Congestive hepatopathy
Congestive hepatopathy is a type of medical liver disease caused by right heart failure.
General
- Liver failure due to (right) heart failure.
- AKA cardiac cirrhosis - a term used by clinicians.
- Generally, it does not satisfy pathologic criteria for cirrhosis.[1]
Gross
- "Nutmeg" liver - yellow spotted appearance.
Microscopic
Features:[2]
- Zone III atrophy.
- Portal venule (central vein) distension.
- Perisinusoidal fibrosis - progresses to centrilobular fibrosis and then diffuse fibrosis.
- Dilation of sinusoids in all zone III areas - key feature.[3]
DDx:
- Hemangioma of the liver - should be focal lesion.
Cardiac (congestive) hepatopathy, wherein outflow obstruction occurs secondary to backflow from a failing heart, and Budd Chiari syndrome, wherein obstruction of outflow occurs secondary to obstruction, usually thrombotic, have overlapping features, including sinusoidal dilation with emphasis upon the central vein, space of Disse erythrocytes, centrilobular inflammation, hemorrhage, bile ductules, and hemosiderin, and portal inflammation, fibrosis and bile ductular reaction. Centrilobular dropout/necrosis is more common in Budd Chiari syndrome, while peri-central venous and sinusoidal fibrosis are more common in cardiac hepatopathy. In end stage liver, fibrosis for cardiac hepatopathy comprises stellate centrizonal fibrous with haphazard spread, as opposed to the more frequent nodular cirrhosis in Budd-Chiari. Clinical findings are important to take into account, as cardiac failure is usually well known at the time of diagnosis as are the clinical predictors of Budd Chiari syndrome, prothrombotic states, myeloproliferative diseases, and oral contraceptive use. [4]
Images
A.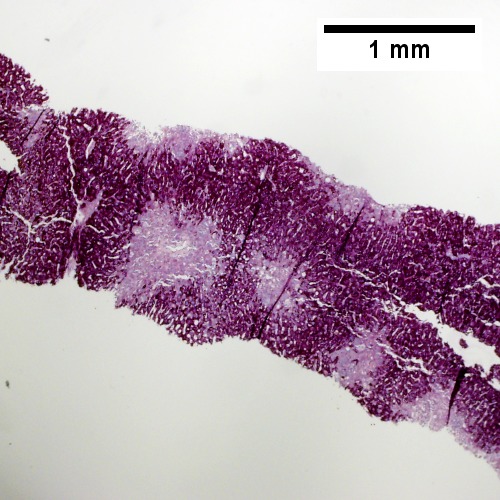
|
B.![Necrosis with central vein [yellow arrowhead], inflammatory cells, residual Councilman body [green arrowhead], and hepatocyte with mitotic figure [red arrowhead] (400X).](/w/images/thumb/0/08/2_CEN_NEC_1_680x512px.tif/lossy-page1-500px-2_CEN_NEC_1_680x512px.tif.jpg)
|
C.![Trichrome highlights fibrosis about central vein [yellow arrowhead] & shows beginning scar formation [green arrowheads]. Note residual atrophic hepatocytes [blue arrowheads] (400X).](/w/images/thumb/0/06/3_CEN_NEC_1_680x512px.tif/lossy-page1-500px-3_CEN_NEC_1_680x512px.tif.jpg)
|
D.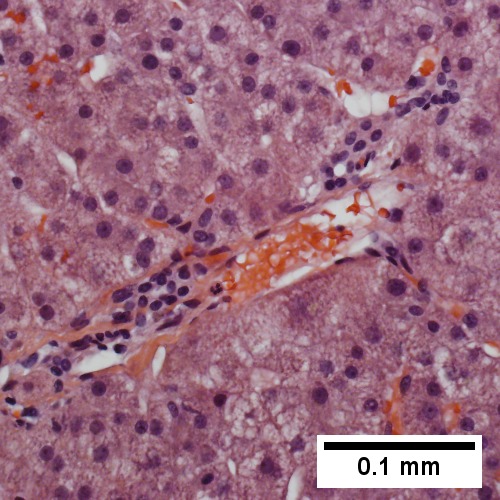
|
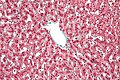
Centrilobular necrosis (seen in circulatory failure and with toxins/drugs). A. PAS without diastase shows ovoids of necrosis. B. Necrosis with central vein [yellow arrowhead], inflammatory cells, residual Councilman body [green arrowhead], and hepatocyte with mitotic figure [red arrowhead]. C. Trichrome highlights fibrosis about central vein [yellow arrowhead] & shows beginning scar formation [green arrowheads]. Note residual atrophic hepatocytes [blue arrowheads]. D. Portal triads are largely unaffected (LR 400X)
A.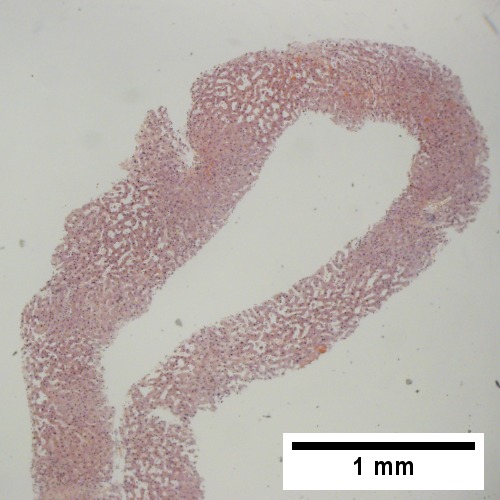
|
B.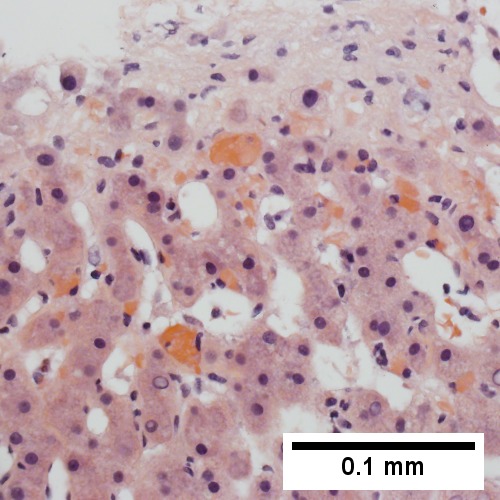
|
C.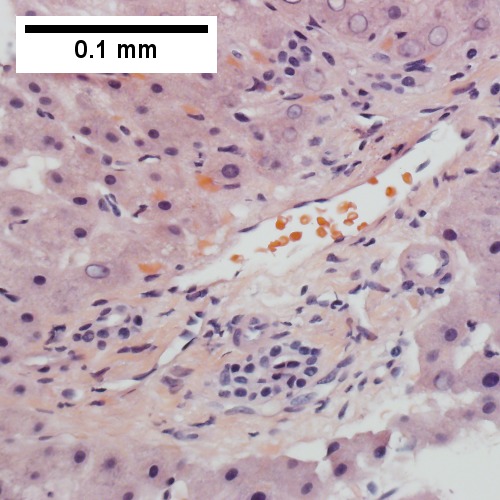
|
D.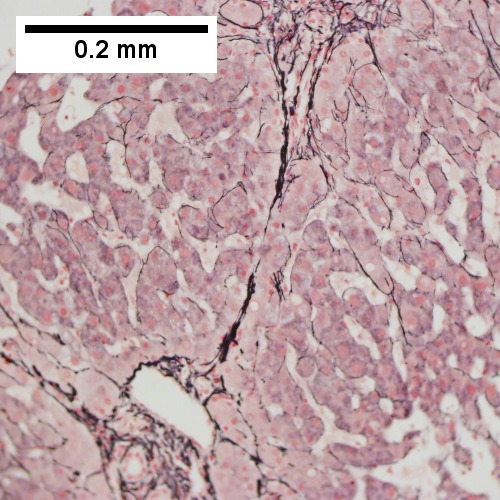
|
E.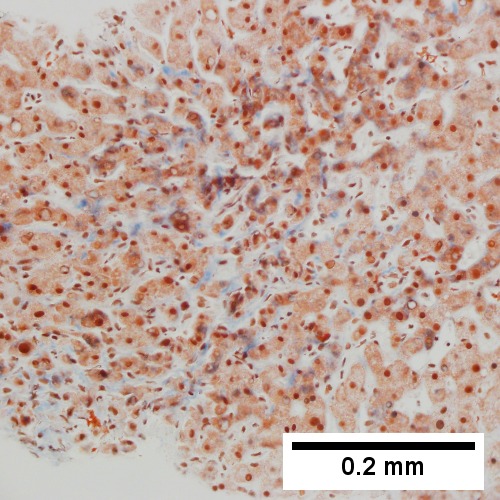
|
F.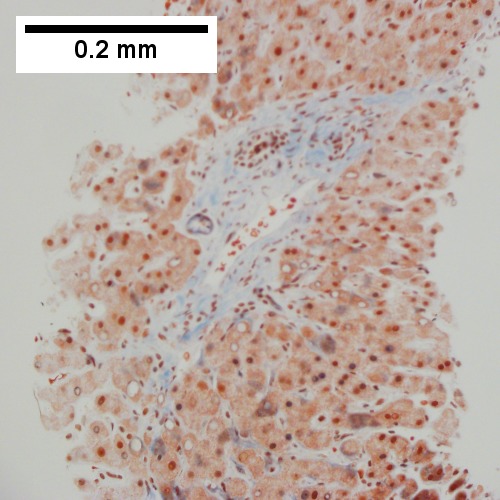
|
Patient with congestive heart failure and stage I fibrosis. A. Dilated and undilated sinusoidal regions. B. Thrombi in sinusoids; glycogenated nuclei likely reflect patient’s diabetes mellitus. C. Dilated portal vein. D. Reticulin shows black lines of bridging, too thick for collapse. E. Trichrome shows space of Disse collagenization (pericellular fibrosis). F. Trichrome shows bridge beginning off to right; when it is more than a mere spike, it is a bridge.
See also
References
- ↑ URL: http://emedicine.medscape.com/article/151792-overview. Accessed on: 17 June 2010.
- ↑ URL: http://emedicine.medscape.com/article/151792-diagnosis. Accessed on: 17 June 2010.
- ↑ Suggested by OA. September 2009.
- ↑ Gonzalez RS, Gilger MA, Huh WJ, Washington MK (2017). [http http://www.archivesofpathology.org/doi/10.5858/arpa.2015-0388-OA?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed&code=coap-site "The spectrum of histologic findings in hepatic outflow obstruction"]. Arch Pathol Lab Med 141: 98. doi:10.5858/arpa.2015-0388-OA. PMID 27681331. http http://www.archivesofpathology.org/doi/10.5858/arpa.2015-0388-OA?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed&code=coap-site.