Cervical polyps
Cervical polyps are common entities that can be bothersome and are thus removed by a gynecologist. The vast majority are benign. An introduction to the uterine cervix is in the uterine cervix article.
Benign endocervical polyp
- Endocervical polyp redirects here.
General
- Usually 30-50 years old.
- May cause bleeding.
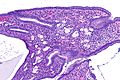
Microscopic
Features:[1]
- May have mixed epithelium, i.e. squamous and endocervical type (with eosinophilic mucin).
- Endocervical epithelium should have nuclei like that in the colon, i.e. small, round & basal.
- Polypoid shape.
- +/-Inflammation.
- +/-Squamous metaplasia.
Negatives:
- No mitoses.
- No nuclear atypia.
- No stromal proliferation.
Notes:
- No histologic features separate cervical polyps from benign endocervical mucosa; ergo, they are often signed-out as "... consistent with cervical polyp."
DDx:
- Benign endometrial polyp.
- Fibroepithelial stromal polyp.
- Adenosarcoma.
- Papillary adenofibroma of the uterine cervix.[2]
- Nabothian cysts.
Images
Sign out
CERVICAL POLYP, EXCISION: - CONSISTENT WITH BENIGN ENDOCERVICAL POLYP.
CERVICAL POLYP, EXCISION: - CONSISTENT WITH BENIGN ENDOCERVICAL POLYP WITH ACUTE AND CHRONIC INFLAMMATION.
CERVICAL POLYP, EXCISION: - CONSISTENT WITH BENIGN ENDOCERVICAL POLYP WITH AN EROSION AND INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
Significant squamous epithelium present
CERVICAL POLYP, EXCISION: - BENIGN CERVICAL POLYP WITH ACUTE AND CHRONIC INFLAMMATION.
History provided
CERVICAL POLYP, EXCISION: - BENIGN ENDOCERVICAL POLYP.
Papillary adenofibroma of the uterine cervix
General
- Rare.[2]
Clinical:[2]
Gross
- Polypoid mass.
DDx:
Microscopic
Features:
- Branching nipple like projections (papillae) covered by endocervical epithelium +/- metaplastic squamous epithelium.
- Fibrous stroma.
DDx:
Fibroepithelial stromal polyp
General
- Usually easy to recognize.[4]
Microscopic
Features:[4]
- Bland nuclei.
- Hypocellular.
Note:
- The Foundation series books appears to lump together fibroepithelial stromal polyp and pseudosarcomatous fibroepithelial stromal polyp.
- Features as per Foundation series book:[5]
- Polypoid lesions.
- Squamous epithelium.
- Variable cellularity.
- Multinucleated cells.
- Features as per Foundation series book:[5]
Image:
Pseudosarcomatous fibroepithelial stromal polyp
General
- Uncommon.
- Wide age range.
- May be misdiagnosed as a sarcoma and overtreated.[4]
- Similar lesions in vagina and vulva.
Microscopic
Features:[4]
- Hypercellularity.
- Marked nuclear pleomorphism (common).
- +/-High mitotic rate ( > 10 mitoses / 10 HPF).
- +/-Atypical mitoses.
- No identifiable margin between lesion and normal - important feature.
- Scattered multinucleated stromal cells - usu. close to epithelium.
DDx:
IHC
- Desmin +ve (common).
- SMA usu. -ve.
Adenosarcoma
Main article: Adenosarcoma
See also
References
- ↑ URL: http://pathologyoutlines.com/cervix.html#endocervpolyp. Accessed on: 22 October 2011.
- ↑ 2.0 2.1 2.2 Fratini, D.; Cavaliere, A. (Apr 1996). "Papillary adenofibroma of the uterine cervix. A case report.". Pathologica 88 (2): 135-6. PMID 8927449.
- ↑ Haberal, A.; Cil, AP.; Gunes, M.; Cavusoglu, D. (Aug 2005). "Papillary adenofibroma of the cervix: a case report.". Ultrasound Obstet Gynecol 26 (2): 186-7. doi:10.1002/uog.1948. PMID 16041681.
- ↑ 4.0 4.1 4.2 4.3 Nucci, MR.; Young, RH.; Fletcher, CD. (Feb 2000). "Cellular pseudosarcomatous fibroepithelial stromal polyps of the lower female genital tract: an underrecognized lesion often misdiagnosed as sarcoma.". Am J Surg Pathol 24 (2): 231-40. PMID 10680891.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 31. ISBN 978-0443069208.