Diverticular disease
Jump to navigation
Jump to search
| Diverticular disease | |
|---|---|
| Diagnosis in short | |
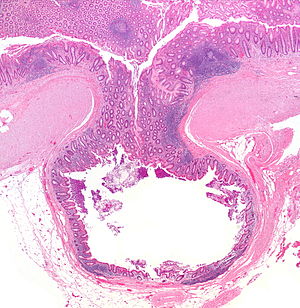 Diverticulum. H&E stain. | |
|
| |
| LM | mucosa/submucosa invaginate into the musuclaris propria |
| Gross | outpouching - best seen after sectioning |
| Grossing notes | partial colectomy for diverticular disease |
| Site | colon - classically sigmoid, other sites |
|
| |
| Associated Dx | diverticulitis, peritonitis, diverticular disease-associated colitis |
| Symptoms | usu. asymptomatic, diverticulitis presents with abdominal pain - classically left lower quadrant |
| Prevalence | common - especially elderly |
| Radiology | colonic outpouchings (typically sigmoid colon) +/-pericolic stranding |
| Clin. DDx | colorectal carcinoma, epiploic appendagitis |
| Treatment | usually conservative, surgical resection (recurrent or perforating diverticulitis) |
Diverticular disease, also diverticulosis, is a common disease of the colon. Inflammation of diverticula is known as diverticulitis.
General
- Very common.
- Typically seen in elderly patients - 50s and 60s.
- Weakly associated with adenomatous polyps (odd ratio ~ 1.03) - probably due to shared causality (i.e. diet).[1]
Presentations:
- Incidental finding on imaging.
- Abdominal pain.
- Classically left lower quadrant.
- +/-Peritoneal signs.
- Blood per rectum.
- Large bowel obstruction.
Complications:
- Diverticulitis - seen in ~25% of individuals with divertiulosis.[2]
- Peformation - peritonitis.
- Diverticular-associated colitis - see below.
- Bowel obstruction - not common, may mimic malignancy.[3]
Diverticular disease-associated colitis
Features:[4]
- Rare.
- Definitions vary somewhat - one is: IBD-like inflammation restricted to areas with diverticular disease.
- Considerable overlap with IBD histologically - no definite histologic findings.
- Rectal biopsy may be used to differentiate from ulcerative colitis.
Gross
- Corrugated - like cardboard.
- Wall thickening (reactive).[5]
- Usually sigmoid colon.
- May be elsewhere, e.g. appendix.[6]
Images
Microscopic
Features:
- Mucosa/submucosa invagination into the musuclaris propria (MP).
- At the site the blood vessels supplying the mucosa and submucosa penetrate the MP.[7]
Notes:
- Crypt disortion and/or granulomas should not be seen.[8]
DDx:
- Colorectal carcinoma - may cause a stricture, usually obvious on microscopy.
- Inflammatory bowel disease.
Images
www:
Sign out
Sternberg's Diagnostic Surgical Pathology suggests using the term diverticular disease instead of trying to distinguish between diverticulosis and diverticulitis, as diverticulitis clinically may be seen without objective evidence of inflammation.[10]
- This is reasonable, considering that (1) sampling in large specimens may miss the definite active inflammation, and (2) the distinction is academic, as the management is not driven by this detail of the pathologic findings.
Sigmoid Colon, Sigmoidectomy: - Diverticular disease with surrounding fibrosis and small focus of active mucosal inflammation. - Four benign lymph nodes. - NEGATIVE for malignancy.
Block letters
SIGMOID COLON, SIGMOIDECTOMY: - DIVERTICULAR DISEASE WITHOUT EVIDENCE OF ACTIVE DIVERTICULITIS. - NEGATIVE FOR MALIGNANCY.
SIGMOID COLON WITH EEA DONUTS, SIGMOIDECTOMY: - DIVERTICULAR DISEASE WITHOUT EVIDENCE OF ACTIVE DIVERTICULITIS. - ONE BENIGN SMALL LYMPH NODE. - NEGATIVE FOR MALIGNANCY.
Perforated
RECTO-SIGMOID, LARGE BOWEL RESECTION: - PERFORATED DIVERTICULITIS WITH SEROSITIS AND ABSCESS FORMATION. - SUBMUCOSAL FIBROSIS. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR MALIGNANCY.
SIGMOID COLON, RESECTION: - COLONIC PERFORATION ASSOCIATED WITH FAT NECROSIS, SEROSITIS AND MICROABSCESS FORMATION, IN THE SETTING OF DIVERTICULAR DISEASE. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ Lim, YJ.; Nanto, S.; Masuyama, T.; Kohama, A.; Kodama, K.; Kitabatake, A.; Kamada, T. (Dec 1989). "[Evaluation of function of human collateral coronary arteries using myocardial contrast echocardiography].". J Cardiol 19 (4): 973-9. PMID 2486634.
- ↑ Agarwal, AK.; Karanjawala, BE.; Maykel, JA.; Johnson, EK.; Steele, SR. (Sep 2014). "Routine colonic endoscopic evaluation following resolution of acute diverticulitis: is it necessary?". World J Gastroenterol 20 (35): 12509-16. doi:10.3748/wjg.v20.i35.12509. PMID 25253951.
- ↑ Pereira, JM.; Sirlin, CB.; Pinto, PS.; Jeffrey, RB.; Stella, DL.; Casola, G.. "Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain.". Radiographics 24 (3): 703-15. doi:10.1148/rg.243035084. PMID 15143223.
- ↑ Mulhall, AM.; Mahid, SS.; Petras, RE.; Galandiuk, S. (Jun 2009). "Diverticular disease associated with inflammatory bowel disease-like colitis: a systematic review.". Dis Colon Rectum 52 (6): 1072-9. doi:10.1007/DCR.0b013e31819ef79a. PMID 19581849.
- ↑ Nicholson, BD.; Hyland, R.; Rembacken, BJ.; Denyer, M.; Hull, MA.; Tolan, DJ. (Aug 2011). "Colonoscopy for colonic wall thickening at computed tomography: a worthwhile pursuit?". Surg Endosc 25 (8): 2586-91. doi:10.1007/s00464-011-1591-7. PMID 21359889.
- ↑ Sohn, TJ.; Chang, YS.; Kang, JH.; Kim, DH.; Lee, TS.; Han, JK.; Kim, SH.; Hong, YO. (Jan 2013). "Clinical characteristics of acute appendiceal diverticulitis.". J Korean Surg Soc 84 (1): 33-7. doi:10.4174/jkss.2013.84.1.33. PMID 23323233.
- ↑ West, AB.. "The pathology of diverticulitis.". J Clin Gastroenterol 42 (10): 1137-8. doi:10.1097/MCG.0b013e3181862a9f. PMID 18936652.
- ↑ Goldstein, NS.; Ahmad, E. (Apr 1997). "Histology of the mucosa in sigmoid colon specimens with diverticular disease: observations for the interpretation of sigmoid colonoscopic biopsy specimens.". Am J Clin Pathol 107 (4): 438-44. PMID 9124212.
- ↑ URL: http://histology-group28.wikispaces.com/DigestiveSystemProject. Accessed on: 23 August 2011.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 1346. ISBN 978-0781779425.


