Difference between revisions of "Heart valves"
m (→Sign out) |
(→Rheumatic heart disease: split out) |
||
| (39 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
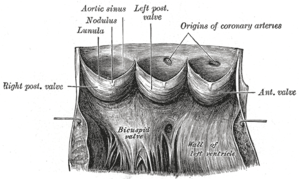
[[Image:Gray497.png|thumb|right|Aortic valve - drawing. (WC/Gray's Anatomy)]] | |||
'''[[Heart]] valves''' are the domain of the cardiac surgeon and their bread & butter. | '''[[Heart]] valves''' are the domain of the cardiac surgeon and their bread & butter. | ||
| Line 53: | Line 54: | ||
*Posterior (non-coronary cusp). | *Posterior (non-coronary cusp). | ||
Note: | |||
*The [[cut-up]] is described in ''[[grossing aortic valves]]''. | |||
===Microscopic=== | ===Microscopic=== | ||
Three layers (from proximal (ventricular side) to distal (valsalva side)):<ref name=Ref_PBoD558>{{Ref PBoD|558}}</ref> | Three layers (from proximal (ventricular side) to distal (valsalva side)):<ref name=Ref_PBoD558>{{Ref PBoD|558}}</ref> | ||
| Line 64: | Line 67: | ||
Notes: | Notes: | ||
*The loading of the ventricular aspect is tensile and the valsalva side compressive. Thus, it makes sense that the tissue on the ventricular aspect is good in tensile loading and the tissue on the valsalva side good in compression. The elastic tissue can be thought of as [http://en.wikipedia.org/wiki/Rebar rebar]... the collagen as concrete. | *The loading of the ventricular aspect is tensile and the valsalva side compressive. Thus, it makes sense that the tissue on the ventricular aspect is good in tensile loading and the tissue on the valsalva side good in compression. The elastic tissue can be thought of as [http://en.wikipedia.org/wiki/Rebar rebar]... the collagen as concrete. | ||
Image: | |||
*[http://www.e-heart.org/Photos/01_Cardiac_Structure_Photos/%C2%A9Mitral%20Valve%20Normal%20Chordae%20Tendinea%20640%20x%20419.jpg Normal mitral valve (e-heart.org)].<ref>URL: [http://www.e-heart.org/pages/01_cardiac_structure/01_Cardiac_Structure_MV_003.htm http://www.e-heart.org/pages/01_cardiac_structure/01_Cardiac_Structure_MV_003.htm]. Accessed on: 20 December 2012.</ref> | |||
==Mitral valve== | ==Mitral valve== | ||
| Line 71: | Line 77: | ||
**No fusion. | **No fusion. | ||
Note: | |||
*The [[cut-up]] is described in ''[[grossing mitral valves]]''. | |||
===Microscopic=== | ===Microscopic=== | ||
Similar to the aortic valve - layers: | Similar to the aortic valve - layers: | ||
#Atrialis. | #Atrialis.<ref name=pmid6821906 >{{Cite journal | last1 = Chesler | first1 = E. | last2 = King | first2 = RA. | last3 = Edwards | first3 = JE. | title = The myxomatous mitral valve and sudden death. | journal = Circulation | volume = 67 | issue = 3 | pages = 632-9 | month = Mar | year = 1983 | doi = | PMID = 6821906 | URL = http://circ.ahajournals.org/content/67/3/632.full.pdf }}</ref> | ||
#Spongiosa. | #Spongiosa. | ||
#Fibrosa. | #Fibrosa. | ||
| Line 80: | Line 88: | ||
==Calcific aortic stenosis== | ==Calcific aortic stenosis== | ||
*Abbreviated ''CAS''. | *Abbreviated ''CAS''. | ||
{{Main|Calcific aortic stenosis}} | |||
==Localized dystrophic heart valve amyloidosis== | ==Localized dystrophic heart valve amyloidosis== | ||
| Line 145: | Line 117: | ||
==Myxomatous degeneration== | ==Myxomatous degeneration== | ||
{{Main|Myxomatous degeneration}} | |||
=Infective conditions= | =Infective conditions= | ||
==Rheumatic heart disease== | ==Rheumatic heart disease== | ||
{{Main|Rheumatic heart disease}} | |||
==Infective endocarditis== | ==Infective endocarditis== | ||
{{Main|Infective endocarditis}} | |||
=Non-infective conditions= | =Non-infective conditions= | ||
| Line 338: | Line 162: | ||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name=pmid3049284/><ref name=Ref_PCPBoD8_296>{{Ref PCPBoD8|296}}</ref> | Features:<ref name=pmid3049284/><ref name=Ref_PCPBoD8_296>{{Ref PCPBoD8|296}}</ref> | ||
*Increased thickness of spongiosa layer. | *Increased thickness of spongiosa layer. ‡ | ||
*Thinning of the fibrosa layer. | *Thinning of the fibrosa layer. | ||
*+/-Fibrin deposition - atrial aspect. | *+/-Fibrin deposition - atrial aspect. | ||
Notes: | |||
*‡ The Tthicking may be due to superimposed fibrosis, instead of spongiosa layer thickening.<ref name=pmid24316086>{{Cite journal | last1 = Roberts | first1 = WC. | last2 = Vowels | first2 = TJ. | last3 = Ko | first3 = JM. | last4 = Hebeler | first4 = RF. | title = Gross and histological features of excised portions of posterior mitral leaflet in patients having operative repair of mitral valve prolapse and comments on the concept of missing (= ruptured) chordae tendineae. | journal = J Am Coll Cardiol | volume = 63 | issue = 16 | pages = 1667-74 | month = Apr | year = 2014 | doi = 10.1016/j.jacc.2013.11.017 | PMID = 24316086 }}</ref> | |||
DDx: | DDx: | ||
| Line 377: | Line 204: | ||
===Gross=== | ===Gross=== | ||
*Vegetations anywhere on the valve surface<ref name=pmid19946116>{{Cite journal | last1 = Plastiras | first1 = SC. | last2 = Pamboucas | first2 = CA. | last3 = Tektonidou | first3 = M. | last4 = Toumanidis | first4 = ST. | title = Real-time three-dimensional echocardiography in evaluating Libman-Sacks vegetations. | journal = Eur J Echocardiogr | volume = 11 | issue = 2 | pages = 184-5 | month = Mar | year = 2010 | doi = 10.1093/ejechocard/jep172 | PMID = 19946116 }}</ref> - often seen on both sides (flow surface & non-flow surface).<ref>{{Ref PBoD8|567}}</ref> | *Vegetations anywhere on the valve surface<ref name=pmid19946116>{{Cite journal | last1 = Plastiras | first1 = SC. | last2 = Pamboucas | first2 = CA. | last3 = Tektonidou | first3 = M. | last4 = Toumanidis | first4 = ST. | title = Real-time three-dimensional echocardiography in evaluating Libman-Sacks vegetations. | journal = Eur J Echocardiogr | volume = 11 | issue = 2 | pages = 184-5 | month = Mar | year = 2010 | doi = 10.1093/ejechocard/jep172 | PMID = 19946116 }}</ref> - often seen on both sides (flow surface & non-flow surface).<ref>{{Ref PBoD8|567}}</ref> | ||
*Flat, pale brown/tan, usually small.<ref>URL: [http://library.med.utah.edu/WebPath/CVHTML/CV122.html http://library.med.utah.edu/WebPath/CVHTML/CV122.html]. Accessed on: 6 March 2013.</ref> | |||
Images: | |||
*[http://media.photobucket.com/image/nonbacterial%20thrombotic%20endocarditis/cat_at_uw/Osler%20-%20Cardiac/libman-sacks.jpg?t=1269402236 Libman-Sacks endocarditis (photobucket.com)]. | *[http://media.photobucket.com/image/nonbacterial%20thrombotic%20endocarditis/cat_at_uw/Osler%20-%20Cardiac/libman-sacks.jpg?t=1269402236 Libman-Sacks endocarditis (photobucket.com)]. | ||
*[http://library.med.utah.edu/WebPath/CVHTML/CV122.html Libman-Sacks endocarditis (utah.edu)]. | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 400: | Line 229: | ||
*Associated with ascending [[aortic aneurysm]]s - x10 risk of [[aortic dissection]] vs. normal population.<ref name=pmid18514024/> | *Associated with ascending [[aortic aneurysm]]s - x10 risk of [[aortic dissection]] vs. normal population.<ref name=pmid18514024/> | ||
*30% develop serious morbidity.<ref name=pmid18514024/> | *30% develop serious morbidity.<ref name=pmid18514024/> | ||
*Associated with early development of [[calcific aortic stenosis]]. | *Associated with early development of [[calcific aortic stenosis]] - often in 50s. | ||
**Calcific disease in normal (tricuspid) aortic valves is typically seen in the 70s. | |||
*[[Coarctation of the aorta]].<ref name=pmid16129122>{{Cite journal | last1 = Braverman | first1 = AC. | last2 = Güven | first2 = H. | last3 = Beardslee | first3 = MA. | last4 = Makan | first4 = M. | last5 = Kates | first5 = AM. | last6 = Moon | first6 = MR. | title = The bicuspid aortic valve. | journal = Curr Probl Cardiol | volume = 30 | issue = 9 | pages = 470-522 | month = Sep | year = 2005 | doi = 10.1016/j.cpcardiol.2005.06.002 | PMID = 16129122 }}</ref> | |||
===Gross=== | ===Gross=== | ||
| Line 417: | Line 248: | ||
*"No evidence of fusion."<ref name=Ref_AoGP>{{Ref AoGP|2}}</ref> | *"No evidence of fusion."<ref name=Ref_AoGP>{{Ref AoGP|2}}</ref> | ||
*Elastic fibres through-out (not interrupted by fibrous tissue). (???) | *Elastic fibres through-out (not interrupted by fibrous tissue). (???) | ||
Note: | |||
*The clinical impression and gross pathologic impression of bicuspid valve should concur. | |||
DDx: | DDx: | ||
*Senile [[calcific aortic stenosis]]. | *Senile [[calcific aortic stenosis]] with fusion of leaflets. | ||
===Sign out=== | |||
<pre> | |||
AORTIC VALVE, REPLACEMENT: | |||
- BICUSPID AORTIC VALVE WITH CALCIFIC STENOSIS. | |||
</pre> | |||
====Micro==== | |||
The sections show valve tissue with marked calcification of the fibrosa layer. No neutrophils are identified. No microorganisms are identified with routine stains. | |||
=Heart valve tumours= | =Heart valve tumours= | ||
{{main|Cardiac tumours}} | {{main|Cardiac tumours}} | ||
[[Papillary fibroelastoma]]s are the most common tumour of the valve. | [[Papillary fibroelastoma]]s are the most common tumour of the valve. | ||
=Other= | |||
==Subvalvular membrane== | |||
:''Subvalvular aortic membrane'' redirects here. | |||
===General=== | |||
*Rare. | |||
*May lead to [[sudden natural death]].<ref name=pmid16501359>{{Cite journal | last1 = Turan | first1 = AA. | last2 = Guven | first2 = T. | last3 = Karayel | first3 = F. | last4 = Pakis | first4 = I. | last5 = Gurpinar | first5 = K. | last6 = Ozaslan | first6 = A. | title = Subvalvular aortic stenosis as a cause of sudden death: two case reports. | journal = Am J Forensic Med Pathol | volume = 27 | issue = 1 | pages = 90-2 | month = Mar | year = 2006 | doi = 10.1097/01.paf.0000203301.96511.f7 | PMID = 16501359 }}</ref> | |||
Clinical: | |||
*Symptoms of aortic stenosis. | |||
*No ejection sound (as in aortic valvular stenosis).<ref name=pmid5817839>{{Cite journal | last1 = van der Schaar | first1 = PJ. | last2 = Roos | first2 = JP. | last3 = Rohmer | first3 = J. | title = Subvalvular membranous aortic stenosis. Results of surgical therapy. | journal = Thorax | volume = 24 | issue = 3 | pages = 276-82 | month = May | year = 1969 | doi = | PMID = 5817839 }}</ref> | |||
===Microscopic=== | |||
Features: | |||
*Fibrous tissue.<ref name=pmid16501359/><ref name=pmid21881724>{{Cite journal | last1 = Dearani | first1 = JA. | last2 = Croti | first2 = UA. | last3 = Price | first3 = TN. | last4 = Braile | first4 = DM. | title = Subvalvular aortic membrane resection. | journal = Rev Bras Cir Cardiovasc | volume = 26 | issue = 1 | pages = 135-6 | month = | year = | doi = | PMID = 21881724 }}</ref> | |||
Note: | |||
*Similar to valvular tissue. | |||
===Stains=== | |||
*[[Movat stain]]. | |||
===Sign out=== | |||
<pre> | |||
SUBVALVULAR MEMBRANE, AORTA, EXCISION: | |||
- BENIGN PAUCICELLULAR FIBROUS TISSUE CONSISTENT WITH SUBVALVULAR MEMBRANE. | |||
</pre> | |||
=See also= | =See also= | ||
Latest revision as of 01:14, 26 July 2016
Heart valves are the domain of the cardiac surgeon and their bread & butter.
Clinical
General
- Insufficiency (regurgitant flow) - murmur in diastole.
- Stenosis (decreased flow area) - murmur in systole.
Pathology
Which valves cause the most trouble?
- Mostly those on the left side (subjected to higher pressures), i.e. mitral valve (or left atrioventricular v.) and aortic valve.
Aortic stenosis - cause?
- Mostly "calcific aortic stenosis".
Quick approach to valves
Gross
- Calcification?
- Consider calcific stenosis.
- Vegetations?
- Consider infective endocarditis.
- Thin (see-through)?
- Consider myxomatous change.
Microscopic
- Inflammation?
- Consider endocarditis.
- Anitschkow's cells (caterpillar cells)?
- Rheumatic heart disease.
- Aschoff bodies?
- Rheumatic heart disease.
- Thickening of spongiosa (layer)?
- Myxomatous change?
Normal morphology
Aortic valve
General
- Covered by endothelium.
- Mostly avascular (nutrients supplied by diffusion).
Gross
Terminology:
- Base - closest to the aortic wall.
- Free edge - closest to the centre of the valve/interacts with other valve cusps.
Cusps:
- Left - has LMCA ostium.
- Right - has RCA ostium.
- Posterior (non-coronary cusp).
Note:
- The cut-up is described in grossing aortic valves.
Microscopic
Three layers (from proximal (ventricular side) to distal (valsalva side)):[1]
- Ventricularis.
- Elastic tissue.
- Spongiosa.
- Loose connective tissue.
- Fibrosa.
- Mostly collagen, thickest part in a normal valve.
Notes:
- The loading of the ventricular aspect is tensile and the valsalva side compressive. Thus, it makes sense that the tissue on the ventricular aspect is good in tensile loading and the tissue on the valsalva side good in compression. The elastic tissue can be thought of as rebar... the collagen as concrete.
Image:
Mitral valve
Gross
- Cordae tendinae.
- Should be thin.
- No fusion.
Note:
- The cut-up is described in grossing mitral valves.
Microscopic
Similar to the aortic valve - layers:
- Atrialis.[3]
- Spongiosa.
- Fibrosa.
Degenerative conditions
Calcific aortic stenosis
- Abbreviated CAS.
Localized dystrophic heart valve amyloidosis
General
- Common:
- ~75[4]-100%[5] of valves with calcific degeneration, i.e. calcific aortic stenosis.
- ~50% of valves with post-rheumatic sclerosis.[6]
- Not seen in acute disease and healed endocarditis.[6]
Hypothesis:
- Amyloid deposition in the aortic valve is the precursor lesion of calcific aortic stenosis.[5]
Microscopic
Features:[6]
- Pink amorphous material - key feature.
- Usually around the calcific foci.
DDx:
- Systemic amyloidosis, e.g. senile systemic amyloidosis, AL-amyloidosis.
Stains
- Congo red +ve.
Dystrophic amyloid:[6]
- Alcian blue -ve.
- Periodic acid-Schiff -ve.
Myxomatous degeneration
Infective conditions
Rheumatic heart disease
Infective endocarditis
Non-infective conditions
Mitral valve prolapse
General
- Classically young women.
- Afflicts ~ 3% of population in the USA.[8]
Clinical:
- Pansystolic murmur.
- +/-Left ventricular hypertrophy - secondary to MVP.
Complications:[8]
- Infective endocarditis.
- Congestive heart failure.
- Sudden cardiac death.[9]
- Thromboembolism.
Gross
Features - any of the following:[10]
- "Intrachordal hooding" = ballooning/bulging of leaflet between chordal attachments.
- Hooding or doming of the body of the leftlet into the left atrium.
- Extreme concavity of the valve when seen from the left ventricle.
- Elongated leaflets/large valve area.
- Dilated valve annulus.
- Thickening of the valve.
- +/-Left ventricular hypertrophy.
Note - location:
- Posterior leaflet pathology more common than anterior leaflet pathology.[10]
Image:
Microscopic
- Increased thickness of spongiosa layer. ‡
- Thinning of the fibrosa layer.
- +/-Fibrin deposition - atrial aspect.
Notes:
- ‡ The Tthicking may be due to superimposed fibrosis, instead of spongiosa layer thickening.[11]
DDx:
Nonbacterial thrombotic endocarditis
General
Associations:
Note:
- Marantic = wasting away.
Gross
- Round non-destructive vegetations, usually at the line of closure.[15]
Microscopic
Features:
- Vegetation without inflammation and microorganisms.
Libman-Sacks endocarditis
General
- Associated with systemic lupus erythematosus.
- Seen in approximately in 1/10 SLE cases by echocardiography.[16]
- Affects the mitral and aortic valves.[17]
- Mitral valve most commonly affected.[18]
- It has been suggested that it may be a manifestation of APLA syndrome.[17][18]
Clinical:
- Usually regurgitation.
Gross
- Vegetations anywhere on the valve surface[16] - often seen on both sides (flow surface & non-flow surface).[19]
- Flat, pale brown/tan, usually small.[20]
Images:
Microscopic
Features:[citation needed]
- Fibrin.
- No microorganisms.
- No inflammation.
Biscupid aortic valve
General
- Aortic valve usually tricuspid.
- Most common congenital heart defect.[21]
- Inherited in autosomal dominant pattern.
- NOTCH1 gene - implicated.[24]
Significance:
- Associated with ascending aortic aneurysms - x10 risk of aortic dissection vs. normal population.[22]
- 30% develop serious morbidity.[22]
- Associated with early development of calcific aortic stenosis - often in 50s.
- Calcific disease in normal (tricuspid) aortic valves is typically seen in the 70s.
- Coarctation of the aorta.[25]
Gross
Features - either:
Note:
- Raphe ~ suture or seam.[28]
Images:
Microscopic
Features - section through raphe:
- "No evidence of fusion."[26]
- Elastic fibres through-out (not interrupted by fibrous tissue). (???)
Note:
- The clinical impression and gross pathologic impression of bicuspid valve should concur.
DDx:
- Senile calcific aortic stenosis with fusion of leaflets.
Sign out
AORTIC VALVE, REPLACEMENT: - BICUSPID AORTIC VALVE WITH CALCIFIC STENOSIS.
Micro
The sections show valve tissue with marked calcification of the fibrosa layer. No neutrophils are identified. No microorganisms are identified with routine stains.
Heart valve tumours
Papillary fibroelastomas are the most common tumour of the valve.
Other
Subvalvular membrane
- Subvalvular aortic membrane redirects here.
General
- Rare.
- May lead to sudden natural death.[30]
Clinical:
- Symptoms of aortic stenosis.
- No ejection sound (as in aortic valvular stenosis).[31]
Microscopic
Features:
Note:
- Similar to valvular tissue.
Stains
Sign out
SUBVALVULAR MEMBRANE, AORTA, EXCISION: - BENIGN PAUCICELLULAR FIBROUS TISSUE CONSISTENT WITH SUBVALVULAR MEMBRANE.
See also
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 558. ISBN 0-7216-0187-1.
- ↑ URL: http://www.e-heart.org/pages/01_cardiac_structure/01_Cardiac_Structure_MV_003.htm. Accessed on: 20 December 2012.
- ↑ Chesler, E.; King, RA.; Edwards, JE. (Mar 1983). "The myxomatous mitral valve and sudden death.". Circulation 67 (3): 632-9. PMID 6821906.
- ↑ Kristen, AV.; Schnabel, PA.; Winter, B.; Helmke, BM.; Longerich, T.; Hardt, S.; Koch, A.; Sack, FU. et al. "High prevalence of amyloid in 150 surgically removed heart valves--a comparison of histological and clinical data reveals a correlation to atheroinflammatory conditions.". Cardiovasc Pathol 19 (4): 228-35. doi:10.1016/j.carpath.2009.04.005. PMID 19502085.
- ↑ 5.0 5.1 Falk, E.; Ladefoged, C.; Christensen, HE. (Jan 1981). "Amyloid deposits in calcified aortic valves.". Acta Pathol Microbiol Scand A 89 (1): 23-6. PMID 7223424.
- ↑ 6.0 6.1 6.2 6.3 Cooper, JH. (Jul 1983). "Localized dystrophic amyloidosis of heart valves.". Hum Pathol 14 (7): 649-53. PMID 6190729.
- ↑ Boudoulas, H.; Wooley, CF. (2001). "Floppy mitral valve/mitral valve prolapse/mitral valvular regurgitation: effects on the circulation.". J Cardiol 37 Suppl 1: 15-20. PMID 11433820.
- ↑ 8.0 8.1 8.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 296. ISBN 978-1416054542.
- ↑ Franchitto, N.; Bounes, V.; Telmon, N.; Rougé, D. (Jul 2010). "Mitral valve prolapse and out-of-hospital sudden death: a case report and literature review.". Med Sci Law 50 (3): 164-7. PMID 21133272.
- ↑ 10.0 10.1 10.2 Virmani, R.; Atkinson, JB.; Forman, MB. (Aug 1988). "The pathology of mitral valve prolapse.". Herz 13 (4): 215-26. PMID 3049284.
- ↑ Roberts, WC.; Vowels, TJ.; Ko, JM.; Hebeler, RF. (Apr 2014). "Gross and histological features of excised portions of posterior mitral leaflet in patients having operative repair of mitral valve prolapse and comments on the concept of missing (= ruptured) chordae tendineae.". J Am Coll Cardiol 63 (16): 1667-74. doi:10.1016/j.jacc.2013.11.017. PMID 24316086.
- ↑ 12.0 12.1 Borowski, A.; Ghodsizad, A.; Cohnen, M.; Gams, E. (Jun 2005). "Recurrent embolism in the course of marantic endocarditis.". Ann Thorac Surg 79 (6): 2145-7. doi:10.1016/j.athoracsur.2003.12.024. PMID 15919332.
- ↑ Young, RS.; Zalneraitis, EL.. "Marantic endocarditis in children and young adults: clinical and pathological findings.". Stroke 12 (5): 635-9. PMID 7303049.
- ↑ Dickens, P.; Chan, AC. (Apr 1991). "Nonbacterial thrombotic endocarditis in Hong Kong Chinese.". Arch Pathol Lab Med 115 (4): 359-61. PMID 2012496.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 567. ISBN 978-1416031215.
- ↑ 16.0 16.1 Plastiras, SC.; Pamboucas, CA.; Tektonidou, M.; Toumanidis, ST. (Mar 2010). "Real-time three-dimensional echocardiography in evaluating Libman-Sacks vegetations.". Eur J Echocardiogr 11 (2): 184-5. doi:10.1093/ejechocard/jep172. PMID 19946116.
- ↑ 17.0 17.1 Lee, JL.; Naguwa, SM.; Cheema, GS.; Gershwin, ME. (Jun 2009). "Revisiting Libman-Sacks endocarditis: a historical review and update.". Clin Rev Allergy Immunol 36 (2-3): 126-30. doi:10.1007/s12016-008-8113-y. PMID 19089657.
- ↑ 18.0 18.1 Hojnik, M.; George, J.; Ziporen, L.; Shoenfeld, Y. (Apr 1996). "Heart valve involvement (Libman-Sacks endocarditis) in the antiphospholipid syndrome.". Circulation 93 (8): 1579-87. PMID 8608627.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 567. ISBN 978-1416031215.
- ↑ URL: http://library.med.utah.edu/WebPath/CVHTML/CV122.html. Accessed on: 6 March 2013.
- ↑ Siu SC, Silversides CK (June 2010). "Bicuspid aortic valve disease". J. Am. Coll. Cardiol. 55 (25): 2789–800. doi:10.1016/j.jacc.2009.12.068. PMID 20579534.
- ↑ 22.0 22.1 22.2 Vallely MP, Semsarian C, Bannon PG (October 2008). "Management of the ascending aorta in patients with bicuspid aortic valve disease". Heart Lung Circ 17 (5): 357-63. doi:10.1016/j.hlc.2008.01.007. PMID 18514024.
- ↑ Tzemos, N.; Therrien, J.; Yip, J.; Thanassoulis, G.; Tremblay, S.; Jamorski, MT.; Webb, GD.; Siu, SC. (Sep 2008). "Outcomes in adults with bicuspid aortic valves.". JAMA 300 (11): 1317-25. doi:10.1001/jama.300.11.1317. PMID 18799444.
- ↑ Garg, V.; Muth, AN.; Ransom, JF.; Schluterman, MK.; Barnes, R.; King, IN.; Grossfeld, PD.; Srivastava, D. (Sep 2005). "Mutations in NOTCH1 cause aortic valve disease.". Nature 437 (7056): 270-4. doi:10.1038/nature03940. PMID 16025100.
- ↑ Braverman, AC.; Güven, H.; Beardslee, MA.; Makan, M.; Kates, AM.; Moon, MR. (Sep 2005). "The bicuspid aortic valve.". Curr Probl Cardiol 30 (9): 470-522. doi:10.1016/j.cpcardiol.2005.06.002. PMID 16129122.
- ↑ 26.0 26.1 Rose, Alan G. (2008). Atlas of Gross Pathology with Histologic Correlation (1st ed.). Cambridge University Press. pp. 2. ISBN 978-0521868792.
- ↑ Sabet, HY.; Edwards, WD.; Tazelaar, HD.; Daly, RC. (Jan 1999). "Congenitally bicuspid aortic valves: a surgical pathology study of 542 cases (1991 through 1996) and a literature review of 2,715 additional cases.". Mayo Clin Proc 74 (1): 14-26. doi:10.4065/74.1.14. PMID 9987528.
- ↑ URL: http://dictionary.reference.com/browse/raphe. Accessed on: 25 February 2012.
- ↑ Fedak, PW.; Verma, S.; David, TE.; Leask, RL.; Weisel, RD.; Butany, J. (Aug 2002). "Clinical and pathophysiological implications of a bicuspid aortic valve.". Circulation 106 (8): 900-4. PMID 12186790.
- ↑ 30.0 30.1 Turan, AA.; Guven, T.; Karayel, F.; Pakis, I.; Gurpinar, K.; Ozaslan, A. (Mar 2006). "Subvalvular aortic stenosis as a cause of sudden death: two case reports.". Am J Forensic Med Pathol 27 (1): 90-2. doi:10.1097/01.paf.0000203301.96511.f7. PMID 16501359.
- ↑ van der Schaar, PJ.; Roos, JP.; Rohmer, J. (May 1969). "Subvalvular membranous aortic stenosis. Results of surgical therapy.". Thorax 24 (3): 276-82. PMID 5817839.
- ↑ Dearani, JA.; Croti, UA.; Price, TN.; Braile, DM.. "Subvalvular aortic membrane resection.". Rev Bras Cir Cardiovasc 26 (1): 135-6. PMID 21881724.