Difference between revisions of "Lymphocytic colitis"
Jump to navigation
Jump to search
(tweak) |
|||
| Line 72: | Line 72: | ||
==Microscopic== | ==Microscopic== | ||
Features: | Features: | ||
*Lots of intraepithelial lymphocytes (>=20/100 lymphocytes/surface epithelial cells<ref name=pmid19109861>{{cite journal |author=Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S |title=Diagnosis and management of microscopic colitis |journal=World J. Gastroenterol. |volume=14 |issue=48 |pages=7280-8 |year=2008 |month=December |pmid=19109861 | PMC = 2778111 |doi= |url=http://www.wjgnet.com/1007-9327/14/7280.asp}}</ref>) and | *Lots of [[intraepithelial lymphocytes]] (>=20/100 lymphocytes/surface epithelial cells<ref name=pmid19109861>{{cite journal |author=Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S |title=Diagnosis and management of microscopic colitis |journal=World J. Gastroenterol. |volume=14 |issue=48 |pages=7280-8 |year=2008 |month=December |pmid=19109861 | PMC = 2778111 |doi= |url=http://www.wjgnet.com/1007-9327/14/7280.asp}}</ref>) and | ||
*Lymphocytes in the lamina propria. | *Lymphocytes in the lamina propria. | ||
Latest revision as of 14:29, 25 May 2016
| Lymphocytic colitis | |
|---|---|
| Diagnosis in short | |
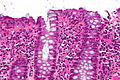
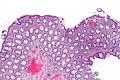
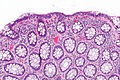
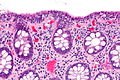
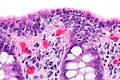
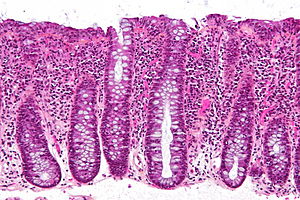 Lymphocytic colitis. HPS stain. | |
|
| |
| LM | intraepithelial lymphocytes (>20/100 enterocytes), none or rare PMNs, no architectural distortion, normal subepithelial collagen band (< 10 micrometres thick) |
| LM DDx | collagenous colitis, infectious colitis, Crohn's disease (rare) |
| Site | colon, rectum |
|
| |
| Associated Dx | autoimmune diseases (celiac disease, diabetes mellitus, thyroid disorders, arthritis) |
| Symptoms | diarrhea, non-bloody |
| Endoscopy | normal |
| Clin. DDx | irritable bowel syndrome |
| Lymphocytic colitis | |
|---|---|
| External resources | |
| EHVSC | 10184 |
Lymphocytic colitis, abbreviated LC, is a type of microscopic colitis. It has a characteristic clinical presentation and no apparent endoscopic changes.
Lymphocytic proctitis redirects here.
General
Presentation:
- Chronic diarrhea, non-bloody.[1]
- Lymphocytic colitis may be related to collagenous colitis.
- It is hypothesized that these conditions may be the same pathology at different time points.[1]
Notes:
- Clinical DDx includes irritable bowel syndrome - which has no or subtle histopathologic changes.
- This pathology also afflicits rectum; however, it is less commonly found there.
- The rectum is afflicted in approximately in 65% of cases.[2]
Epidemiology
- Age: a disease of adults - usually 50s.
- Sex:
- Drugs are associated with LC and CC.
- NSAIDs - posulated association/weak association,
- SSRIs (used primarily for depression) - moderate association, dependent on specific drug.
- Associated with autoimmune disorders - celiac disease, diabetes mellitus, thyroid disorders and arthritis.[3]
- No increased risk of colorectal carcinoma.[3]
Treatment
- Sometimes just follow-up.
- Steroids - budesonide -- short-term treatment.[3]
Gross
- Endoscopic examination is normal.
- This is why it is called a microscopic colitis.
Microscopic
Features:
- Lots of intraepithelial lymphocytes (>=20/100 lymphocytes/surface epithelial cells[3]) and
- Lymphocytes in the lamina propria.
Significant negatives:[4]
- No neutrophils.
- No crypt distortion.
DDx:
- Infectious colitis - neutrophils present... not lymphocytes.
- Collagenous colitis - has a band of collagen below the epithelium.
- Crohn's disease - uncommon, may be a perfect mimic.[5]
Images
www:
Sign out
ASCENDING COLON, BIOPSY: - LYMPHOCYTIC COLITIS.
RECTUM, BIOPSY: - LYMPHOCYTIC PROCTITIS. - NEGATIVE FOR ARCHITECTURAL DISTORTION AND NEGATIVE FOR CRYPTITIS. - NEGATIVE FOR DYSPLASIA.
Micro
The sections show colonic mucosa with abundant intraepithelial lymphocytes (>20 lymphocytes/100 surface epithelial cells). The glandular architecture is within normal limits. No thickened collagen band is apparent below the epithelium.
There are no granulomas. No neutrophilic cryptitis is apparent. The epithelium matures appropriately to the surface.
Alternate
The sections show rectal mucosa with increased intraepithelial lymphocytes (25-30/100 epithelial cells), apoptotic epithelial cells, abundant lamina propria plasma cells, rare lymphoid aggregates and a mild increase of eosinophils (25/1 HPF (0.24 mm*mm)). There is surface goblet cell depletion. The collagen table is not apparently thickened. There is no apparent cryptitis. The architecture is within normal limits.
See also
References
- ↑ 1.0 1.1 1.2 1.3 URL: http://emedicine.medscape.com/article/180664-overview. Accessed on: 31 May 2010.
- ↑ Agnarsdottir M, Gunnlaugsson O, Orvar KB, et al. (May 2002). "Collagenous and lymphocytic colitis in Iceland". Dig. Dis. Sci. 47 (5): 1122–8. PMID 12018911.
- ↑ 3.0 3.1 3.2 3.3 3.4 Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S (December 2008). "Diagnosis and management of microscopic colitis". World J. Gastroenterol. 14 (48): 7280-8. PMC 2778111. PMID 19109861. http://www.wjgnet.com/1007-9327/14/7280.asp.
- ↑ http://hopkins-gi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&disease=29&organ=6&lang_id=1
- ↑ Goldstein, NS.; Gyorfi, T. (Sep 1999). "Focal lymphocytic colitis and collagenous colitis: patterns of Crohn's colitis?". Am J Surg Pathol 23 (9): 1075-81. PMID 10478667.