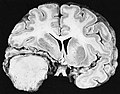
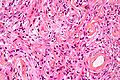
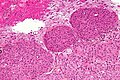
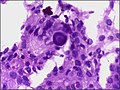
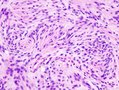
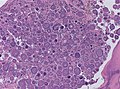
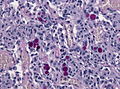
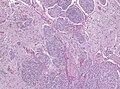
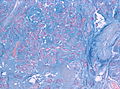
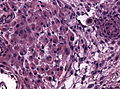
 Meningioma. HPS stain. | |
|
| |
| LM | whorled appearance, calcification - psammomatous, +/-nuclear pseudoinclusions |
| Subtypes | Grade I (meningothelial, fibrous, transistional, psammomatous, angiomatous, microcystic, secretory, lymphoplasmacyte-rich, metaplastic), Grade II (invasive, clear cell, chordoid), Grade III (papillary, rhabdoid) |
| LM DDx | schwannoma, solitary fibrous tumour, hemangiopericytoma, others |
| IHC | EMA +ve, keratins usu. -ve, CD34 -ve/+ve, S-100 -ve (usu.), PR +ve (-ve in more aggressive ones) |
| Site | see CNS tumours |
|
| |
| Syndromes | neurofibromatosis 2, nevoid basal cell carcinoma syndrome |
|
| |
| Clinical history | +/-radiation |
| Prevalence | common |
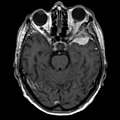
| Radiology | extra-axial, intradural lesion, dural tail sign (on MRI) |
| Prognosis | usually benign, dependent on grade |
| Clin. DDx | dependent on site - see CNS tumours |
| Treatment | surgical removal |
Meningioma a very common tumour in neuropathology.
General
Prevalence
- Most common primary brain tumour.[1]
- May be caused by prior radiation.[2]
- Women develop meningioma twice as likely as men.[3]
- More than 90% are solitary.
Prognosis
- Most are benign - usu. a good prognosis.
- Even benign tumors may show extensive local spread - considerable morbidity and mortality.
- Metastases are rare and then usu. after surgery.
- May be malignant - bad prognosis.
- Factors associated with unfavourable prognosis:
Genetics
- May be seen in genetic disorders such as:
- Neurofibromatosis 2 (NF2).[7]
- Nevoid basal cell carcinoma syndrome (Gorlin syndrome).[8][9]
Quick overview
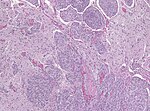
| Name | Histologic criteria | Subtypes | Image |
|---|---|---|---|
| Classic, WHO I | less then 4 mit/10 HPF and no atypia | meningeothelial, fibroblastic, transitional, psammomatous, angiomatous, microcytsic, secretory, lymphoplasmacyte-rich, metaplastic | |
| Atypical, WHO II | brain invasion, 4 or more mit/10 HPF, or 3 of the following: necrosis, increased cellularity, high nuc:cyto ratio, nucleoli, sheeting | chordoid, clear cell | |
| Anaplastic, WHO III | 20 or more mitoses/10 HPF, morphologiy similiar to carcinoma or sarcoma | rhabdoid, papillary |
Gross/Radiology
- Extra-axial, intradural.
- Can be extradural - very rare.[10]
- Dural tail sign (DTS) on MRI.[11][12]
- +/-Hyperostosis.
- Associated with invasion into the skull in ~20% of cases.[15]
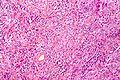
Microscopic
Features (memory device WCN):
- Whorled appearance - key feature.
- Calcification, psammomatous (target-like appearance; (tight) onion skin).
- +/-Nuclear pseudoinclusions - focal nuclear clearing with a sharp interface to unremarkable chromatin.
Notes:
- May involute into benign sclerotic tissue.[16]
- Thick-walled blood vessels -> think schwannoma.
DDx:
- Schwannoma - especially at CP angle.
- Solitary fibrous tumour.
- Hemangiopericytoma.
- Others - see subtypes.
Images
www:
Morphologic subtypes
- Many subtypes exist.[17]
- The histologic subtypes generally don't have much prognostic significance.
- Some subtypes are high grade by definition; also see histologic grading.
Grade I
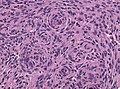
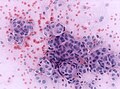
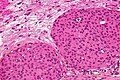
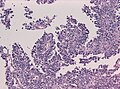
Meningothelial meningioma
- Most common.
Microscopic:
- Syncytial, nuclear clearing (pseudoinclusions).
- Whorls, Onion bulb formations.
- Few psammoma bodies.
Molecular:
- AKT E17K mutations.[18]
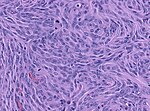
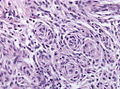
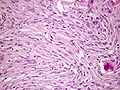
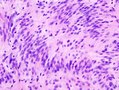
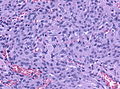
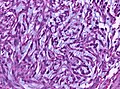
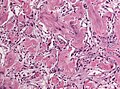
Fibrous meningioma
- AKA fibroblastic meningioma.
- Not collagen... but looks like it.
- It is really laminin or fibronectin.
- Spindle cells in parallel bundles.
- Few to none whorl formations.
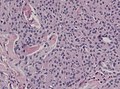
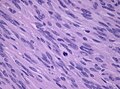
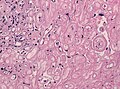
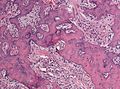
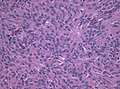
Transitional meningioma
- AKA mixed.
- Common.
- Lobular and fasicular growth patterns coexist.
- Usu. a mixture of meningeothelial and fibromatous meningioma
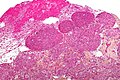
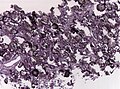
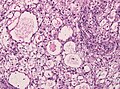
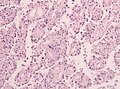
Psammomatous meningioma
Microscopic:
- Psammoma bodies dominate over tumor cells.
- Irregular calcifications (confluent psammoma bodies).
- Usually found in spinal cord.
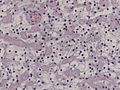
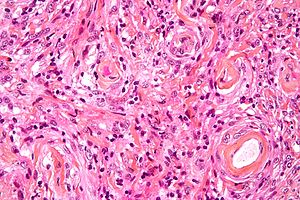
Angiomatous meningioma
- AKA vascular.
- May bleed like stink.
- May show extensive edema.
- Hyalinized vessels dominate over tumor cells.
- Degenerative nuclear atypia.
DDx:
- Vascular malformatons
- Hemangioblastoma
Microcystic meningioma
Microscopic:
- Cystic appearance.
- Increased cytologic pleomorphism of the elongated cells.
DDx:
- Clear cell meningioma
- Hemangioblastoma
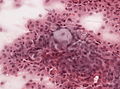
Secretory meningioma
- Associated with brain edema; may have a worse outcome.
Microscopic:[19]
Molecular:
- Combined KLF4 K409Q and TRAF7 mutations.[20]
DDx:
- Metastatic mucinous adenocarcinoma.
- Pituitary adenoma
Images:
Lymphoplasmacyte-rich meningioma
Microscopic:
- Lymphocytes.
- Plasma cells.
Images:
- Lymphoplasmacyte-rich meningioma - case 1 - several images (upmc.edu).
- Lymphoplasmacyte-rich meningioma - case 2 - several images (upmc.edu).
- Lymphoplasmacyte-rich meningioma - case 3 - several images (upmc.edu).
Metaplastic meningioma
- No clinical significance.
- Probably do not represent true metaplasia in all cases.
- Clincal information is rquired to distinguish between bone invasion and meningiomas with bone formation.
Microscopic:
- Cartilage or bone formation.
- Myxoid or xanthomatous changes.
Grade II
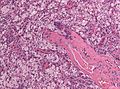
Brain invasive meningioma
- Invades the brain (irregular, tongue-like).
- Absence of leptomeningeal layer.
- Brain invasion can be present in grade I tumors, these are then classified as "atypical", ie. as grade II tumors.
- The prognostic significance of brain invasion is still unclear, some studies do not show a course similiar to grade II meningiomas.[22][23][24]
Images:
Clear cell meningioma
Epidemiology:
- Usu. spinal cord.[25]
Microscopic:
- Clear cells - contain glycogen (PAS +ve).
Molecular:
- SMARCE1 mutations.[26]
Images:
Chordoid meningioma
- Chordoma-like.
Microscopic:
- Myxoid appearance.
Image:
Grade III
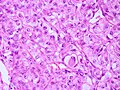
Papillary meningioma
Microscopic:
- discohesive meningothelial tumour cells around a fibrovascular core.
- perivascular pseudorosettes.
Rhabdoid meningioma
Microscopic:
- Rhabdoid appearance (abundant cytoplasm).
- Cross-striations.
www:
- Rhabdoid meningioma - case 1 - several images (upmc.edu).
- Rhabdoid meningioma - case 2 - several images (upmc.edu).
Other morphological variants
These are currently not listed in the WHO as separate entities.
Histologic grading
Grading:[17]
- Grade 1:
- Low mitotic rate (< 4 mitoses/10 HPF - for whatever HPF means, see HPFitis).
- Excludes clear cell, chordoid, papillary, and rhabdoid subtypes.
- Grade 2 (either #1, #2 or #3):
- Brain-invasive meningioma.
- Invasion of meningioma into brain.
- Meninogioma with entraped GFAP +ve tissue.
- Invasion of meningioma into brain.
- Atypical meningioma (by histomorphology) - either A or B.
- A. Intermediate mitotic rate (>= 4 mitoses/10 HPF - for whatever HPF means, see HPFitis.)
- B. Three of the following five features:
- Clear cell or chordoid subtype.
- Brain-invasive meningioma.
- Grade 3 (either of the following):
- High mitotic rate (>=20 mitoses/10 HPF - for whatever HPF means, see HPFitis.)
- "Frank anaplasia"; marked nuclear atypia.
- Papillary or rhabdoid subtype.
Notes:
- Grade II soft criteria memory device HMNs: hypercellular, macronucleoli, NC ratio increased, necrosis, sheeting.
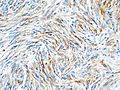
IHC
- EMA +ve (approx. 90%).[30]
- PR +ve (approx. 75%, expression decreases from grade I to III).
- SSTR2A +ve (approx. 95%).
- S100 variable (up to 35% cases, usually patchy).[31]
- SOX10 -ve.
- GFAP -ve.
- CD34 usu. -ve (approx 8% cases positive).
- CD13 +ve.[32]
- Other CKs usually -ve (approx 6% cases positive, mostly secretory meningiomas).
Molecular
Non-syndromal meningiomas may show AKT1/TRAF7, SMO, KLF4/TRAF7, and PIK3CA mutations (1/3 of cases).[33]
- AKT/TRAF7 mutations are usually basal and associated with meningothelial histology.
- KLF4/TRAF7 mutations are highly specific for secretory histology.
- TRAF7 mutations are the first step and occur thorughout the WD40 domain. [34]
Intraventricular meningiomas have NF2 mutations. [35]
Several inherited diseases are associated with meningiomas:
- Neurofibromatosis type II[36]
- Germline SMARCE1 and SMARCB1 mutations[37][38]
- Loss of SUFU (SHH-Pathway).[39]
- Rare YAP1 fusions in a subset of pediatric meningioma (HIPPO pathyway).[40]
Methylation profiling distinguishes two major groups with six distinct clinically relevant methylation classes.[41]
DDx of meningioma & IHC[42]
- S-100 strong +ve - schwannoma.
- +ve in ~80% of fibrous meningiomas.
- CD34 +ve - solitary fibrous tumour.
- +ve in ~60% of fibrous meningiomas.
- STAT6 nuclear +ve: solitary fibrous tumour.
- EMA +ve in ~30% of solitary fibrous tumour/hemangiopericytoma.
- Claudin-1 - new kid on the block: +ve in meningioma, but low sensitivity.
- SSTR2A +ve in meningioma, usu. -ve in Perineurioma [43]
- Progesterone receptor: +ve in mostly grade I and meningeothelial tumors.[44]
- Pulmonary meningothelial-like nodule
A standard work-up
- Ki-67 >5-10% - predicts re-occurrence.[45]
- PR (progesterone receptor) +ve in > 80% of meningiomas.[46]
- Loss of PR staining predicts recurrence.
- Strong association with tumour grade:[47]
- Low WHO grade tumours usu. +ve.
- High WHO grade tumours usu. -ve.
See also
References
- ↑ Rogers, L.; Barani, I.; Chamberlain, M.; Kaley, TJ.; McDermott, M.; Raizer, J.; Schiff, D.; Weber, DC. et al. (Oct 2014). "Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review.". J Neurosurg: 1-20. doi:10.3171/2014.7.JNS131644. PMID 25343186.
- ↑ Baldi, I.; Engelhardt, J.; Bonnet, C.; Bauchet, L.; Berteaud, E.; Grüber, A.; Loiseau, H. (Sep 2014). "Epidemiology of meningiomas.". Neurochirurgie. doi:10.1016/j.neuchi.2014.05.006. PMID 25249493.
- ↑ Wiemels, J.; Wrensch, M.; Claus, EB. (Sep 2010). "Epidemiology and etiology of meningioma.". J Neurooncol 99 (3): 307-14. doi:10.1007/s11060-010-0386-3. PMID 20821343.
- ↑ Shankar, GM.; Abedalthagafi, M.; Vaubel, RA.; Merrill, PH.; Nayyar, N.; Gill, CM.; Brewster, R.; Bi, WL. et al. (04 2017). "Germline and somatic BAP1 mutations in high-grade rhabdoid meningiomas.". Neuro Oncol 19 (4): 535-545. doi:10.1093/neuonc/now235. PMID 28170043.
- ↑ Sahm, F.; Schrimpf, D.; Olar, A.; Koelsche, C.; Reuss, D.; Bissel, J.; Kratz, A.; Capper, D. et al. (May 2016). "TERT Promoter Mutations and Risk of Recurrence in Meningioma.". J Natl Cancer Inst 108 (5). doi:10.1093/jnci/djv377. PMID 26668184.
- ↑ Katz, LM.; Hielscher, T.; Liechty, B.; Silverman, J.; Zagzag, D.; Sen, R.; Wu, P.; Golfinos, JG. et al. (Apr 2018). "Loss of histone H3K27me3 identifies a subset of meningiomas with increased risk of recurrence.". Acta Neuropathol. doi:10.1007/s00401-018-1844-9. PMID 29627952.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/neurotest/Q13-Ans.htm. Accessed on: 26 October 2010.
- ↑ Kimonis, VE.; Mehta, SG.; Digiovanna, JJ.; Bale, SJ.; Pastakia, B.. "Radiological features in 82 patients with nevoid basal cell carcinoma (NBCC or Gorlin) syndrome.". Genet Med 6 (6): 495-502. doi:10.109701.GIM.0000145045.17711.1C. PMID 15545745.
- ↑ Lee, CW.; Tan, TC. (Feb 2014). "Meningioma associated with Gorlin's syndrome.". J Clin Neurosci 21 (2): 349-50. doi:10.1016/j.jocn.2013.02.033. PMID 24100109.
- ↑ URL: http://path.upmc.edu/cases/case702.html. Accessed on: 2 February 2012.
- ↑ Ikeda, D.; Chiocca, EA. (Oct 2012). "Editorial: dural tail sign.". J Neurosurg 117 (4): 643-4. doi:10.3171/2012.2.JNS12266. PMID 22839655.
- ↑ Wen, M.; Jung, S.; Moon, KS.; Pei, J.; Lee, KH.; Jin, SG.; Li, SY.; Ryu, HH. (Dec 2014). "Immunohistochemical profile of the dural tail in intracranial meningiomas.". Acta Neurochir (Wien) 156 (12): 2263-73. doi:10.1007/s00701-014-2216-4. PMID 25238986.
- ↑ Aoki, S.; Sasaki, Y.; Machida, T.; Tanioka, H.. "Contrast-enhanced MR images in patients with meningioma: importance of enhancement of the dura adjacent to the tumor.". AJNR Am J Neuroradiol 11 (5): 935-8. PMID 2120998.
- ↑ Qi, ST.; Liu, Y.; Pan, J.; Chotai, S.; Fang, LX. (Oct 2012). "A radiopathological classification of dural tail sign of meningiomas.". J Neurosurg 117 (4): 645-53. doi:10.3171/2012.6.JNS111987. PMID 22839654.
- ↑ Goyal, N.; Kakkar, A.; Sarkar, C.; Agrawal, D.. "Does bony hyperostosis in intracranial meningioma signify tumor invasion? A radio-pathologic study.". Neurol India 60 (1): 50-4. doi:10.4103/0028-3886.93589. PMID 22406780.
- ↑ URL: http://radiographics.rsna.org/content/23/3/785.long. Accessed on: 3 November 2010.
- ↑ 17.0 17.1 Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 194. ISBN 978-0443069826.
- ↑ Sahm, F.; Bissel, J.; Koelsche, C.; Schweizer, L.; Capper, D.; Reuss, D.; Böhmer, K.; Lass, U. et al. (Nov 2013). "AKT1E17K mutations cluster with meningothelial and transitional meningiomas and can be detected by SFRP1 immunohistochemistry.". Acta Neuropathol 126 (5): 757-62. doi:10.1007/s00401-013-1187-5. PMID 24096618.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com04/Com405-1-Diss.htm. Accessed on: 12 October 2011.
- ↑ Reuss, DE.; Piro, RM.; Jones, DT.; Simon, M.; Ketter, R.; Kool, M.; Becker, A.; Sahm, F. et al. (Mar 2013). "Secretory meningiomas are defined by combined KLF4 K409Q and TRAF7 mutations.". Acta Neuropathol 125 (3): 351-8. doi:10.1007/s00401-013-1093-x. PMID 23404370.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com04/Com405-1-Diss.htm. Accessed on: 3 January 2012.
- ↑ Baumgarten, P.; Gessler, F.; Schittenhelm, J.; Skardelly, M.; Tews, DS.; Senft, C.; Dunst, M.; Imoehl, L. et al. (Sep 2016). "Brain invasion in otherwise benign meningiomas does not predict tumor recurrence.". Acta Neuropathol 132 (3): 479-81. doi:10.1007/s00401-016-1598-1. PMID 27464983.
- ↑ Brokinkel, B.; Hess, K.; Mawrin, C. (Apr 2017). "Brain invasion in Meningiomas - Clinical considerations and impact of neuropathological evaluation: A systematic Review.". Neuro Oncol. doi:10.1093/neuonc/nox071. PMID 28419308.
- ↑ Pizem, J.; Velnar, T.; Prestor, B.; Mlakar, J.; Popovic, M.. "Brain invasion assessability in meningiomas is related to meningioma size and grade, and can be improved by extensive sampling of the surgically removed meningioma specimen.". Clin Neuropathol 33 (5): 354-63. doi:10.5414/NP300750. PMID 25034703.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 200. ISBN 978-0443069826.
- ↑ Smith, MJ.; Wallace, AJ.; Bennett, C.; Hasselblatt, M.; Elert-Dobkowska, E.; Evans, LT.; Hickey, WF.; van Hoff, J. et al. (Dec 2014). "Germline SMARCE1 mutations predispose to both spinal and cranial clear cell meningiomas.". J Pathol 234 (4): 436-40. doi:10.1002/path.4427. PMID 25143307.
- ↑ Zunarelli, E.; Tallarico, E.; Valentini, A.; Maiorana, A. (2010). "Oncocytic meningioma: study of eight new cases and analysis of 13 reported cases.". Pathology 42 (6): 587-9. doi:10.3109/00313025.2010.508740. PMID 20854082.
- ↑ Haberler, C.; Jarius, C.; Lang, S.; Rössler, K.; Gruber, A.; Hainfellner, JA.; Budka, H. (Feb 2002). "Fibrous meningeal tumours with extensive non-calcifying collagenous whorls and glial fibrillary acidic protein expression: the whorling-sclerosing variant of meningioma.". Neuropathol Appl Neurobiol 28 (1): 42-7. PMID 11849562.
- ↑ Liverman, C.; Mafra, M.; Chuang, SS.; Shivane, A.; Chakrabarty, A.; Highley, R.; Hilton, DA.; Byrne, NP. et al. (Aug 2015). "A clinicopathologic study of 11 rosette-forming meningiomas: a rare and potentially confusing pattern.". Acta Neuropathol 130 (2): 311-3. doi:10.1007/s00401-015-1456-6. PMID 26106026.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 13. ISBN 978-0443069826.
- ↑ "The prognostic role of the immunohistochemical expression of S100 in meningiomas". J Cancer Res Clin Oncol. July 2022. doi:10.1007/s00432-022-04186-9. PMID 35838837.
- ↑ "CD13 is a useful tool in the differential diagnosis of meningiomas with potential biological and prognostic implications". Virchows Arch 480 (6): 1223–1230. June 2022. doi:10.1007/s00428-022-03304-9. PMC 9184408. PMID 35212813. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9184408/.
- ↑ Clark, VE.; Erson-Omay, EZ.; Serin, A.; Yin, J.; Cotney, J.; Ozduman, K.; Avşar, T.; Li, J. et al. (Mar 2013). "Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO.". Science 339 (6123): 1077-80. doi:10.1126/science.1233009. PMID 23348505.
- ↑ "Single-cell DNA sequencing reveals order of mutational acquisition in TRAF7/AKT1 and TRAF7/KLF4 mutant meningiomas". Acta Neuropathol 144 (4): 799–802. October 2022. doi:10.1007/s00401-022-02485-6. PMID 35984495.
- ↑ "Intraventricular meningiomas frequently harbor NF2 mutations but lack common genetic alterations in TRAF7, AKT1, SMO, KLF4, PIK3CA, and TERT". Acta Neuropathol Commun 7 (1): 140. August 2019. doi:10.1186/s40478-019-0793-4. PMC 6716845. PMID 31470906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6716845/.
- ↑ Fontaine, B.; Rouleau, GA.; Seizinger, BR.; Menon, AG.; Jewell, AF.; Martuza, RL.; Gusella, JF. (1991). "Molecular genetics of neurofibromatosis 2 and related tumors (acoustic neuroma and meningioma).". Ann N Y Acad Sci 615: 338-43. PMID 2039155.
- ↑ Smith, MJ.; O'Sullivan, J.; Bhaskar, SS.; Hadfield, KD.; Poke, G.; Caird, J.; Sharif, S.; Eccles, D. et al. (Mar 2013). "Loss-of-function mutations in SMARCE1 cause an inherited disorder of multiple spinal meningiomas.". Nat Genet 45 (3): 295-8. doi:10.1038/ng.2552. PMID 23377182.
- ↑ van den Munckhof, P.; Christiaans, I.; Kenter, SB.; Baas, F.; Hulsebos, TJ. (Feb 2012). "Germline SMARCB1 mutation predisposes to multiple meningiomas and schwannomas with preferential location of cranial meningiomas at the falx cerebri.". Neurogenetics 13 (1): 1-7. doi:10.1007/s10048-011-0300-y. PMID 22038540.
- ↑ Aavikko, M.; Li, SP.; Saarinen, S.; Alhopuro, P.; Kaasinen, E.; Morgunova, E.; Li, Y.; Vesanen, K. et al. (Sep 2012). "Loss of SUFU function in familial multiple meningioma.". Am J Hum Genet 91 (3): 520-6. doi:10.1016/j.ajhg.2012.07.015. PMID 22958902.
- ↑ Sievers, P.; Chiang, J.; Schrimpf, D.; Stichel, D.; Paramasivam, N.; Sill, M.; Gayden, T.; Casalini, B. et al. (Nov 2019). "YAP1-fusions in pediatric NF2-wildtype meningioma.". Acta Neuropathol. doi:10.1007/s00401-019-02095-9. PMID 31734728.
- ↑ Sahm, F.; Schrimpf, D.; Stichel, D.; Jones, DT.; Hielscher, T.; Schefzyk, S.; Okonechnikov, K.; Koelsche, C. et al. (Mar 2017). "DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis.". Lancet Oncol. doi:10.1016/S1470-2045(17)30155-9. PMID 28314689.
- ↑ Hahn HP, Bundock EA, Hornick JL (February 2006). "Immunohistochemical staining for claudin-1 can help distinguish meningiomas from histologic mimics". Am. J. Clin. Pathol. 125 (2): 203–8. doi:10.1309/G659-FVVB-MG7U-4RPQ. PMID 16393681. http://ajcp.ascpjournals.org/content/125/2/203.full.pdf.
- ↑ Agaimy, A.; Buslei, R.; Coras, R.; Rubin, BP.; Mentzel, T. (Jul 2014). "Comparative study of soft tissue perineurioma and meningioma using a five-marker immunohistochemical panel.". Histopathology 65 (1): 60-70. doi:10.1111/his.12366. PMID 24393170.
- ↑ Grunberg, SM. (1991). "The role of progesterone receptors in meningioma.". Cancer Treat Res 58: 127-37. PMID 1683782.
- ↑ Croul, SE. 8 November 2010.
- ↑ Takei, H.; Buckleair, LW.; Powell, SZ. (Feb 2008). "Immunohistochemical expression of apoptosis regulating proteins and sex hormone receptors in meningiomas.". Neuropathology 28 (1): 62-8. doi:10.1111/j.1440-1789.2007.00852.x. PMID 18021195.
- ↑ Tao, Y.; Liang, G.; Li, Z.; Wang, Y.; Wu, A.; Wang, H.; Lu, Y.; Liu, Z. et al. (May 2012). "Clinical features and immunohistochemical expression levels of androgen, estrogen, progesterone and Ki-67 receptors in relationship with gross-total resected meningiomas relapse.". Br J Neurosurg. doi:10.3109/02688697.2012.685780. PMID 22616825.