Epidermal necrosis
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
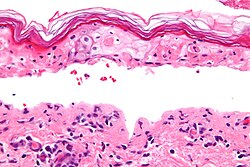
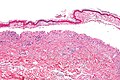
Confluent epidermal necrosis. H&E stain.
Epidermal necrosis is an important finding in dermatopathology. Full-thickness necrosis, especially is very serious.
General
Full thickness DDx:
- Erythema multiform (EM).
- Toxic epidermal necrolysis (TEN).
- Stevens-Johnson syndrome (SJS).
- Trauma.
- Others. (???)
Partial thickness DDx:
- Staphylococcal scalded skin syndrome.
- Trauma. (???)
- Others. (???)
Notes:
- SJS and TEN are on a spectrum, EM (depending on who you ask) is considered separate.
- These are signed-out as "confluent epidermal necrosis - see comment".
- Comment: The histomorphologic findings are consistent with EM/SJS/TEN.
- The clinical DDx of EM/SJS/TEN includes acute generalized exanthematous pustulosis (AGEP).
- These are signed-out as "confluent epidermal necrosis - see comment".
Erythema multiforme
- Abbreviated EM.
General
Features:[1]
- Hypersensitivity disorder due to a drug or infection.
- Associated with the following: HSV, Mycoplasma, Histoplasma, others.
Clinical:
- Target-like lesion.
Microscopic
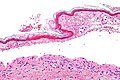
Features:[1]
- Lymphocytic interface dermatitis (lymphocytes at the dermal-epidermal junction).
- Necrotic/degenerative keratinocytes - key feature.
- +/-Epidermal blistering.
- +/-Epidermal sloughing.
Images
Stevens-Johnson syndrome
- Abbreviated SJS.
General
Rx causes of SJS:
- NSAIDs.
- Anticonvulsants.
- Sulfonamides.
- Penicillins.
Microscopic
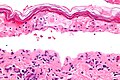
Features:
- Similar erythema multiforme.
Images
Toxic epidermal necrolysis
- Abbreviated TEN.
General
- TEN more severe form SJS.
Definition:
- >30% sheet-like epidermal detachment, diffuse erythema, severe mucous membrane involvement.
- Most TEN (80%) Rx-related, only 50% of SJS Rx-related.
Microscopic
Features:
- Like erythema multiforme - but usu. less inflammation.[2]
Images
Staphylococcal scalded skin syndrome
- Abbreviated SSSS.
General
- Due to keratinocyte cell-cell adhesion loss in the superficial epidermis - caused by S. aureus.[3]
Clinical:
- Blisters
Microscopic
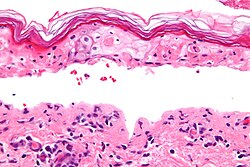
Features:[3]
- Superficial dermis separates from underlying tissue - looks artefactual.
- Minimal/scant inflammation is typical.[4]
Image:
See also
- Dermatopathology - an introduction to the topic.
- Non-malignant skin disease.
- Inflammatory skin disease.
References
- ↑ 1.0 1.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1189. ISBN 978-1416031215.
- ↑ S. Sade. 8 September 2011.
- ↑ 3.0 3.1 Nishifuji, K.; Sugai, M.; Amagai, M. (Jan 2008). "Staphylococcal exfoliative toxins: "molecular scissors" of bacteria that attack the cutaneous defense barrier in mammals.". J Dermatol Sci 49 (1): 21-31. doi:10.1016/j.jdermsci.2007.05.007. PMID 17582744.
- ↑ URL: http://dermatlas.med.jhmi.edu/derm/display.cfm?ImageID=2105774586. Accessed on: 22 September 2011.