Gastritis
| Gastritis | |
|---|---|
| Diagnosis in short | |
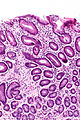
 Chronic gastritis. H&E stain. | |
|
| |
| LM | acute: PMNs in the lamina propria or intraepithelial; (usual) chronic: cluster of plasma cells (mild), several clusters (moderate), +/-mucosal erosions (severe); lymphocytic: intraepithelial lymphocytes (25 lymphocytes/100 epithelial cells) |
| Subtypes | acute gastritis, chronic gastritis, focal acute gastritis (pill gastritis), lymphocytic gastritis |
| LM DDx | Helicobacter gastritis, collagenous gastritis, Crohn's disease, intestinal metaplasia of the stomach, gastric columnar dysplasia, gastric carcinoma |
| Stains | Diff-Quik -ve, cresyl violet -ve |
| IHC | Helicobacter -ve |
| Site | stomach |
|
| |
| Associated Dx | intestinal metaplasia of the stomach - esp. in chronic gastritis |
| Clinical history | dyspepsia |
| Symptoms | upper abdominal pain |
| Prevalence | very common |
| Blood work | H. pylori -ve or previously +ve |
| Endoscopy | erythema |
| Prognosis | good |
| Other | neg. Helicobacter breath test |
| Clin. DDx | reactive gastropathy |
Gastritis refers to an inflammatory process that affects the stomach.
There are several types of gastritis:
- Chronic gastritis.
- Helicobacter pylori gastritis.
- Acute gastritis.
- "Chemical gastritis" - not really a gastritis; the preferred term is reactive gastropathy.
- Autoimmune gastritis.
- Lymphocytic gastritis.
- Collagenous gastritis.
This article gives an overview of causes of gastritis. It also deals with acute gastritis and the usual chronic gastritis without an apparent histologic cause, and lymphocytic gastritis.
General
- Very common.
- A specific cause is uncommonly identified histologically.
Clinical:
- Dyspepsia - esp. upper abdominal pain.
Etiology
Gastritis causes:[1]
- Infectious:
- H. pylori infection.
- Tuberculosis.
- Salmonellosis.
- CMV.
- Endocrine-related:
- Pernicious anemia.
- Diabetes mellitus - gastric atony.
- Trauma, e.g. NG tube.
- Vascular, ischemia.
- Autoimmune:
- Toxins:
- Radiation.
Endoscopic appearance
- Erythematous.
Microscopic
- Inflammatory cells - see below.
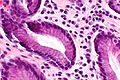
Acute gastritis
- AKA active gastritis.
Features:
- Neutrophils - especially when intraepithelial.
Focal active gastritis
DDx:
Chronic gastritis
Features:
- Plasma cells (in lamina propria).
- Various criteria:
- Two plasma cells kissing, i.e. two plasma cells touching/overlapping.
- Three is a crowd, i.e. three plasma cells in close proximity.
- Various criteria:
Note:
- Approximately 20% of cases with an inflamed cardia will have intestinal metaplasia.[3]
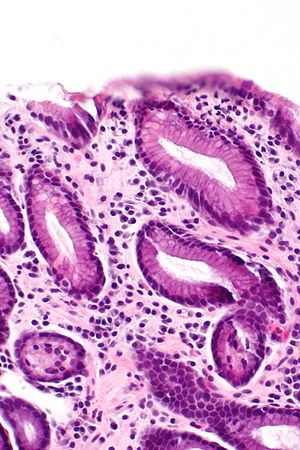
Images
Lymphocytic gastritis
General
The DDx is limited:
- Celiac disease - most common (39 of 82 cases in one series[4]).
- Helicobacter gastritis - common (30 of 82 cases in one series[4]).
- NSAIDs.[citation needed]
- Idiopathic.
- HIV/AIDS.
- Crohn's disease.
- Lymphoma.
Microscopic
Features:[5]
- 25 lymphocytes / 100 epithelial cells.
Sydney criteria for gastritis
A bunch of pathologists in Sydney came-up with criteria... and these were revised in Houston.[6]
Classification
Updated Sydney classification:[6]
| Feature | Non-atrophic Helicobacter | Atrophic Helicobacter | Autoimmune |
| Inflammation pattern | antral or diffuse | antrum & corpus, mild inflammation | corpus only |
| Atrophy & metaplasia | nil | atrophy present, metaplasia at incisura | corpus only |
Notes:
- Corpus = gastric body.
- Incisura = angular incisure, incisura angularis (Latin) - notched transition point on lesser curvature of the stomach between pylorus and body.[7]
Severity
The Sydney group suggests grading severity with the following language:[6]
- Mild.
- Moderate.
- Marked.
These terms are applied to the parameters described in a biopsy. The Sydney criteria lists H. pylori, neutrophils, mononuclear cells, antrum (atrophy), corpus (atrophy) and intestinal metaplasia. The paper that discusses this also give a visual analogue scale.
Parameters & Severity (adapted from Dixon et al.[6]):
| Feature | Mild | Moderate | Marked |
|---|---|---|---|
| H. pylori | few touching | many touching | piles |
| Neutrophils | few | bunches | crowded |
| Mononuclear cells | not touching | kissing | partying |
Sign out
Minimal chronic inactive
STOMACH, BIOPSY: - BODY AND ANTRAL-TYPE GASTRIC MUCOSA WITH MINIMAL CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR HELICOBACTOR-LIKE ORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Mild chronic inactive
Stomach, Antrum, Biopsy: - Antral-type gastric mucosa with mild chronic inactive inflammation. - NEGATIVE for Helicobacter-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Stomach, Antrum, Biopsy: - Antral-type gastric mucosa with mild focal chronic inactive inflammation, and mild focal gland tortousity without smooth muscle hyperplasia. - NEGATIVE for Helicobacter-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Block letters
STOMACH, BIOPSY: - BODY AND ANTRAL-TYPE GASTRIC MUCOSA WITH MILD CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR HELICOBACTOR-LIKE ORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Moderate chronic inactive antrum with mild chronic inactive body
STOMACH, BIOPSY: - ANTRAL-TYPE GASTRIC MUCOSA WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - BODY-TYPE GASTRIC MUCOSA WITH MILD CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR HELICOBACTOR-LIKE ORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Moderate chronic active
STOMACH, BIOPSY: - Body and antral-type gastric mucosa with moderate chronic active inflammation. - NEGATIVE for Helicobacter-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Block letters
STOMACH, BIOPSY: - BODY AND ANTRAL-TYPE GASTRIC MUCOSA WITH MODERATE CHRONIC ACTIVE INFLAMMATION. - NEGATIVE FOR HELICOBACTOR-LIKE ORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Sleeve gastrectomy
Partial Stomach, Sleeve Gastrectomy: - Stomach wall with focal mild chronic inactive inflammation of the mucosa. - NEGATIVE for Helicobactor-like organisms. - NEGATIVE for intestinal metaplasia. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Block letters
STOMACH, GREATER CURVATURE, SLEEVE GASTRECTOMY: - STOMACH WALL WITH FOCAL MILD CHRONIC ACTIVE INFLAMMATION OF THE MUCOSA. - NEGATIVE FOR HELICOBACTOR-LIKE ORGANISMS. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro - inactive
The sections show gastric body type mucosa with small clusters of plasma cells. There are no intraepithelial neutrophils. Goblet cells are not identified. The epithelium matures normally to the surface. No Helicobacter organisms are seen.
See also
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 812-3. ISBN 0-7216-0187-1.
- ↑ Parfitt, JR.; Driman, DK. (Apr 2007). "Pathological effects of drugs on the gastrointestinal tract: a review.". Hum Pathol 38 (4): 527-36. doi:10.1016/j.humpath.2007.01.014. PMID 17367604.
- ↑ Voutilainen, M.; Färkkilä, M.; Mecklin, JP.; Juhola, M.; Sipponen, P. (Nov 1999). "Chronic inflammation at the gastroesophageal junction (carditis) appears to be a specific finding related to Helicobacter pylori infection and gastroesophageal reflux disease. The Central Finland Endoscopy Study Group.". Am J Gastroenterol 94 (11): 3175-80. doi:10.1111/j.1572-0241.1999.01513.x. PMID 10566710.
- ↑ 4.0 4.1 Wu, TT.; Hamilton, SR. (Feb 1999). "Lymphocytic gastritis: association with etiology and topology.". Am J Surg Pathol 23 (2): 153-8. PMID 9989841.
- ↑ El-Zimaity. 18 October 2010.
- ↑ 6.0 6.1 6.2 6.3 Dixon MF, Genta RM, Yardley JH, Correa P (October 1996). "Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994". Am. J. Surg. Pathol. 20 (10): 1161-81. PMID 8827022. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0147-5185&volume=20&issue=10&spage=1161.
- ↑ http://en.wikipedia.org/wiki/Angular_incisure