Difference between revisions of "Lymph node pathology"
| Line 283: | Line 283: | ||
==Sinus histiocytosis== | ==Sinus histiocytosis== | ||
{{Main|Sinus histiocytosis}} | {{Main|Sinus histiocytosis}} | ||
Should '''not''' be confused with ''[[sinus histiocytosis with massive lymphadenopathy]]'', also known as Rosai-Dorfman disease. | |||
==Kikuchi disease== | ==Kikuchi disease== | ||
Revision as of 00:46, 1 December 2013
This article deals with non-haematologic malignant, i.e. metastases, and non-malignant lymph node pathology. An introduction to the lymph node is in the lymph nodes article.
Haematologic malignancies (in lymph nodes) are dealt with in other articles - see haematopathology and lymphoma.
Overview
Clinical:
- Lymphadenopathy.
Differential diagnosis:[1]
- Infectious - fungal, mycobacterial, viral, protozoal (Toxoplasma), bacterial (Chlamydia, Rickettsia, Bartonella)).
- Neoplastic - lymphoma, carcinoma.
- Endocrine - hyperthyroidism.
- Trauma.
- Autoimmune - SLE, RA, dermatomyositis.
- Inflammatory - drugs (phenytoin).
- Idiopathic - sarcoidosis.
Overview in a table
| Entity | Key feature | Other findings | IHC | DDx | Image |
|---|---|---|---|---|---|
| Non-specific reactive follicular hyperplasia (NSRFH) | large spaced cortical follicles | tingible body macrophages, normal dark/light GC pattern | BCL2 -ve | infection (Toxoplasmosis, HIV/AIDS), Hodgkin's lymphoma | image ? |
| Lymph node metastasis | foreign cell population, usu. in subcapsular sinuses | +/-nuclear atypia, +/-malignant architecture | dependent on tumour type (see IHC) | dependent on morphology, endometriosis (mimics adenocarcinoma), ectopic decidua (mimics SCC) | |
| Progressive transformation of germinal centers | large (atypical) germinal centers | poorly demarcated germinal center (GC)/mantle zone interfaces, expanded mantle zone | IHC to r/o nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) | NLPHL, follicular hyperplasia | |
| Toxoplasmosis | large follicles; epithelioid cells perifollicular & intrafollicular | reactive GCs, monocytoid cell clusters, epithelioid cells | IHC for toxoplasma | NSRFH, HIV/AIDS, Hodgkin's lymphoma | |
| Kikuchi disease (histiocystic necrotizing lymphadenitis) | No PMNs | histiocytes, necrosis | IHC for large cell lymphoma (CD30 + others) | SLE (has (blue) hematoxylin bodies in necrotic areas), large cell lymphomas | |
| Cat-scratch disease | PMNs in necrotic area | "stellate" (or serpentine) shaped microabscesses, granulomas | B. henselae, Dieterle stain | HIV/AIDS, NSRFH | |
| Dermatopathic lymphadenopathy | melanin-laden histiocytes | histiocytosis | S100+ve (interdigitating dendritic cells), CD1a+ve (Langerhans cells) | cutaneous T-cell lymphoma | |
| Kimura disease | eosinophils | angiolymphoid proliferation (thick-walled blood vessels with hobnail endothelial cells) | IHC ? | Langerhans cell histiocytosis, drug reaction, angiolymphoid hyperplasia with eosinophilia | |
| Langerhans cell histiocytosis | abundant histiocytes with reniform nuclei | often prominent eosinophilia | S100+, CD1a+ | Kimura disease (eosinophilia), Rosai-Dorfman disease | |
| Rosai-Dorfman disease | sinus histiocytosis | emperipolesis (intact cell within a macrophage) | S100+, CD1a- | Langerhans cell histiocytosis | |
| Systemic lupus erythematosus lymphadenopathy | (blue) hematoxylin bodies | necrosis, no PMNs | IHC for large cell lymphoma (CD30 + others) | Kikuchi disease, large cell lymphomas | |
| Castleman disease, hyaline vascular variant | thick mantle cell layer with laminar appearance ("onion skin" layering) | hyaline (pink crap), lollipops (large vessels into GC), no mitoses in GC | IHC - to r/o mantle cell lymphoma | mantle cell lymphoma, HIV/AIDS | |
| Castleman disease, plasma cell variant | thick mantle cell layer | sinus perserved, interfollicular plasma cells, mitoses in GC | HHV-8 | HIV/AIDS | image ? |
| Intranodal palisaded myofibroblastoma | spindle cells with nuclear palisading | RBC extravasation, fibrillary bodies with a central vessel "amianthoid fibers" | SMA+, cyclin D1+ | schwannoma |
Follicular lymphoma vs. reactive follicular hyperplasia
Factors to consider:[2]
| Reactive follicular hyperplasia |
Follicular lymphoma | |
|---|---|---|
| Follicle location | cortex | cortex and medulla |
| Germinal center edge | sharp/well-demarcated | poorly demarcated |
| Germinal center density | well spaced, sinuses open | crowded, sinuses effaced/ compressed to nothingness |
| Tingible body macrophages |
common | uncommon |
| Germinal center light/dark pattern |
normal | abnormal |
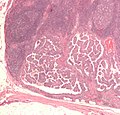
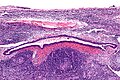
Lymph node metastasis
General
- Determination of lymph node status is one of the most common indications for the examination of lymph nodes.
- It is a good idea to look at the tumour (if available) ...before looking at the LNs for mets.
- Lymph node metastasis, in the absence of other metastases, often up-stage a cancer from stage II to stage III.
Gross
- Outside:
- "Large" - size varies by site.
- Neck >10 mm.[3]
- Shape - round more suspicious than oval.
- "Large" - size varies by site.
- Sectioned:
- White firm lesion with irregular border - classic appearance.
- Non-fatty hilum.[3]
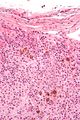
Microscopic
Features:
- Foreign cell population - key feature.
- Classic location: subcapsular sinuses.
- +/-Cells with cytologic features of malignancy.
- Nuclear pleomorphism (variation in size, shape and staining).
- Nuclear atypia:
- Nuclear enlargement.
- Irregular nuclear membrane.
- Irregular chromatin pattern, esp. asymmetry.
- Large or irregular nucleolus.
- Abundant mitotic figures.
- +/-Cells in architectural arrangements seen in malignancy; highly variable - dependent on tumour type and differentiation.
- +/-Gland formation.
- +/-Single cells.
- +/-Small clusters of cells.
Notes:
- Cytologic features of malignancy may not be present; some tumours, e.g. gallbladder carcinoma, do not always have overt cytologic features of malignancy.
- The diagnosis is based on the fact that they are foreign to the lymph node and architecturally consistent with a well-differentiated malignancy.
- Lymph node metastases in sarcomas are uncommon; they are seen in <3% of cases.[4]
- Fatty lymph nodes (esp. fatty hilus[3]) are less likely to harbor metastases.[5]
DDx - mimics of metastatic disease:
- Endometriosis.
- Ectopic decidua.[6]
- Endosalpingiosis.[7]
- Melanocytic nevus - intracapsular or within the trabeculae.[8]
- Dermatopathic lymphadenopathy.[citation needed]
- Sinus histiocytosis - especially for the junior resident.
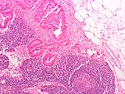
Images
Mimics
Kaposi sarcoma
- One of the few non-lymphoid primary lymph node tumours.[9]
Melanocytic nevi
- Benign melanocytic nevi can be found in lymph nodes.[9]
Progressive transformation of germinal centers
- Abbreviated as PTGC.
Reactive follicular hyperplasia
General
- Many causes - including: bacteria, viruses, chemicals, drugs, allergens.
- In only approximately 10% can definitive cause be identified.[10]
Microscopic
Features:[11]
- Enlarged follicles, follicle size variation - key feature with:
- Large germinal centers (pale on H&E).
- Mitoses common.
- Variable lymphocyte morphology.
- Tingible-body macrophage (large, pale cells with junk in the cytoplasm).
- Germinal centers (GCs) have a crisp/sharp edge.
- Normal dark/light variation of GCs; superficial aspect light, deeper aspect darker.
- Rim of small (inactive) lymphocytes.
- Large germinal centers (pale on H&E).
DDx:
- Hodgkin lymphoma - with rare Reed-Sternberg cells.
- Non-Hodgkin lymphoma.
- T-cell/histiocyte-rich large B cell lymphoma.
Image: Normal lymph node (umdnj.edu).
IHC
Screening panel:
- CD3.
- CD5.
- CD10.
- CD20.
- CD30.
- CD15.
Others:
- BCL2 -ve.
Diffuse paracortical hyperplasia
General
- Benign.
Microscopic
Features:[11]
- Interfollicular areas enlarged - key feature.
- T cell population increased.
- Plasma cells.
- Macrophages.
- Large Reed-Sternberg-like cells.
Sinus histiocytosis
Should not be confused with sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease.
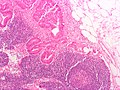
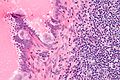
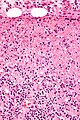
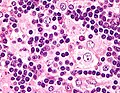
Kikuchi disease
General
Epidemiology:[13]
- Usually <40 years old.
- Asian.
- Female:Male = 3:1.[14]
Treatment:
- Usually self-limited.[13]
- Oral corticosteroids.
DDx:
- Non-Hodgkin lymphoma.
- Systemic lupus erythematosus.
- Have hematoxyphil bodies in necrotic foci.
- Dark blue irregular bodies on H&E.
- Have hematoxyphil bodies in necrotic foci.
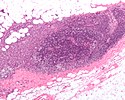
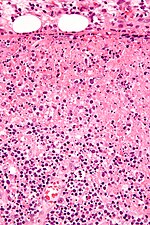
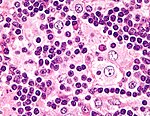
Micrograph
Features (the three main features - just as the name suggests):[15]
- Histiocytes.
- May be crescentic.
- Necrosis (due to apoptosis) - paracortical areas.[13]
- Necrosis without neutrophils - key feature.
- Lymphocytes (CD8 +ve).
- Plasmacytoid dendritic cells.
Notes:
- Dendritic cell - vaguely resembles a macrophage:[16]
- Long membrane projections - key feature.
- Abundant blue-grey cytoplasm, +/- ground-glass appearance.
- Nucleus: small, ovoid, usu. single nucleolus.
Images
www:
IHC
- CD68 +ve.
- CD8 +ve - usu. predominant.
- CD4, CD20, CD3, and CD30 - mixed.
- Done to excluded lymphoma; esp. large cell lymphomas;[17] should show a mixed population of lymphocytes.
- Others:
- CD56 -ve.
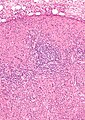
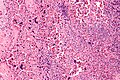
Systemic lupus erythematosus lymphadenopathy
General
- Lymphadenopathy associated with systemic lupus erythematosus (SLE).
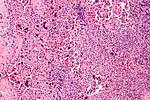
Microscopic
Features:[18]
- Necrosis.
- Hematoxylin bodies (in necrotic foci).
- Dark blue irregular bodies on H&E.
DDx:
Images
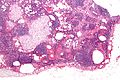
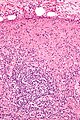
Castleman disease
General
- Benign.
- Hyaline vascular variant - a pathology of the follicular dendritic cells.[20]
Classification
CD is grouped by histologic appearance:[21]
- Hyaline vascular (HV) variant (described by Castleman).
- Usually unicentric.
- Typically mediastinal or axial.
- More common than plasma cell variant; represents 80-90% of CD cases.
- May be associated with follicular dendritic cell neoplasia.[22]
- Plasma cell (PC) variant.
- Usually multicentric, may be unicentric.
- Abundant plasma cells.
- Associated with HHV-8 infection (the same virus implicated in Kaposi's sarcoma).
Notes:
- The subclassification of CD is in some flux. Some authors advocate splitting-out HHV-8 and multicentric as separate subtypes.[23]
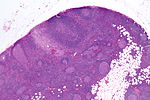
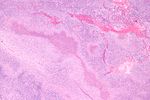
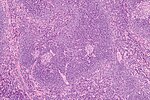
Microscopic
Hyaline-vascular variant
- Pale concentric (expanded) mantle zone lymphocytes - key feature.
- "Regressed follicles" - germinal center (pale area) is small.
- "Lollipops":
- Germinal centers fed by prominent (radially penetrating sclerotic) vessels; lollipop-like appearance.
- Two germinal centers in one follicle.
- Hyaline material (pink acellular stuff on H&E) in germinal center.
- Sinuses effaced (lost).
- Mitoses absent.
Images
www:
Plasma cell variant
Features:[25]
- Interfollicular sheets of plasma cells - key feature.
- Active germinal centers - mitoses present.
- Sinus perserved.
IHC
Hyaline-vascular variant:
- Stains to exclude mantle cell lymphoma:
- Cyclin D1.
Plasma cell variant:
- HHV-8 +ve.
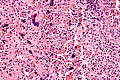
Cat-scratch disease
- AKA Cat-scratch fever.
General
- Infection caused Bartonella henselae,[26] a gram-negative bacilla (0.3-1.0 x 0.6-3.0 micrometers) in chains, clumps, or singular.[27]
- Treatment: antibiotics.
Clinical
Features:[28]
- Usually unilateral.
- May be disseminated in individuals with immune dysfunction.
- Contact with cats.
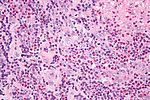
Micrograph
Features:[28]
- Necrotizing granulomas with:
- Neutrophils present in microabscess (necrotic debris) - key feature.
- Microabscesses often described as "stellate" (star-shaped).
- Neutrophils present in microabscess (necrotic debris) - key feature.
- +/-Multinucleated giant cells.
Notes:
- May involve capsule or perinodal tissue.
DDx of stellate abscess in lymph nodes - cat split:[29]
- Cat-scratch disease.
- Sporotrichosis.
- Lymphogranuloma venereum.
- Tularemia.
Images
www:
Stains
- Warthin-Starry stain +ve.
IHC
- B. henselae IHC stain +ve - diagnostic.
Toxoplasma lymphadenitis
General
- Caused by protozoan Toxoplasma gondii.
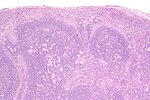
Microscopic
Features:[28]
- Reactive germinal centers (pale areas - larger than usual).
- Often poorly demarcated - due to loose epithelioid cell clusters at germinal center edge - key feature.
- Epithelioid cells - perifollicular & intrafollicular.
- Loose aggregates of histiocytes (do not form round granulomas):
- Abundant pale cytoplasm.
- Nucleoli.
- Loose aggregates of histiocytes (do not form round granulomas):
- Monocytoid cells (monocyte-like cells) - in cortex & paracortex.
- Large cells in islands/sheets key feature with:
- Abundant pale cytoplasm - important.
- Well-defined cell border - important.
- Singular nucleus.
- Cell clusters usually have interspersed neutrophils.
- Large cells in islands/sheets key feature with:
Images:
Notes:
- Monocytoid cells CD68 -ve.
IHC
- IHC for toxoplasmosis.
Dermatopathic lymphadenopathy
General
- Lymphadenopathy associated with a skin lesion - key feature.
- May be benign or malignant (e.g. T-cell lymphoma).
Microscopic
Features:[30]
- Abundant histiocytes & special histiocytes - in loose irregular clusters - located in the sinuses, i.e. sinus histiocytosis - key feature:
- Do not form granuloma; may be similar to toxoplasma.
- Plasma cells (medulla).
- Eosinophils.
Histiocytes & special histiocytes:
- Histiocytes:
- +/-Melanin pigment key feature (if present).
- Lipid-laden macrophages.
- Interdigitating dendritic cells:
- Need IHC to identify definitively.
- Langerhans cells:
- Classically have a kidney bean nuclei.
- Need IHC to identify definitively.
DDx:
- Metastatic malignant melanoma - (melanin) pigmented cells have nuclear atypia, not histiocytes.
- Sinus histiocytosis - no cells with melanin.
Images
IHC
- Interdigitating dendritic cells: S100 +ve, CD1a -ve.
- Langerhans cells: S100 +ve, CD1a +ve.
Kimura lymphadenopathy
Microscopic
Features:
- Abundant eosinophils.
- Thick-wall blood vessels.
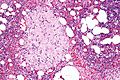
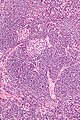
Rosai-Dorfman disease
- Abbreviated RDD.
General
- AKA sinus histiocytosis with massive lymphadenopathy, abbreviated SHML.[31]
- Super rare.
- Prognosis - good.
Clinical findings:[32]
- Fever.
- Leukocytosis with neutrophilia.
- Polyclonal gamaglobulinemia.
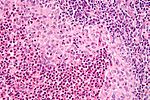
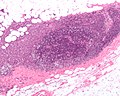
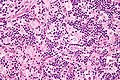
Microscopic
Features:
- Sinus histiocytosis:
- Histiocytes - abundant.
- Singular large round nuclei[33] ~2x the size of resting lymphocyte.
- Prominent nucleolus - visible with 10x objective.
- Abundant cytoplasm.
- Singular large round nuclei[33] ~2x the size of resting lymphocyte.
- Histiocytes - abundant.
- Emperipolesis (from Greek: em = inside, peri = around, polemai = wander about[34]):
DDx:
- Other histiocytosis:
- Infection, e.g. rhinoscleroma (nasopharynx), xanthogranulomatous pyelonephritis.
- Xanthomatous change.
Images
www:
- RDD - case 1 - several images (upmc.edu).
- RDD - case 2 - several images of breast (upmc.edu).
- RDD - case 3 - several images (upmc.edu).
- RDD - case 4 - several images (upmc.edu).
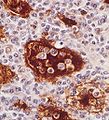
IHC
- CD68 +ve.
- S100 +ve.
- Useful for seeing emperipolesis.
- CD1a -ve.
- CD1a positive in Langerhans cell histiocytosis.
Langerhans cell histiocytosis
Microscopic
Features:
- Langerhans cells histiocytes - key feature.
- Clusters of cells (histiocytes) with a reniform (kidney-shaped) nucleus and abundant foamy cytoplasm.
- +/-Eosinophils - often prominent.
See Langerhans cell histiocytosis for details.
Lymph node hyalinization
- AKA hyalinized lymph node.
General
- Benign.
- Associated with aging.[37]
Microscopic
Features:
- Hyaline material (acellular pink stuff on H&E) within a lymph node.
Subdivided into:[37]
- Mediastinal-type.
- Usually in medullary sinus.
- Onion peel-like appearance.
- Pelvic-type hyalinization.
- Discrete round, eosinophilic, glassy appearance at low power, whirled/fibrous at high power.
- +/-Calcification.
DDx:
- Amyloidosis - cotton candy-like appearance, usu. no calcifications.
Images:
See also
References
- ↑ URL: http://path.upmc.edu/cases/case289.html. Accessed on: 14 January 2012.
- ↑ DB. 4 August 2010.
- ↑ 3.0 3.1 3.2 Mack, MG.; Rieger, J.; Baghi, M.; Bisdas, S.; Vogl, TJ. (Jun 2008). "Cervical lymph nodes.". Eur J Radiol 66 (3): 493-500. doi:10.1016/j.ejrad.2008.01.019. PMID 18337039.
- ↑ Fong, Y.; Coit, DG.; Woodruff, JM.; Brennan, MF. (Jan 1993). "Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients.". Ann Surg 217 (1): 72-7. PMC 1242736. PMID 8424704. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242736/.
- ↑ Korteweg, MA.; Veldhuis, WB.; Mali, WP.; Diepstraten, SC.; Luijten, PR.; van den Bosch, MA.; Eijkemans, RM.; van Diest, PJ. et al. (Feb 2012). "Investigation of lipid composition of dissected sentinel lymph nodes of breast cancer patients by 7T proton MR spectroscopy.". J Magn Reson Imaging 35 (2): 387-92. doi:10.1002/jmri.22820. PMID 21972135.
- ↑ Wu, DC.; Hirschowitz, S.; Natarajan, S. (May 2005). "Ectopic decidua of pelvic lymph nodes: a potential diagnostic pitfall.". Arch Pathol Lab Med 129 (5): e117-20. doi:10.1043/1543-2165(2005)129e117:EDOPLN2.0.CO;2. PMID 15859655.
- ↑ Corben, AD.; Nehhozina, T.; Garg, K.; Vallejo, CE.; Brogi, E. (Aug 2010). "Endosalpingiosis in axillary lymph nodes: a possible pitfall in the staging of patients with breast carcinoma.". Am J Surg Pathol 34 (8): 1211-6. doi:10.1097/PAS.0b013e3181e5e03e. PMID 20631604.
- ↑ Biddle, DA.; Evans, HL.; Kemp, BL.; El-Naggar, AK.; Harvell, JD.; White, WL.; Iskandar, SS.; Prieto, VG. (May 2003). "Intraparenchymal nevus cell aggregates in lymph nodes: a possible diagnostic pitfall with malignant melanoma and carcinoma.". Am J Surg Pathol 27 (5): 673-81. PMID 12717252.
- ↑ 9.0 9.1 Bigotti, G.; Coli, A.; Mottolese, M.; Di Filippo, F. (Sep 1991). "Selective location of palisaded myofibroblastoma with amianthoid fibres.". J Clin Pathol 44 (9): 761-4. PMC 496726. PMID 1918406. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC496726/.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 174. ISBN 978-0781775960.
- ↑ 11.0 11.1 Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 179. ISBN 978-0781775960.
- ↑ Kaushik V, Malik TH, Bishop PW, Jones PH (June 2004). "Histiocytic necrotising lymphadenitis (Kikuchi's disease): a rare cause of cervical lymphadenopathy". Surgeon 2 (3): 179–82. PMID 15570824.
- ↑ 13.0 13.1 13.2 13.3 Hutchinson CB, Wang E (February 2010). "Kikuchi-Fujimoto disease". Arch. Pathol. Lab. Med. 134 (2): 289–93. PMID 20121621.
- ↑ URL: http://emedicine.medscape.com/article/210752-overview. Accessed on: 3 June 2010.
- ↑ URL: http://www.ispub.com/journal/the_internet_journal_of_head_and_neck_surgery/volume_1_number_1_30/article_printable/kikuchi_s_lymphadenitis_in_a_young_male.html. Accessed on: 1 June 2010.
- ↑ URL: http://www.healthsystem.virginia.edu/internet/hematology/hessedd/benignhematologicdisorders/normal-hematopoietic-cells/dendritic-cell.cfm?drid=214. Accessed on: 3 June 2010.
- ↑ Good DJ, Gascoyne RD (August 2009). "Atypical lymphoid hyperplasia mimicking lymphoma". Hematol. Oncol. Clin. North Am. 23 (4): 729–45. doi:10.1016/j.hoc.2009.04.005. PMID 19577167.
- ↑ Kojima, M.; Nakamura, S.; Itoh, H.; Yoshida, K.; Asano, S.; Yamane, N.; Komatsumoto, S.; Ban, S. et al. (1997). "Systemic lupus erythematosus (SLE) lymphadenopathy presenting with histopathologic features of Castleman' disease: a clinicopathologic study of five cases.". Pathol Res Pract 193 (8): 565-71. PMID 9406250.
- ↑ URL: http://www.mayoclinic.com/health/castleman-disease/DS01000. Accessed on: 17 June 2010.
- ↑ Cokelaere, K.; Debiec-Rychter, M.; De Wolf-Peeters, C.; Hagemeijer, A.; Sciot, R. (May 2002). "Hyaline vascular Castleman's disease with HMGIC rearrangement in follicular dendritic cells: molecular evidence of mesenchymal tumorigenesis.". Am J Surg Pathol 26 (5): 662-9. PMID 11979097.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 228. ISBN 978-0781775960.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 596. ISBN 978-0781765275.
- ↑ Cronin, DM.; Warnke, RA. (Jul 2009). "Castleman disease: an update on classification and the spectrum of associated lesions.". Adv Anat Pathol 16 (4): 236-46. doi:10.1097/PAP.0b013e3181a9d4d3. PMID 19546611.
- ↑ URL: http://www.ispub.com/journal/the_internet_journal_of_otorhinolaryngology/volume_9_number_2_11/article/a_rare_case_of_castleman_s_disease_presenting_as_cervical_neck_mass.html. Accessed on: 15 June 2010.
- ↑ 25.0 25.1 Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 236. ISBN 978-0781775960.
- ↑ Jerris, RC.; Regnery, RL. (1996). "Will the real agent of cat-scratch disease please stand up?". Annu Rev Microbiol 50: 707-25. doi:10.1146/annurev.micro.50.1.707. PMID 8905096.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 110. ISBN 978-0781775960.
- ↑ 28.0 28.1 28.2 Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 113. ISBN 978-0781775960.
- ↑ URL: http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm. Accessed on: 23 September 2011.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 226. ISBN 978-0781775960.
- ↑ Agarwal A, Pathak S, Gujral S (October 2006). "Sinus histiocytosis with massive lymphadenopathy--a review of seven cases". Indian J Pathol Microbiol 49 (4): 509–15. PMID 17183839.
- ↑ Landim, FM.; Rios, Hde O.; Costa, CO.; Feitosa, RG.; Rocha Filho, FD.; Costa, AA. (Jul 2009). "Cutaneous Rosai-Dorfman disease.". An Bras Dermatol 84 (3): 275-8. PMID 19668942.
- ↑ Bailey, D. 24 August 2010.
- ↑ Stedman's Medical Dictionary. 27th Ed.
- ↑ Viswanathan P, Raghunathan K, Majhi U, Pandit RV, Shanthi R, Rajkumar T (1997). Emperipolesis : an electron microscopic characteristic in RDD (Rosai-Dorfaman disease) : a case report. pp. 14-6. http://www.ijmpo.org/article.asp?issn=0971-5851;year=1997;volume=18;issue=1;spage=14;epage=16;aulast=Viswanathan;type=0.
- ↑ Lyons DJ, Gautam A, Clark J, et al. (January 1992). "Lymphocyte macrophage interactions: peripolesis of human alveolar macrophages". Eur. Respir. J. 5 (1): 59–66. PMID 1577151.
- ↑ 37.0 37.1 Taniguchi, I.; Murakami, G.; Sato, A.; Fujiwara, D.; Ichikawa, H.; Yajima, T.; Kohama, G. (Oct 2003). "Lymph node hyalinization in elderly Japanese.". Histol Histopathol 18 (4): 1169-80. PMID 12973685.