Epilepsy
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
Epilepsy is a common chronic seizure disorder.
General
- Epilepsy = seizures that are "idiopathic", i.e. no brain tumour, no mass lesion, no brain injury.
- Most common form: temporal lobe epilepsy.[1]
Etiology
- Many.
- Cortical dysplasia.
- Hamartia.
- Stroke.
- Infection.
- Head trauma.
Syndromic:
Tumour:
- Dysembryoplastic neuroepithelial tumour.[2]
- Ganglioglioma.[3]
- Isomorphic astrocytoma.
Types
Features:[4]
- Temporal lobe epilepsy
- Mesial temporal sclerosis = scarring of the medial temporal lobe.
- Involves: hippocampus, parahippocampal gyrus and amygdala.
- Granule cell dispersion
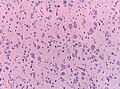
Hamartia
- Small collection of ectopic glioneuronal cells.
- Morpholology resembling oligodendroglial-like cells. [5]
- Mostly amygdala, less common in hippocampus or temporal lobe.
- Can coexist with focal cortical dysplasia.
Focal cortical dysplasia (FCD)
- Localized malformations of the cortex.
- Frequently associated with epilepsy in children.
- Includes cortical dyslamination, cytoarchitectural changes and white matter abnormalities.
- Current consensus: ILAE classification scheme 2011 [6](based on previous classification by Palmini 2004):
- Type I FCD (focal)
- Ia: Abnormal radial cortical lamination.
- Ib: Abnormal tangential cortical lamination.
- Ic: Abnormal radial and tangential cortical lamination.
- Type II FCD (focal)
- IIa: Presence of dysmorphic neurons.
- IIb: Presence of dysmorphic neurons and balloon cells.
- Type III FCD (associated with other lesion)
- IIIa: FCD associated with hippocampal sclerosis.
- IIIb: FCD adjacent to a brain tumor.
- IIIc: FCD adjacent to vascular malformation.
- IIIc: FCD associated with previous injury (trauma, inflammation...).
Hippocampal sclerosis
- Most frequent histopathology in temporal lobe epilepsy (33% of all epilepsy surgery specimen).
- ILAE classification for hippocampus specimen:[7]
- ILAE type 1: cell loss predominantly in CA1 and CA4 sectors.
- ILAE type 2: predominant CA1 neuron loss and gliosis.
- ILAE type 3: CA4 predominant neuronal cell loss and gliosis.
Clinic: ILAE type 1: benefit from epilepsy surgery.
Notes:
- Gliosis withot neuronal loss is not considered hippocampal sclerosis.
Granule cell dispersion
- Affects dentate gyrus.
- Observed in up to 40% specimen with hippocampal sclerosis.
- Clinico-pathological classification:[8]
- Granule cell pathology (GCP) Type 1: Substantial granule cell loss.
- Granule cell pathology (GCP) Type 2: Cell dispersion, ectopic neurons or clusters of neurons in the molecular layer or bi-lamination.
Clinic:
- Association with longer epilepsy duration.
DDx:
- Epilepsy.
- Dementia.
Mild Malformation of Cortical Development with Oligodendroglial Hyperplasia
- Abbreviated: MOGHE [9].
- Frontal lobe.
- Nonlesional (3.7% of epilepsy case).
- Increase cellularity of Olig2-, and PDGFR-alpha-immunoreactive oligodendroglia.
Sudden unexpected death in epilepsy
- Abbreviated SUDEP.
Diagnosis:
- Negative autopsy.
- History of epilepsy.
Epidemiology:[10]
- Typically poorly controlled epilepsy.
- Incidence: 0.09-9 per 1000 patient-years.
See also
References
- ↑ URL: http://emedicine.medscape.com/article/342150-overview. Accessed on: 20 November 2010.
- ↑ Cataltepe, O.; Turanli, G.; Yalnizoglu, D.; Topçu, M.; Akalan, N. (Apr 2005). "Surgical management of temporal lobe tumor-related epilepsy in children.". J Neurosurg 102 (3 Suppl): 280-7. doi:10.3171/ped.2005.102.3.0280. PMID 15881751.
- ↑ Im, SH.; Chung, CK.; Cho, BK.; Lee, SK. (Mar 2002). "Supratentorial ganglioglioma and epilepsy: postoperative seizure outcome.". J Neurooncol 57 (1): 59-66. PMID 12125968.
- ↑ MUN. 15 November 2010.
- ↑ Kasper, BS.; Stefan, H.; Buchfelder, M.; Paulus, W. (Jan 1999). "Temporal lobe microdysgenesis in epilepsy versus control brains.". J Neuropathol Exp Neurol 58 (1): 22-8. PMID 10068310.
- ↑ Blümcke, I.; Aronica, E.; Miyata, H.; Sarnat, HB.; Thom, M.; Roessler, K.; Rydenhag, B.; Jehi, L. et al. (Mar 2016). "International recommendation for a comprehensive neuropathologic workup of epilepsy surgery brain tissue: A consensus Task Force report from the ILAE Commission on Diagnostic Methods.". Epilepsia 57 (3): 348-58. doi:10.1111/epi.13319. PMID 26839983.
- ↑ Blümcke, I.; Thom, M.; Aronica, E.; Armstrong, DD.; Bartolomei, F.; Bernasconi, A.; Bernasconi, N.; Bien, CG. et al. (Jul 2013). "International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a Task Force report from the ILAE Commission on Diagnostic Methods.". Epilepsia 54 (7): 1315-29. doi:10.1111/epi.12220. PMID 23692496.
- ↑ Blümcke, I.; Kistner, I.; Clusmann, H.; Schramm, J.; Becker, AJ.; Elger, CE.; Bien, CG.; Merschhemke, M. et al. (May 2009). "Towards a clinico-pathological classification of granule cell dispersion in human mesial temporal lobe epilepsies.". Acta Neuropathol 117 (5): 535-44. doi:10.1007/s00401-009-0512-5. PMID 19277686.
- ↑ Schurr, J.; Coras, R.; Rössler, K.; Pieper, T.; Kudernatsch, M.; Holthausen, H.; Winkler, P.; Woermann, F. et al. (01 2017). "Mild Malformation of Cortical Development with Oligodendroglial Hyperplasia in Frontal Lobe Epilepsy: A New Clinico-Pathological Entity.". Brain Pathol 27 (1): 26-35. doi:10.1111/bpa.12347. PMID 26748554.
- ↑ Tomson, T.; Nashef, L.; Ryvlin, P. (Nov 2008). "Sudden unexpected death in epilepsy: current knowledge and future directions.". Lancet Neurol 7 (11): 1021-31. doi:10.1016/S1474-4422(08)70202-3. PMID 18805738.