Giardiasis
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Giardiasis | |
|---|---|
| Diagnosis in short | |
 Giardiasis. H&E stain. | |
|
| |
| LM | flagellate protozoa - pale/transluence on H&E, 12-15 micrometers (long axis) x 6-10 micrometers (short axis); +/-loss of villi, intraepithelial lymphocytes, inflammatory cells - especially close to the luminal surface |
| LM DDx | celiac disease |
| Stains | methylene blue +ve |
| IHC | CD117 +ve (microorganisms) |
| Site | duodenum |
|
| |
| Signs | diarrhea x5 days, foul smelling feces, flatulence |
| Symptoms | fatigue, abdominal cramps, nausea |
| Prevalence | uncommon |
| Endoscopy | +/-white spots, diffuse changes |
| Prognosis | good, benign |
| Clin. DDx | celiac disease, other causes of diarrhea |
| Treatment | antibiotics |
Giardiasis is a rare infection, classically found in the duodenum. It can mimic celiac disease. It is also known as beaver fever.
General
Clinical features - usually two or more of the following:[1]
- Diarrhea - x5 days.
- Flatulence.
- Foul smelling feces.
- Nausea.
- Abdominal cramps.
- Excessive tiredness.
Epidemiology:
- Uncommon.
Etiology:
- Flagellate protozoan Giardia lamblia.
Treatment
- Antibiotics, e.g. metronidazole (Flagyl).
Gross
- Diffuse changes.
- May have scattered white spots.[2]
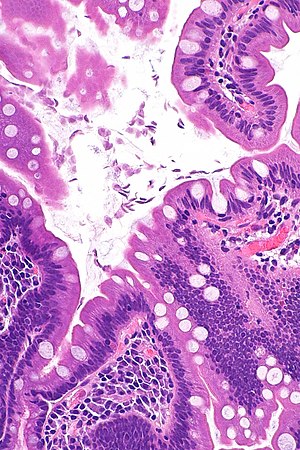
Microscopic
Features:
- +/-Loss of villi.
- Intraepithelial lymphocytes.
- +Other inflammatory cells, especially PMNs, close to the luminal surface.
- Flagellate protozoa -- diagnostic feature.
- Organisms often at site of bad inflammation.
- Pale/translucent on H&E.
- Size: 12-15 micrometers (long axis) x 6-10 micrometers (short axis) -- if seen completely.[3]
- Often look like a crescent moon (image of crescent moon) or semicircular[4] -- as the long axis of the organism is rarely in the plane of the (histologic) section.
Note:
- Changes are typically diffuse, i.e. if multiple biopsies are done the changes are present in all fragments.[5]
DDx:
- Celiac disease - near perfect mimic; missing giardia organisms.
Images
Case 1
Case 2
www
Stains
- Methylene blue +ve.[6]
IHC
- CD117 +ve.[7]
Sign out
A. Duodenum, Biopsy: - Abundant micro-organisms consistent with GIARDIA and small bowel mucosa with increased intraepithelial lymphocytes, see comment. - NEGATIVE for dysplasia. B. Stomach, Biopsy: - Body and antral-type mucosa with mild chronic inactive inflammation. - NEGATIVE for Helicobacter-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: The increased intraepithelial lymphocytes are likely to due to the Giardia; however, other causes cannot be excluded.
Block letters
DUODENUM, BIOPSY: - SMALL BOWEL MUCOSA WITH BRUNNER'S GLANDS AND MICROORGANISMS CONSISTENT WITH GIARDIA.
See also
References
- ↑ Hopkins, RS.; Juranek, DD. (Feb 1991). "Acute giardiasis: an improved clinical case definition for epidemiologic studies.". Am J Epidemiol 133 (4): 402-7. PMID 1994703.
- ↑ Biyikoğlu, I.; Babali, A.; Cakal, B.; Köklü, S.; Filik, L.; Astarci, MH.; Ustün, H.; Ustündağ, Y. et al. (Nov 2009). "Do scattered white spots in the duodenum mark a specific gastrointestinal pathology?". J Dig Dis 10 (4): 300-4. doi:10.1111/j.1751-2980.2009.00399.x. PMID 19906109.
- ↑ http://www.water-research.net/Giardia.htm
- ↑ http://en.wikipedia.org/wiki/Semicircle
- ↑ Freeman, HJ. (Mar 2008). "Pearls and pitfalls in the diagnosis of adult celiac disease.". Can J Gastroenterol 22 (3): 273-80. PMID 18354756.
- ↑ Rajurkar, MN.; Lall, N.; Basak, S.; Mallick, SK. (Nov 2012). "A simple method for demonstrating the giardia lamblia trophozoite.". J Clin Diagn Res 6 (9): 1492-4. doi:10.7860/JCDR/2012/4358.2541. PMID 23285438.
- ↑ Sinelnikov, I.; Sion-Vardy, N.; Shaco-Levy, R. (Mar 2009). "C-kit (CD117) immunostain is useful for the diagnosis of Giardia lamblia in duodenal biopsies.". Hum Pathol 40 (3): 323-5. doi:10.1016/j.humpath.2008.07.015. PMID 18835628.