Difference between revisions of "Hodgkin lymphoma"
m (fill in BCL6 and MUM1 in comparison table) |
|||
| Line 132: | Line 132: | ||
|CD20 || +ve || -ve | |CD20 || +ve || -ve | ||
|- | |- | ||
|BCL6 || || | |BCL6 || +ve || -ve | ||
|- | |- | ||
|MUM1<ref>URL: [http://www.ncbi.nlm.nih.gov/omim/601900 http://www.ncbi.nlm.nih.gov/omim/601900]. Accessed on: 10 August 2010.</ref> || -ve || | |MUM1<ref>URL: [http://www.ncbi.nlm.nih.gov/omim/601900 http://www.ncbi.nlm.nih.gov/omim/601900]. Accessed on: 10 August 2010.</ref> || -ve || +ve | ||
|- | |- | ||
|CD30 || -ve || +ve (most sensitive). | |CD30 || -ve || +ve (most sensitive). | ||
Latest revision as of 22:01, 4 December 2018
| Classical Hodgkin lymphoma | |
|---|---|
| Diagnosis in short | |
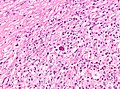
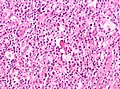
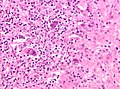
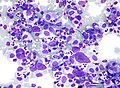
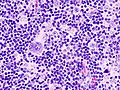
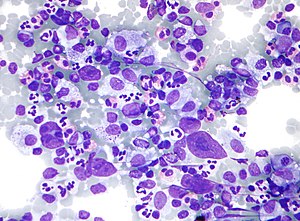 HL mixed cellularity - cytology. | |
|
| |
| LM | Reed-Sternberg cell (large binucleated cell (>= 45 micrometres), +/-multinucleated, +/-horseshoe-like shape, macronucleolus - approximately the size of a RBC (~8 micrometers)), well-defined cell border, abundant cytoplasm. |
| Subtypes | nodular sclerosis CHL, mixed cellularity CHL, lymphocyte-rich CHL, lymphocyte-depleted CHL |
| LM DDx |
diffuse large B cell lymphoma (esp. T-cell/histiocytic-rich LBCL), anaplastic large cell lymphoma, B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma, nodular lymphocyte-predominant Hodgkin lymphoma |
| IHC | CD30 Reed-Sternberg cells (RSCs) +ve ~98%, CD15 Reed-Sternberg cells +ve ~80% (also stains neutrophils), CD45 often negative in RSCs, CD20 -ve/+ve, PAX5 +ve |
| Site | usu. lymph node - classically in the neck |
|
| |
| Clinical history | young adults, older adults (bimodal distribution) |
| Signs | lymphadenopathy - usu. neck, +/-B symptoms (fever, night sweats, weight loss) |
| Prevalence | common |
| Prognosis | usu. good, dependent on stage |
Hodgkin lymphoma, abbreviated HL, is a haematological malignancy. If not otherwise specified, Hodgkin lymphoma generally refers to classical Hodgkin lymphoma (CHL) rather than nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL). The latter accounts for only about 5% of the loose label of Hodgkin lymphoma[1] and shows a sufficiently different biology and immunophenotype that is essentially a different disease (see main article on NLPHL). The common feature is large atypical cells: Hodgkin/Reed-Sternberg cells in the case of classical Hodgkin lymphoma and "popcorn"/lymphohistiocytic/L&H cells in NLPHL. However, at least in typical cases, there are morphological and immunophenotypic differences.
Classical Hodgkin lymphoma has a bi-modal distribution, afflicting young adults and with a further peak in incidence in middle-age. Fortunately, it usually has a good prognosis.
Pathologists say "... it is both the easiest and hardest diagnosis to make." The reason for this is: the diagnosis depends on finding Reed-Sternberg cells (or Popcorn cells); if they are obvious the diagnosis is easy... if you can't find 'em and an alternative diagnosis is not apparent -- you wonder whether you're missing them.
General
Clinical
Symptoms:[1]
- "B symptoms" - all required:[2] weight loss, night sweats and fever.
- Infections due to immune dysfunction.
Diagnosis:
- HL cannot be diagnosed with standard flow cytometry (FC) - but has been diagnosed with specialized FC.[3]
Prognosis:
- Usually good.
- Unlike non-Hodgkin lymphomas, it spreads in a predictable pattern; thus, staging plays an important role in determining the therapy.[4]
- Clinically classified into early favourable, early unfavourable and late/advanced disease.
Classic HL sub-types
Subtypes of classic HL
There are four CHL subtypes:[1]
- Nodular sclerosis CHL - ~70% of CHL.
- Mixed cellular background - T cell, plasma cells, eosinophils, neutrophils and histiocytes.
- Nodular sclerosing fibrosis - thick strands fibrosis.
- Mixed cellularity CHL - ~20-25% of CHL.
- Lymphocyte-rich CHL - rare.
- T lymphocytes only (no mix of cells).
- Lymphocyte-depleted CHL - rare.
- May be associated with HIV infection.[5]
Memory device:
- The subtypes prevalence is in reverse alphabetical order.
Gross
Location:
- Almost always arises from a lymph node - classically in the neck, but may be in the axilla and mediastinum
- Spleen may be involved
- Bone marrow involvement is unusual (~5% of cases, higher in HIV-associated cases), so bone marrow assessment is usually not performed
- Extranodal Hodgkin lymphoma is (case report) rare.[6]
Microscopic
Defined by Reed-Sternberg cells (RSCs). Morphologically similar mononuclear cells are known as Hodgkin cells. RSCs are:
- Large binucleated cell (>= 45 micrometres).[7]
- May be multinucleated.
- May have a horseshoe-like shape.
- Macronucleolus - approximately the size of a RBC (~8 micrometers).
- Well-defined cell border.
- Abundant cytoplasm.
RSC may show peri-cellular clearing, making the cells appear within a space. These are called lacunar cells (as they are in a "lake"). Apoptotic RSC may show pyknotic nuclei and scant eosinophilic cytoplasm and are sometimes known as "mummified" cells.
Images (classic HL)
DDx both CHL & NLPHL
- CHL/NLPHL.
- Diffuse large B cell lymphoma (DLBCL), esp. T-cell/histiocytic-rich LBCL.
- Anaplastic large cell lymphoma (ALCL).
- B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma.[8] (typically in cases of numerous large atypical cells where the morphology and immunophenotype do not neatly fit into either DLBCL or CHL).
IHC
Abbreviated panel:[9]
- CD30 Reed-Sternberg cells (RSCs) +ve ~98% (beware of mis-interpreting CD30+ activated lymphoid cells)
- CD15 Reed-Sternberg cells +ve ~80%, stains neutrophils.
- Both CD30 and CD15 are classically positive in a membranous and Golgi pattern
- MUM1 +ve
- CD45 often negative in RSCs.
- CD20 may stain RSCs (usually negative, but can be weak).
- PAX5 +ve, though said to be weaker than background normal B-cells[10]
Additional - for completeness:
- CD3 (T lymphocytes) - negative in RSCs
- OCT2/BOB1 negative (co-transcription factors for immunoglobulin production, one or the other is usually negative)
- 40% are EBV positive.
NLPHL IHC differs from the classical HL:[10]
- LCA +ve.
- CD20 +ve.
- CD10 +ve.
- Bcl-6 +ve.
- EMA +ve (40-50%)
- CD30 -ve
- CD15 -ve.
A panel
| Antibody | NLPHL | CHL |
| CD45 | +ve | -ve |
| CD20 | +ve | -ve |
| BCL6 | +ve | -ve |
| MUM1[11] | -ve | +ve |
| CD30 | -ve | +ve (most sensitive). |
| CD15 | -ve | +ve |
| CD21 | networks present | no networks |
| CD23 | networks present | no networks |
| OCT-2 | +ve | -ve |
| PAX5 | +ve | +ve (proves B cell linage) |
| CD3 | usu. < benign B cell | usu. > benign B cell component |
| CD57 | rosettes around malign. cells | - |
| EBER | -ve | +ve/-ve |
| EMA | +ve/-ve | -ve |
| 4 unstained |
Sign out
Suggestive FNA
Lymph Node, Right Neck, FNA: - Large binucleated and multinucleated cells with macronucleoli in a background of abundant lymphocytes, histiocytes, rare eosinophils. Comment: A cell block is not available for further work-up. The findings raise the possibility of Hodgkin's lymphoma. A further biopsy is required for the diagnosis.
See also
References
- ↑ 1.0 1.1 1.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 567. ISBN 978-0781765275.
- ↑ URL: http://lymphoma.about.com/od/symptoms/f/bsymptoms.htm. Accessed on: 11 August 2010.
- ↑ Fromm JR, Thomas A, Wood BL (March 2009). "Flow cytometry can diagnose classical hodgkin lymphoma in lymph nodes with high sensitivity and specificity". Am. J. Clin. Pathol. 131 (3): 322–32. doi:10.1309/AJCPW3UN9DYLDSPB. PMID 19228638.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 315. ISBN 978-1416054542.
- ↑ 5.0 5.1 Sissolak G, Sissolak D, Jacobs P (April 2010). "Human immunodeficiency and Hodgkin lymphoma". Transfus. Apher. Sci. 42 (2): 131–9. doi:10.1016/j.transci.2010.01.008. PMID 20138008.
- ↑ Vadmal, MS.; LaValle, GP.; DeYoung, BR.; Frankel, WL.; Marsh, WL. (Dec 2000). "Primary localized extranodal hodgkin disease of the transverse colon.". Arch Pathol Lab Med 124 (12): 1824-7. doi:10.1043/0003-9985(2000)1241824:PLEHDO2.0.CO;2. PMID 11100066.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 329. ISBN 978-1416054542.
- ↑ Gualco, G.; Natkunam, Y.; Bacchi, CE. (Jan 2012). "The spectrum of B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma: a description of 10 cases.". Mod Pathol. doi:10.1038/modpathol.2011.200. PMID 22222636.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 568. ISBN 978-0781765275.
- ↑ 10.0 10.1 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 683. ISBN 978-1416025887.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/601900. Accessed on: 10 August 2010.