Difference between revisions of "Breast pathology"
(create) |
(→Columnar cell change: split out) |
||
| (330 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
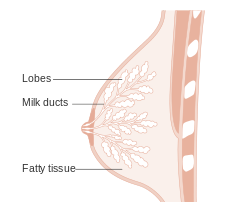
''' | [[Image:Diagram showing the lobes and ducts of a breast CRUK 307.svg|thumb|250px|Diagram of the structure of breast. (CRUK/WC)]] | ||
The '''breast''' is an important organ that [[pathologist]]s see quite often because it is often afflicted by [[breast cancer|cancer]]. Before women started [[smoking]] in large numbers, it was a leading cause of cancer death in women. | |||
Fortunately, breast cancer, | Fortunately, breast cancer, in this day, has a relatively good prognosis if it is detected early. | ||
=Clinical= | |||
===Clinical Presentations of Breast Pathology=== | |||
==Clinical== | *'''Abnormal/suspicious screening mammogram''' | ||
**Suspicious microcalcifications and/or suspicious mass. | |||
**Most common history on the specimen requisition | |||
**May be accompanied by a [[BI-RADS]] score. | |||
*Nipple discharge. | *Nipple discharge. | ||
*Pain. | *Pain. | ||
| Line 12: | Line 15: | ||
*New nipple inversion. | *New nipple inversion. | ||
*Skin changes, e.g. ''peau d'orange''. | *Skin changes, e.g. ''peau d'orange''. | ||
===Breast cancer screening=== | ===Breast cancer screening=== | ||
| Line 23: | Line 23: | ||
# The incidence of breast cancer is lower. | # The incidence of breast cancer is lower. | ||
==Normal | ===Breast radiology=== | ||
*Glands -- normally has two cell layers (like the [[prostate]]) | {{Main|Breast imaging reporting and data system}} | ||
=Specimens= | |||
Three major specimen types: | |||
#Core needle biopsy (CNB). | |||
#Lumpectomy. | |||
#Modified radical mastectomy. | |||
Note: | |||
*Breast [[cytopathology]] is dealt with in the ''[[breast cytopathology]]'' article. Breast cytology is almost extinct unless you happen to be in Australia where for reasons unknown, the art is still taken seriously. Breast cytology is not sensitive or specific enough to justify forgoing a CNB. | |||
===Core needle biopsy=== | |||
Work-up of CNBs is dependent on the clinical abnormality:<ref>MUA. 1 October 2010.</ref> | |||
#Mass lesion - usu. obvious what is going on; typically 3 levels. | |||
#Calcifications - abnormality may be very small; typically 10 levels. | |||
Note - if you have a high BI-RADS score on the biopsy requisition, and no correlating histologic findings, be sure to correlate with the specimen radiograph, consider leveling the specimen to exhaustion and/or note the lack of a correlating lesion on your report. | |||
===Lumpectomy=== | |||
Lumpectomies are usually oriented with short and long suture; '''s'''hort is typically '''s'''uperior (aspect) and '''l'''ong is typically '''l'''ateral (aspect). | |||
===Modified radical mastectomy=== | |||
*Usually done with sentinel [[lymph node]] biopsy - as one cannot go back later to do this. | |||
=Where to start= | |||
{{Main|Short_power_list#Breast_pathology|Long_power_list#Breast_pathology}} | |||
The following is a starting point for mentally framing routine breast pathology & some of the challenges in breast pathology: | |||
The key to breast pathology is the myoepithelial cell. | |||
**A benign gland has two cell layers - myoepithelial and epithelial. | |||
**The luminal cell is epithelial | |||
**The basal cells is myoepithelial | |||
***The myoepithelial layer is hard to see at times. | |||
***IHC can aid in visualizing the myoepithelial layer. | |||
***The immunostains used in breast pathology for the myoepithelial layer include: [[CK5/6]], SMA, [[p63]] and calponin. | |||
===Questions to Ask=== | |||
*Is it normal or close to normal? | |||
**Are you familiar with normal/altered but benign/physiologic changes in the breast? | |||
**Do the changes observed explain the biopsy (are you sure you are seeing the radiographic lesion)? | |||
**Have you found the microcalcifications? | |||
*Is it a neoplastic but benign? | |||
**Are you familiar with the common benign breast neoplasms? | |||
**Do you know the morphologic criteria for a benign breast gland? | |||
**Do you know how to use IHC to confirm a benign process? | |||
*Is it an in situ carcinoma? | |||
**Are you familiar with DCIS and LCIS and their variants? | |||
**Do you know the morphologic criteria for in situ carcinoma? | |||
**Do you know how to use ICH to confirm an in situ carcinoma? | |||
**Do you know how to report an in situ breast carcinoma? | |||
*Is it invasive carcinoma? | |||
**Do you know the morphologic criteria for an invasive gland? | |||
**Do you know how to use IHC to confirm invasion? | |||
**Do you know the morphologic features of typical invasive breast carcinoma? | |||
**Do you know the subtypes? | |||
**Do you understand the implications of some of the medullary/medullary-like subtype (especially in a young patient)? | |||
**Do you know how to use IHC for prognostication? | |||
**Do you understand the implications of triple negativity? | |||
**Do you know how to report an invasive breast carcinoma? | |||
*Is it something stromal/spindled? | |||
===Important Differential Diagnoses=== | |||
====Papillary Lesions==== | |||
*Nipple adenoma. | |||
*Intraductal papilloma. | |||
*Papillary ductal carcinoma in situ. | |||
*Intracystic papillary carcinoma. | |||
*Intracystic papillary carcinoma with an invasive component. | |||
*Invasive papillary carcinoma. | |||
====Basaloid Lesions==== | |||
*Adenoid cystic carcinoma of the breast. | |||
*Intracystic papillary breast carcinoma, solid variant. | |||
*Invasive papillary breast carcinoma, solid variant. | |||
*Medullary breast carcinoma. | |||
*Medullary-like breast carcinoma. | |||
**Know when to start a discussion about BRCA mutations, triple negativity and the 'basal-like molecular phenotype'. | |||
====Spindle Cell Lesions==== | |||
*Metaplastic breast carcinoma. | |||
*Treated breast carcinoma. | |||
*Mammary myofibroblastoma. | |||
*Phyllodes Tumour - stromal component. | |||
*Desmoid fibromatosis. | |||
*Nodular fasciitis. | |||
=== Additional resources === | |||
*Breast Pathology Info [http://www.breastpathology.info/] | |||
*Digital Atlas of Breast Pathology [http://www.hsc.stonybrook.edu/breast-atlas/] | |||
*Pathology Outlines - Breast Nonmalignant [http://pathologyoutlines.com/breast.html] | |||
*Pathology Outlines - Breast Malignant [http://pathologyoutlines.com/breastmalignant.html] | |||
*WebPathology - Breast [http://www.webpathology.com/atlas_map.asp?section=9] | |||
=Normal breast= | |||
==Resting breast== | |||
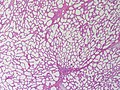
*Glands -- normally has two cell layers (like the [[prostate]]). | |||
**Myoepithelial cells | **Myoepithelial cells | ||
***Frequently spindle-like, often hard to see. | ***Frequently spindle-like, often hard to see. | ||
| Line 33: | Line 133: | ||
May be present: | May be present: | ||
*Calcification: | *[[Breast calcifications|Calcification]]: | ||
**Purple globs (with concentric rings) on H&E = calcium phosphate. | **Purple globs (with concentric rings) on H&E = calcium phosphate. | ||
***Q. How to remember? A. '''P'''urple = '''P'''hosphate. | ***Q. How to remember? A. '''P'''urple = '''P'''hosphate. | ||
**Calcium oxalate visible with (light) polarization - not | **Calcium oxalate visible with (light) [[polarization]] - not associated with [[breast cancer|malignancy]]. | ||
**Often in the lumen of a gland, may be in the stroma. | **Often in the lumen of a gland, may be in the stroma. | ||
**Calcific material typically has a well-demarcated border +/- "sharp corners". | **Calcific material typically has a well-demarcated border +/- "sharp corners". | ||
**Radiologists can pick-up calcs (calcifications) that are approximately 100 micrometers; if "calcs" is on the requisition one needs to find calcs this size.<ref>MUA. 1 October 2010.</ref> | |||
***The large calcs seen on radiology are approximately 1/5 - 1/6 the size of a HPF, if the field of view (FOV) is ~0.55 mm (as is the case with 22 mm-10x eye pieces and a 40x objective). | |||
Notes: | |||
*The architecture is more important than the cytologic features in the diagnosis of malignancy in the breast;<ref>RS. 4 May 2010.</ref> low grade tumours have distorted architecture but normal/near normal cytology. | |||
Image | ===Image=== | ||
*[http://www.breastpathology.info/Images/calcs/FatNec1_700.jpg Breast with calcifications (breastpathology.info)]. | *[http://www.breastpathology.info/Images/calcs/FatNec1_700.jpg Breast with calcifications (breastpathology.info)]. | ||
*[http://www.wjso.com/content/7/1/70/figure/F3 Resting breast tissue (wjso.com)]. | |||
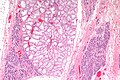
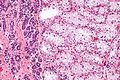
==Lactational changes== | |||
*[[AKA]] secretory change, [[AKA]] lactational adenoma, [[AKA]] lactating adenoma <ref>URL: [Breast_pathology#Lactational_changes Breast_pathology#Lactational_changes. Accessed on: 3 October 2011.</ref> | |||
===General=== | |||
*Lactational adenoma generally arises in during or in the few weeks after pregnancy. | |||
*May be present focally in non-pregnant females. | |||
*"Lactational adenoma"- circumscribed mass displacing the normal breast architecture (hyperplasia plus functional/physiologic change) | |||
*"Lactational change"- normal breast tissue architecture preserved (functional/physiologic change). | |||
ASIDE: | |||
* | *Some believe ''lactational change'' and ''secretory change'' aren't the same... | ||
**Lactational change = only in lactation. | |||
**Secretory change = other times. | |||
*This hair splitting is clinically irrelevant-- both are benign. Also, experts use the terms interchangeably.<ref name=pmid2879437>{{Cite journal | last1 = Tavassoli | first1 = FA. | last2 = Yeh | first2 = IT. | title = Lactational and clear cell changes of the breast in nonlactating, nonpregnant women. | journal = Am J Clin Pathol | volume = 87 | issue = 1 | pages = 23-9 | month = Jan | year = 1987 | doi = | PMID = 2879437 }} | |||
</ref> | |||
===Microscopic=== | |||
Features:<ref>URL: [http://flylib.com/books/en/2.953.1.9/1/ http://flylib.com/books/en/2.953.1.9/1/]. Accessed on: 6 August 2011.</ref> | |||
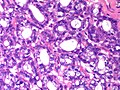
*Glands dilated. | |||
*Increased number of lobules. | |||
**Relative decrease in intralobular and extralobular stroma. | |||
*Luminal cells enlarged. | |||
**Vacuolated cytoplasm. | |||
**[[Hobnail morphology]] - hang into the lumen. | |||
*Myoepithelial cells indistinct - after second trimester. | |||
*Lactational "adenoma" may undergo infarction - Imagine what an infarcted lactational adenoma could look like in a FNA specimen! | |||
DDx: | |||
*[[Secretory carcinoma of the breast]]. | |||
====Images==== | |||
<gallery> | |||
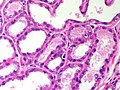
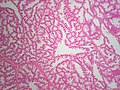
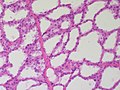
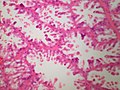
Image:Lactational_change_-_low_mag.jpg | Lactational change - low mag. (WC/Nephron) | |||
Image:Lactational_change_-_high_mag.jpg | Lactational change - high mag. (WC/Nephron) | |||
Image:Breast LactationalChange MP CTR.jpg|Breast - Lactational Change - medium power (SKB) | |||
Image:Breast LactationalChange HP CTR.jpg|Breast - Lactational Change - high power (SKB) | |||
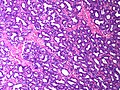
Image:Breast LactationalAdenoma MP CTR.jpg|Breast - Lactational adenoma - medium power (SKB) | |||
Image:Breast LactationalAdenoma HP CTR.jpg|Breast - Lactational adenoma - high power (SKB) | |||
Image:Breast LactationalAdenoma LP SNP.jpg|Breast - Lactational adenoma - low power (SKB) | |||
Image::Breast LactationalAdenoma MP SNP.jpg|Breast - Lactational adenoma - high power (SKB) | |||
Image:Breast LactatingAdenoma (4) PA.JPG|Breast - Lactational adenoma - low power (SKB) | |||
Image:Breast LactationalAdenoma MP SNP.jpg|Lactational adenoma - high power - in this example, the epithelium is flattened with clear bubbly cytoplasm (SKB) | |||
Image:Breast LactatingAdenoma HP PA.JPG|Breast - Lactational adenoma - high power - shows snouting and decapitation secretion. (SKB) | |||
</gallery> | |||
== | www: | ||
* | *[http://www.gfmer.ch/selected_images_v2/detail_list.php?cat1=2&cat2=9&cat3=0&cat4=3&stype=n Lactational changes (gfmer.ch)]. | ||
*[http://www.webpathology.com/image.asp?case=320&n=7 Lactational changes in an angiosarcoma of the breast (webpathology.com)]. | |||
*[http://www.lab.anhb.uwa.edu.au/mb140/CorePages/FemaleRepro/femalerepro.htm#LabMamm Lactating breast (uwa.edu.au)]. | |||
* | |||
== | ==Major Pathologic Patterns== | ||
===General | ===General classification=== | ||
<!-- | <!-- | ||
BREAST PATHOLOGY - SIMPLE | BREAST PATHOLOGY - SIMPLE | ||
| Line 90: | Line 205: | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | A | | | | | | | | | | | |A='''Breast pathology'''}} | {{familytree | | | | | | | | | | | A | | | | | | | | | | | |A='''Breast pathology'''}} | ||
{{familytree | | | | |,|-|-|-|-|-|-| | {{familytree | | | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|.| | | | | |}} | ||
{{familytree | | | | B | | | | | | {{familytree | | | | B | | | | | X | | | | |C | | | | |B=Stromal<br>pathology|X=Miscellaneous|C=Glandular<br>pathology}} | ||
{{familytree | |,|-|-|^|-|-|.| | | | | | |,|-|-|-|+|-|-|-|.| |}} | {{familytree | |,|-|-|^|-|-|.| | | | | | |,|-|-|-|+|-|-|-|.| |}} | ||
{{familytree | D | | | | E | | | | | F | | G | | H |D=Myxoid|E=Long slit-like<br>spaces|F=Simple<br>epithelium|G=Dilated|H=Cellular | {{familytree | D | | | | E | | | | | F | | G | | H |D=Myxoid|E=Long slit-like<br>spaces|F=Simple<br>epithelium|G=Dilated|H=[[Breast pathology#Cellular lesions|Cellular lesions]]}} | ||
{{familytree | |!| | | |,|-|^|-|.| | | | |!| | | |!| | | |!| |}} | {{familytree | |!| | | |,|-|^|-|.| | | | |!| | | |!| | | |!| |}} | ||
{{familytree | I | | J | | K | | | L | | M | | N |I=Fibroadenoma|J=Malignant<br>features|K=Benign features|L=Tubular<br>carcinoma|M=FEA, FCC,<br>CCC|N= | {{familytree | I | | J | | K | | | L | | M | | N |I=[[Fibroadenoma]]|J=Malignant<br>features|K=Benign features|L=[[Tubular carcinoma of the breast|Tubular<br>carcinoma]]|M=[[FEA]], [[FCC]],<br>[[Columnar cell change|CCC]]|N=[[FEHUT]], Neoplastic,<br>Malignant}} | ||
{{familytree | | | | | |!| | | |!| | | | | | | | | | | | | | |}} | {{familytree | | | | | |!| | | |!| | | | | | | | | | | | | | |}} | ||
{{familytree | | | | | O | | P | | | | | | | | | | | | | ||O=Malignant<br>phyllodes|P=Benign phyllodes | {{familytree | | | | | O | | P | | | | | | | | | | | | | ||O=[[Phyllodes tumour|Malignant<br>phyllodes]]|P=[[Phyllodes tumour|Benign phyllodes]]}} | ||
{{familytree/end}} | {{familytree/end}} | ||
Notes: | Notes: | ||
* | *The challenges in breast pathology are in: the ''Simple epithelium'' category and the ''Cellular lesions'' category. | ||
*''Neoplastic'' includes: ADH | *''Neoplastic'' includes: ADH and LDH. | ||
*''Malignant'' includes: DCIS, LCIS, ductal carcinoma (DC) and lobular carcinoma (LC), papillary lesions. | *''Malignant'' includes: DCIS, LCIS, ductal carcinoma (DC) and lobular carcinoma (LC), some papillary lesions. | ||
*''Lobular carcinoma'' (a '''pitfall''') may appear to be a stromal problem, i.e. the stroma looks too cellular. | *''Lobular carcinoma'' (a '''pitfall''') may appear to be a stromal problem, i.e. the stroma looks too cellular. | ||
* | *''Miscellaneous'' includes rare tumours of the breast that do not fit into another category, i.e. [[metastases]], [[lymphoma]]s, [[melanoma]], sarcomas. Skin-related pathology is dealt within the ''[[dermatologic neoplasms]]'' article. ''[[Paget disease of the breast]]'', which may be seen in the context of malignant breast lesions, is discussed in its own article. | ||
===Cellular lesions=== | ===Cellular lesions=== | ||
| Line 112: | Line 227: | ||
--> | --> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | C | | | | | | | | |C='''Cellular lesions'''}} | {{familytree | | | | | | | | | | | | | C | | | | | | | | |C='''Cellular lesions<br>(Glandular)'''}} | ||
{{familytree | | | | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| |}} | {{familytree | | | | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| |}} | ||
{{familytree | | | | | SP | | SS | | DE | | SF | | FC |SP=Equal spacing,<br>punched-out|SS=Streaming, periph. <br>slit-like spaces.|DE=Discohesive cells,<br>expanded gl.|SF=Single cells<br>or single file|FC=Fibrovascular<br>cores}} | {{familytree | | | | | SP | | SS | | DE | | SF | | FC |SP=Equal spacing,<br>punched-out|SS=Streaming, periph. <br>slit-like spaces.|DE=Discohesive cells,<br>expanded gl.|SF=Single cells<br>or single file|FC=Fibrovascular<br>cores}} | ||
{{familytree | | | | | |!| | | |!| | | |!| | | |!| | | |!| |}} | {{familytree | | | | | |!| | | |!| | | |!| | | |!| | | |!| |}} | ||
{{familytree | | | | | DL | | | {{familytree | | | | | DL | | FEHUT | | LL | | LC | | PL |DL=Ductal lesion|FEHUT=[[FEHUT]]|LL=Lobular lesion|LC=[[Invasive lobular carcinoma|Lobular carcinoma]]|PL=[[Breast pathology#Papillary lesions|Papillary lesions]]}} | ||
{{familytree | | | |,|-|^|-|.| | | |,|-|^|-|.| | | | | | | |}} | {{familytree | | | |,|-|^|-|.| | | |,|-|^|-|.| | | | | | | |}} | ||
{{familytree | | | TL | | OL | | LTF | | GTF | | | | | | |TL=Two cell layers|OL=One cell layer|LTF=<50% of gl.|GTF=>50% of gl.}} | {{familytree | | | TL | | OL | | LTF | | GTF | | | | | | |TL=Two cell layers|OL=One cell layer|LTF=<50% of gl.|GTF=>50% of gl.}} | ||
{{familytree | | | |!| | | |!| | | |!| | | |!| | | | | | | |}} | {{familytree | | | |!| | | |!| | | |!| | | |!| | | | | | | |}} | ||
{{familytree | | | DNI | | DC | | | {{familytree | | | DNI | | DC | | ALH | | LCIS | | | | | | |DNI=Ductal non-inv.<br>neoplasm|DC=[[Invasive ductal carcinoma of the breast|Ductal carcinoma]]|ALH=[[ALH]]|LCIS=[[LCIS]]}} | ||
{{familytree | |,|-|^|-|.| | | | | | | | | | | | | | | | | |}} | {{familytree | |,|-|^|-|.| | | | | | | | | | | | | | | | | |}} | ||
{{familytree | LE | | SE | | | | | | | | | | | | | | | | |LE=Large extent|SE=Small extent}} | {{familytree | LE | | SE | | | | | | | | | | | | | | | | |LE=Large extent|SE=Small extent}} | ||
{{familytree | |!| | | |!| | | | | | | | | | | | | | | | | |}} | {{familytree | |!| | | |!| | | | | | | | | | | | | | | | | |}} | ||
{{familytree | DCIS | | ADH | | | | | | | | | | | | | | | | |DCIS=DCIS|ADH=ADH}} | {{familytree | DCIS | | ADH | | | | | | | | | | | | | | | | |DCIS=[[DCIS]]|ADH=[[ADH]]}} | ||
{{familytree/end}} | {{familytree/end}} | ||
Notes: | Notes: | ||
*The largest challenge is: differentiating between the first two categories on level 2, i.e. ''equal spacing | *The largest challenge is: differentiating between the first two categories on level 2, i.e. ''equal spacing' vs. ''streaming''. | ||
*The ''fibrovascular cores'' must arise from a tuft, i.e. if they are arising directly from the wall of glands only it is likely ''papillary DCIS''. | |||
===Papillary lesions=== | ===Papillary lesions=== | ||
| Line 140: | Line 256: | ||
{{familytree | D | | | | | | E | | | | | | F |D=Unremarkable<br>papillae|E=Atypia ''or'' arch. abnorm.<br>''or'' cellular proliferation|F=Neoplastic cells<br>present}} | {{familytree | D | | | | | | E | | | | | | F |D=Unremarkable<br>papillae|E=Atypia ''or'' arch. abnorm.<br>''or'' cellular proliferation|F=Neoplastic cells<br>present}} | ||
{{familytree | |!| | | |,|-|-|-|+|-|-|-|.| | | |!| |}} | {{familytree | |!| | | |,|-|-|-|+|-|-|-|.| | | |!| |}} | ||
{{familytree | G | | H | | I | | J | | K |G=Benign<br>intraductal<br>papilloma|H=High grade atypia|I=Low grade atypia<br>''or'' abnorm. arch.|J=''Only'' cellular<br>proliferation|K=Intracystic<br> (encapsulated)<br>papillary ca.}} | {{familytree | G | | H | | I | | J | | K |G=[[intraductal papilloma of the breast|Benign<br>intraductal<br>papilloma]]|H=High grade atypia|I=Low grade atypia<br>''or'' abnorm. arch.|J=''Only'' cellular<br>proliferation|K=[[Encapsulated papillary carcinoma of the breast|Intracystic<br> (encapsulated)<br>papillary ca.]]}} | ||
{{familytree | | | | | |!| | | |!| | | |!| | | | | |}} | {{familytree | | | | | |!| | | |!| | | |!| | | | | |}} | ||
{{familytree | | | | | L | | |!| | | N | | | | |L=DCIS in<br>papilloma|N= | {{familytree | | | | | L | | |!| | | N | | | | |L=[[DCIS]] in<br>papilloma|N=[[FEHUT]] in<br>papilloma}} | ||
{{familytree | | | | | | | |,|-|^|-|.| | | | | | | |}} | {{familytree | | | | | | | |,|-|^|-|.| | | | | | | |}} | ||
{{familytree | | | | | | | P | | Q | | | | | | |P=>3 mm extent|Q=<3 mm extent}} | {{familytree | | | | | | | P | | Q | | | | | | |P=>3 mm extent|Q=<3 mm extent}} | ||
{{familytree | | | | | | | |!| | | |!| | | | | | | |}} | {{familytree | | | | | | | |!| | | |!| | | | | | | |}} | ||
{{familytree | | | | | | | R | | S | | | | | | |R=DCIS in<br>papilloma|S=ADH in<br>papilloma}} | {{familytree | | | | | | | R | | S | | | | | | |R=DCIS in<br>papilloma|S=[[ADH]] in<br>papilloma}} | ||
{{familytree/end}} | {{familytree/end}} | ||
Notes: | Notes: | ||
*Adapted from ''Mulligan & O'Malley''.<ref>{{cite journal |author=Mulligan AM, O'Malley FP |title=Papillary lesions of the breast: a review |journal=Adv Anat Pathol |volume=14 |issue=2 |pages=108–19 |year=2007 |month=March |pmid=17471117 |doi=10.1097/PAP.0b013e318032508d |url=}}</ref> | *Adapted from ''Mulligan & O'Malley''.<ref>{{cite journal |author=Mulligan AM, O'Malley FP |title=Papillary lesions of the breast: a review |journal=Adv Anat Pathol |volume=14 |issue=2 |pages=108–19 |year=2007 |month=March |pmid=17471117 |doi=10.1097/PAP.0b013e318032508d |url=}}</ref> | ||
| Line 153: | Line 270: | ||
*''abnorm. arch.'' = abnormal architecture present. | *''abnorm. arch.'' = abnormal architecture present. | ||
*''DCIS'' = ductal carcinoma in situ. | *''DCIS'' = ductal carcinoma in situ. | ||
*'' | *''FEHUT'' = florid epithelial hyperplasia of the usual type. | ||
*''extent'' refers to the size of the abnormal cell population within the papillary lesion. | *''extent'' refers to the size of the abnormal cell population within the papillary lesion. | ||
=Malignant lesions= | |||
==Non-invasive breast cancer== | ==Non-invasive breast cancer== | ||
{{main|Non-invasive breast cancer}} | {{main|Non-invasive breast cancer}} | ||
| Line 164: | Line 282: | ||
This is includes descriptions of the usual types... and the not so common ones. | This is includes descriptions of the usual types... and the not so common ones. | ||
= | =Common benign lesions= | ||
The breast has lots of benign things. Unlike the prostate, the where benign is called ''benign'', everything has a name. It is more common among breast pathologists to sign-out things like: ''apocrine metaplasia'' (benign), ''columnar cell change'' (benign), and ''epithelial hyperplasia of the usual type ( | The breast has lots of benign things. Unlike the prostate, the where benign is called ''benign'', everything has a name. It is more common among breast pathologists to sign-out things like: ''apocrine metaplasia'' (benign), ''columnar cell change'' (benign), and ''florid epithelial hyperplasia of the usual type (FEHUT)'' - instead of - ''benign breast tissue''. | ||
==Mild epithelial hyperplasia== | |||
===General=== | |||
*No increased risk of malignancy. | |||
**Often ''not'' reported - as it has no clinical signficance. | |||
*Has to be separated from ''[[moderate epithelial hyperplasia]]'' / ''[[florid epithelial hyperplasia]]''. | |||
===Microscopic=== | |||
Features:<ref>{{Ref BP|159-160}}</ref> | |||
*Breast glands with three ''or'' four cell layers above the basement membrane. | |||
*Variable cells. | |||
Note: | |||
*No nuclear atypia. | |||
DDx: | |||
*[[Flat epithelial atypia]]. | |||
*[[Moderate epithelial hyperplasia]] / [[florid epithelial hyperplasia]]. | |||
*[[Atypical ductal hyperplasia]]. | |||
==Apocrine metaplasia== | ==Apocrine metaplasia== | ||
{{Main|Apocrine metaplasia of the breast}} | |||
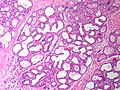
==Duct ectasia== | |||
*Dilation of large ducts secondary to luminal obstruction by inspissated secretions | |||
*Presentation | |||
* | **~age 40-50, possibly with cheesy nipple discharge | ||
** | *Pathology | ||
**Duct lumen dilated and containing foamy macrophages | |||
**Necrosis/shedding of epithelium | |||
**If duct rupture: chronic and granulomatous inflammation of periductal region | |||
**Fibrotic thickening of duct wall | |||
<gallery> | |||
Image:Breast DuctEctasia LP PA.JPG|Breast - Duct Ectasia - low power (SKB) | |||
Image:Breast DuctEctasia MP2 PA.JPG|Breast - Duct Ectasia - low power (SKB) | |||
Image:Breast DuctEctasia MP PA.JPG|Breast - Duct Ectasia - medium power (SKB) | |||
</gallery> | |||
== | ==Fibrocystic change== | ||
* | {{Main|Breast fibrocystic changes}} | ||
*[[AKA]] ''fibrocystic changes'' (abbreviated ''FCC''). | |||
==Columnar cell change== | ==Columnar cell change== | ||
{{Main|Columnar cell change of the breast}} | |||
==Gynecomastoid hyperplasia== | |||
* | *[[AKA]] ''gynecomastia''. | ||
{{Main|Gynecomastoid hyperplasia}} | |||
== | ==Breast prostheses== | ||
{{Main|Breast prostheses}} | |||
= | =Lesions with increased risk of malignancy= | ||
== | ==Florid epithelial hyperplasia== | ||
* | *AKA ''florid epithelial hyperplasia of the usual type'', abbreviated ''FEHUT''. | ||
*AKA ''epithelial hyperplasia'' - term should be avoid as it could lead to confusion with ''[[mild epithelial hyperplasia]]''. | |||
*AKA ''usual ductal hyperplasia'', abbreviated ''UDH''. | |||
{{Main|Florid epithelial hyperplasia}} | |||
==Sclerosing adenosis== | ==Sclerosing adenosis== | ||
{{Main|Sclerosing adenosis of the breast}} | |||
=== | ==Flat epithelial atypia== | ||
*Abbreviated ''FEA''. | |||
{{Main|Flat epithelial atypia}} | |||
* | |||
== | ==Complex sclerosing lesion== | ||
*AKA '' | *[[AKA]] ''radial scar''. | ||
{{Main|Complex sclerosing lesion}} | |||
= | =Stromal lesions= | ||
This section (below) covers stromal lesions of the breast, which vary from benign to malignant. The most common is (the benign) [[fibroadenoma]]. | |||
Non-breast stroma stromal lesions are covered in the ''[[soft tissue lesions]]'' article. [[Angiosarcoma]] (dealt with in the ''[[vascular tumours]]'' article) is the most common (non-breast stroma) sarcoma of the breast, and classically arises after treatment for a breast carcinoma. | |||
==Fibroadenoma== | ==Fibroadenoma== | ||
{{Main|Fibroadenoma}} | |||
== | ==Phyllodes tumour== | ||
* | *Previously ''cystosarcoma phyllodes''. | ||
{{Main|Phyllodes tumour}} | |||
== | ==Pseudoangiomatous stromal hyperplasia== | ||
* | *Abbreviated ''PASH''. | ||
*[[AKA]] ''nodular myofibroblastic stromal hyperplasia of the mammary gland''.<ref name=pmid12199757>{{Cite journal | last1 = Leon | first1 = ME. | last2 = Leon | first2 = MA. | last3 = Ahuja | first3 = J. | last4 = Garcia | first4 = FU. | title = Nodular myofibroblastic stromal hyperplasia of the mammary gland as an accurate name for pseudoangiomatous stromal hyperplasia of the mammary gland. | journal = Breast J | volume = 8 | issue = 5 | pages = 290-3 | month = | year = | doi = | PMID = 12199757 }}</ref> | |||
{{Main|Pseudoangiomatous stromal hyperplasia}} | |||
=Weird stuff= | |||
Like in all niches of pathology... there is weird stuff. | |||
== | ==Mammary hamartoma== | ||
* | *[[AKA]] ''breast hamartoma''. | ||
{{Main|Mammary hamartoma}} | |||
==== | ==Collagenous spherulosis== | ||
*[[AKA]] ''mucinous spherulosis'', [[AKA]] ''spherulosis''.<ref name=stanford_collspher>URL: [http://surgpathcriteria.stanford.edu/breast/collspher/ http://surgpathcriteria.stanford.edu/breast/collspher/]. Accessed on: 4 September 2011.</ref> | |||
* | {{Main|Collagenous spherulosis}} | ||
== | ==Nipple adenoma== | ||
*[[AKA]] ''nipple duct adenoma''. | |||
*[[AKA]] ''nipple adenoma of breast''. | |||
*[[AKA]] ''adenoma of the nipple''. | |||
*[[AKA]] ''florid papillomatosis of the nipple''.<ref name=pmid22342578>{{Cite journal | last1 = Boutayeb | first1 = S. | last2 = Benomar | first2 = S. | last3 = Sbitti | first3 = Y. | last4 = Harroudi | first4 = T. | last5 = Hassam | first5 = B. | last6 = Errihani | first6 = H. | title = Nipple adenoma in a man: An unusual case report. | journal = Int J Surg Case Rep | volume = 3 | issue = 5 | pages = 190-2 | month = | year = 2012 | doi = 10.1016/j.ijscr.2011.05.008 | PMID = 22342578 }}</ref> | |||
{{Main|Nipple adenoma}} | |||
== | ==Intraductal papilloma== | ||
* | *[[AKA]] ''papilloma''. | ||
{{Main|Intraductal papilloma of the breast}} | |||
== | ==Lymphocytic mastitis== | ||
* | *If the individual has [[diabetes mellitus]] it is ''[[diabetic mastopathy]]''. | ||
{{Main|Lymphocytic mastitis}} | |||
=== | ==Microglandular adenosis== | ||
:'''''Not''' to be confused with [[microglandular hyperplasia]]''. | |||
*Abbreviated ''MGA''. | |||
* | {{Main|Microglandular adenosis}} | ||
== | ==Adenomyoepithelioma== | ||
{{Main|Adenomyoepithelioma}} | |||
== | ==Mammary myofibroblastoma== | ||
*[[AKA]] ''breast myofibroblastoma''. | |||
*[[AKA]] ''myofibroblastoma of the breast''. | |||
{{Main|Mammary myofibroblastoma}} | |||
|} | |||
==Squamous metaplasia of lactiferous ducts== | |||
*Abbreviated ''SMOLD''. | |||
{{Main|Squamous metaplasia of lactiferous ducts}} | |||
== | ==Granular cell tumour of the breast== | ||
{{Main|Granular cell tumour}} | |||
===General=== | |||
* | *Uncommon. | ||
===Gross=== | ===Gross=== | ||
*May be a spiculated mass and thus mimic malignancy radiologically.<ref name=pmid16615051>{{Cite journal | last1 = Yang | first1 = WT. | last2 = Edeiken-Monroe | first2 = B. | last3 = Sneige | first3 = N. | last4 = Fornage | first4 = BD. | title = Sonographic and mammographic appearances of granular cell tumors of the breast with pathological correlation. | journal = J Clin Ultrasound | volume = 34 | issue = 4 | pages = 153-60 | month = May | year = 2006 | doi = 10.1002/jcu.20227 | PMID = 16615051 }}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
:See ''[[granular cell tumour]]''. | |||
=== | DDx: | ||
*[[Invasive lobular carcinoma]].<ref name=pmid21398688>{{Cite journal | last1 = Tan | first1 = PH. | last2 = Harada | first2 = O. | last3 = Thike | first3 = AA. | last4 = Tse | first4 = GM. | title = Histiocytoid breast carcinoma: an enigmatic lobular entity. | journal = J Clin Pathol | volume = 64 | issue = 8 | pages = 654-9 | month = Aug | year = 2011 | doi = 10.1136/jcp.2011.088930 | PMID = 21398688 }}</ref> | |||
==Breast | =See also= | ||
*[[Breast cytopathology]]. | |||
*[[Salivary gland]]. | |||
*[[Invasive breast cancer]]. | |||
*[[Non-invasive breast cancer]]. | |||
=References= | |||
{{reflist|2}} | |||
== | =External links= | ||
*[http://www.breastpathology.info/Case_of_the_month/cotm_root.html A collection of breast pathology cases (breastpathology.info)]. | |||
*[http://www.webpathology.com/atlas_map.asp?section=9 Breast pathology (webpathology.com)]. | |||
[[Category:Breast pathology]] | [[Category:Breast pathology]] | ||
Latest revision as of 04:47, 1 July 2016
The breast is an important organ that pathologists see quite often because it is often afflicted by cancer. Before women started smoking in large numbers, it was a leading cause of cancer death in women.
Fortunately, breast cancer, in this day, has a relatively good prognosis if it is detected early.
Clinical
Clinical Presentations of Breast Pathology
- Abnormal/suspicious screening mammogram
- Suspicious microcalcifications and/or suspicious mass.
- Most common history on the specimen requisition
- May be accompanied by a BI-RADS score.
- Nipple discharge.
- Pain.
- Breast lump/mass.
- New nipple inversion.
- Skin changes, e.g. peau d'orange.
Breast cancer screening
Breast cancer screening, for normal risk individuals, starts at age 50 in Canada. In the USA, breast screening starts at age 40.
Radiologic screening is less effective in younger individual as:
- The breast is more dense and thus radiologically more difficult to interpret, and
- The incidence of breast cancer is lower.
Breast radiology
Specimens
Three major specimen types:
- Core needle biopsy (CNB).
- Lumpectomy.
- Modified radical mastectomy.
Note:
- Breast cytopathology is dealt with in the breast cytopathology article. Breast cytology is almost extinct unless you happen to be in Australia where for reasons unknown, the art is still taken seriously. Breast cytology is not sensitive or specific enough to justify forgoing a CNB.
Core needle biopsy
Work-up of CNBs is dependent on the clinical abnormality:[1]
- Mass lesion - usu. obvious what is going on; typically 3 levels.
- Calcifications - abnormality may be very small; typically 10 levels.
Note - if you have a high BI-RADS score on the biopsy requisition, and no correlating histologic findings, be sure to correlate with the specimen radiograph, consider leveling the specimen to exhaustion and/or note the lack of a correlating lesion on your report.
Lumpectomy
Lumpectomies are usually oriented with short and long suture; short is typically superior (aspect) and long is typically lateral (aspect).
Modified radical mastectomy
- Usually done with sentinel lymph node biopsy - as one cannot go back later to do this.
Where to start
The following is a starting point for mentally framing routine breast pathology & some of the challenges in breast pathology:
The key to breast pathology is the myoepithelial cell.
- A benign gland has two cell layers - myoepithelial and epithelial.
- The luminal cell is epithelial
- The basal cells is myoepithelial
Questions to Ask
- Is it normal or close to normal?
- Are you familiar with normal/altered but benign/physiologic changes in the breast?
- Do the changes observed explain the biopsy (are you sure you are seeing the radiographic lesion)?
- Have you found the microcalcifications?
- Is it a neoplastic but benign?
- Are you familiar with the common benign breast neoplasms?
- Do you know the morphologic criteria for a benign breast gland?
- Do you know how to use IHC to confirm a benign process?
- Is it an in situ carcinoma?
- Are you familiar with DCIS and LCIS and their variants?
- Do you know the morphologic criteria for in situ carcinoma?
- Do you know how to use ICH to confirm an in situ carcinoma?
- Do you know how to report an in situ breast carcinoma?
- Is it invasive carcinoma?
- Do you know the morphologic criteria for an invasive gland?
- Do you know how to use IHC to confirm invasion?
- Do you know the morphologic features of typical invasive breast carcinoma?
- Do you know the subtypes?
- Do you understand the implications of some of the medullary/medullary-like subtype (especially in a young patient)?
- Do you know how to use IHC for prognostication?
- Do you understand the implications of triple negativity?
- Do you know how to report an invasive breast carcinoma?
- Is it something stromal/spindled?
Important Differential Diagnoses
Papillary Lesions
- Nipple adenoma.
- Intraductal papilloma.
- Papillary ductal carcinoma in situ.
- Intracystic papillary carcinoma.
- Intracystic papillary carcinoma with an invasive component.
- Invasive papillary carcinoma.
Basaloid Lesions
- Adenoid cystic carcinoma of the breast.
- Intracystic papillary breast carcinoma, solid variant.
- Invasive papillary breast carcinoma, solid variant.
- Medullary breast carcinoma.
- Medullary-like breast carcinoma.
- Know when to start a discussion about BRCA mutations, triple negativity and the 'basal-like molecular phenotype'.
Spindle Cell Lesions
- Metaplastic breast carcinoma.
- Treated breast carcinoma.
- Mammary myofibroblastoma.
- Phyllodes Tumour - stromal component.
- Desmoid fibromatosis.
- Nodular fasciitis.
Additional resources
- Breast Pathology Info [1]
- Digital Atlas of Breast Pathology [2]
- Pathology Outlines - Breast Nonmalignant [3]
- Pathology Outlines - Breast Malignant [4]
- WebPathology - Breast [5]
Normal breast
Resting breast
- Glands -- normally has two cell layers (like the prostate).
- Myoepithelial cells
- Frequently spindle-like, often hard to see.
- Secretory cells.
- Myoepithelial cells
- Stroma:
- Not cellular.
- Not myxoid.
May be present:
- Calcification:
- Purple globs (with concentric rings) on H&E = calcium phosphate.
- Q. How to remember? A. Purple = Phosphate.
- Calcium oxalate visible with (light) polarization - not associated with malignancy.
- Often in the lumen of a gland, may be in the stroma.
- Calcific material typically has a well-demarcated border +/- "sharp corners".
- Radiologists can pick-up calcs (calcifications) that are approximately 100 micrometers; if "calcs" is on the requisition one needs to find calcs this size.[2]
- The large calcs seen on radiology are approximately 1/5 - 1/6 the size of a HPF, if the field of view (FOV) is ~0.55 mm (as is the case with 22 mm-10x eye pieces and a 40x objective).
- Purple globs (with concentric rings) on H&E = calcium phosphate.
Notes:
- The architecture is more important than the cytologic features in the diagnosis of malignancy in the breast;[3] low grade tumours have distorted architecture but normal/near normal cytology.
Image
Lactational changes
General
- Lactational adenoma generally arises in during or in the few weeks after pregnancy.
- May be present focally in non-pregnant females.
- "Lactational adenoma"- circumscribed mass displacing the normal breast architecture (hyperplasia plus functional/physiologic change)
- "Lactational change"- normal breast tissue architecture preserved (functional/physiologic change).
ASIDE:
- Some believe lactational change and secretory change aren't the same...
- Lactational change = only in lactation.
- Secretory change = other times.
- This hair splitting is clinically irrelevant-- both are benign. Also, experts use the terms interchangeably.[5]
Microscopic
Features:[6]
- Glands dilated.
- Increased number of lobules.
- Relative decrease in intralobular and extralobular stroma.
- Luminal cells enlarged.
- Vacuolated cytoplasm.
- Hobnail morphology - hang into the lumen.
- Myoepithelial cells indistinct - after second trimester.
- Lactational "adenoma" may undergo infarction - Imagine what an infarcted lactational adenoma could look like in a FNA specimen!
DDx:
Images
www:
- Lactational changes (gfmer.ch).
- Lactational changes in an angiosarcoma of the breast (webpathology.com).
- Lactating breast (uwa.edu.au).
Major Pathologic Patterns
General classification
| Breast pathology | |||||||||||||||||||||||||||||||||||||||||||||||||
| Stromal pathology | Miscellaneous | Glandular pathology | |||||||||||||||||||||||||||||||||||||||||||||||
| Myxoid | Long slit-like spaces | Simple epithelium | Dilated | Cellular lesions | |||||||||||||||||||||||||||||||||||||||||||||
| Fibroadenoma | Malignant features | Benign features | Tubular carcinoma | FEA, FCC, CCC | FEHUT, Neoplastic, Malignant | ||||||||||||||||||||||||||||||||||||||||||||
| Malignant phyllodes | Benign phyllodes | ||||||||||||||||||||||||||||||||||||||||||||||||
Notes:
- The challenges in breast pathology are in: the Simple epithelium category and the Cellular lesions category.
- Neoplastic includes: ADH and LDH.
- Malignant includes: DCIS, LCIS, ductal carcinoma (DC) and lobular carcinoma (LC), some papillary lesions.
- Lobular carcinoma (a pitfall) may appear to be a stromal problem, i.e. the stroma looks too cellular.
- Miscellaneous includes rare tumours of the breast that do not fit into another category, i.e. metastases, lymphomas, melanoma, sarcomas. Skin-related pathology is dealt within the dermatologic neoplasms article. Paget disease of the breast, which may be seen in the context of malignant breast lesions, is discussed in its own article.
Cellular lesions
| Cellular lesions (Glandular) | |||||||||||||||||||||||||||||||||||||||||||||||
| Equal spacing, punched-out | Streaming, periph. slit-like spaces. | Discohesive cells, expanded gl. | Single cells or single file | Fibrovascular cores | |||||||||||||||||||||||||||||||||||||||||||
| Ductal lesion | FEHUT | Lobular lesion | Lobular carcinoma | Papillary lesions | |||||||||||||||||||||||||||||||||||||||||||
| Two cell layers | One cell layer | <50% of gl. | >50% of gl. | ||||||||||||||||||||||||||||||||||||||||||||
| Ductal non-inv. neoplasm | Ductal carcinoma | ALH | LCIS | ||||||||||||||||||||||||||||||||||||||||||||
| Large extent | Small extent | ||||||||||||||||||||||||||||||||||||||||||||||
| DCIS | ADH | ||||||||||||||||||||||||||||||||||||||||||||||
Notes:
- The largest challenge is: differentiating between the first two categories on level 2, i.e. equal spacing' vs. streaming.
- The fibrovascular cores must arise from a tuft, i.e. if they are arising directly from the wall of glands only it is likely papillary DCIS.
Papillary lesions
| Papillary lesions | |||||||||||||||||||||||||||||||||||||||
| Myoepithelial cells present | Myoepithelial cells absent | ||||||||||||||||||||||||||||||||||||||
| Unremarkable papillae | Atypia or arch. abnorm. or cellular proliferation | Neoplastic cells present | |||||||||||||||||||||||||||||||||||||
| Benign intraductal papilloma | High grade atypia | Low grade atypia or abnorm. arch. | Only cellular proliferation | Intracystic (encapsulated) papillary ca. | |||||||||||||||||||||||||||||||||||
| DCIS in papilloma | FEHUT in papilloma | ||||||||||||||||||||||||||||||||||||||
| >3 mm extent | <3 mm extent | ||||||||||||||||||||||||||||||||||||||
| DCIS in papilloma | ADH in papilloma | ||||||||||||||||||||||||||||||||||||||
Notes:
- Adapted from Mulligan & O'Malley.[7]
- The most important decision is the first one: myoepithelial cells present vs. absent.
- abnorm. arch. = abnormal architecture present.
- DCIS = ductal carcinoma in situ.
- FEHUT = florid epithelial hyperplasia of the usual type.
- extent refers to the size of the abnormal cell population within the papillary lesion.
Malignant lesions
Non-invasive breast cancer
This includes the in situ lesions - DCIS and LCIS.
Invasive breast cancer
This is includes descriptions of the usual types... and the not so common ones.
Common benign lesions
The breast has lots of benign things. Unlike the prostate, the where benign is called benign, everything has a name. It is more common among breast pathologists to sign-out things like: apocrine metaplasia (benign), columnar cell change (benign), and florid epithelial hyperplasia of the usual type (FEHUT) - instead of - benign breast tissue.
Mild epithelial hyperplasia
General
- No increased risk of malignancy.
- Often not reported - as it has no clinical signficance.
- Has to be separated from moderate epithelial hyperplasia / florid epithelial hyperplasia.
Microscopic
Features:[8]
- Breast glands with three or four cell layers above the basement membrane.
- Variable cells.
Note:
- No nuclear atypia.
DDx:
- Flat epithelial atypia.
- Moderate epithelial hyperplasia / florid epithelial hyperplasia.
- Atypical ductal hyperplasia.
Apocrine metaplasia
Duct ectasia
- Dilation of large ducts secondary to luminal obstruction by inspissated secretions
- Presentation
- ~age 40-50, possibly with cheesy nipple discharge
- Pathology
- Duct lumen dilated and containing foamy macrophages
- Necrosis/shedding of epithelium
- If duct rupture: chronic and granulomatous inflammation of periductal region
- Fibrotic thickening of duct wall
Fibrocystic change
- AKA fibrocystic changes (abbreviated FCC).
Columnar cell change
Gynecomastoid hyperplasia
- AKA gynecomastia.
Breast prostheses
Lesions with increased risk of malignancy
Florid epithelial hyperplasia
- AKA florid epithelial hyperplasia of the usual type, abbreviated FEHUT.
- AKA epithelial hyperplasia - term should be avoid as it could lead to confusion with mild epithelial hyperplasia.
- AKA usual ductal hyperplasia, abbreviated UDH.
Sclerosing adenosis
Flat epithelial atypia
- Abbreviated FEA.
Complex sclerosing lesion
- AKA radial scar.
Stromal lesions
This section (below) covers stromal lesions of the breast, which vary from benign to malignant. The most common is (the benign) fibroadenoma.
Non-breast stroma stromal lesions are covered in the soft tissue lesions article. Angiosarcoma (dealt with in the vascular tumours article) is the most common (non-breast stroma) sarcoma of the breast, and classically arises after treatment for a breast carcinoma.
Fibroadenoma
Phyllodes tumour
- Previously cystosarcoma phyllodes.
Pseudoangiomatous stromal hyperplasia
Weird stuff
Like in all niches of pathology... there is weird stuff.
Mammary hamartoma
- AKA breast hamartoma.
Collagenous spherulosis
Nipple adenoma
- AKA nipple duct adenoma.
- AKA nipple adenoma of breast.
- AKA adenoma of the nipple.
- AKA florid papillomatosis of the nipple.[11]
Intraductal papilloma
- AKA papilloma.
Lymphocytic mastitis
- If the individual has diabetes mellitus it is diabetic mastopathy.
Microglandular adenosis
- Not to be confused with microglandular hyperplasia.
- Abbreviated MGA.
Adenomyoepithelioma
Mammary myofibroblastoma
Squamous metaplasia of lactiferous ducts
- Abbreviated SMOLD.
Granular cell tumour of the breast
General
- Uncommon.
Gross
- May be a spiculated mass and thus mimic malignancy radiologically.[12]
Microscopic
- See granular cell tumour.
DDx:
See also
References
- ↑ MUA. 1 October 2010.
- ↑ MUA. 1 October 2010.
- ↑ RS. 4 May 2010.
- ↑ URL: [Breast_pathology#Lactational_changes Breast_pathology#Lactational_changes. Accessed on: 3 October 2011.
- ↑ Tavassoli, FA.; Yeh, IT. (Jan 1987). "Lactational and clear cell changes of the breast in nonlactating, nonpregnant women.". Am J Clin Pathol 87 (1): 23-9. PMID 2879437.
- ↑ URL: http://flylib.com/books/en/2.953.1.9/1/. Accessed on: 6 August 2011.
- ↑ Mulligan AM, O'Malley FP (March 2007). "Papillary lesions of the breast: a review". Adv Anat Pathol 14 (2): 108–19. doi:10.1097/PAP.0b013e318032508d. PMID 17471117.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 159-160. ISBN 978-0443066801.
- ↑ Leon, ME.; Leon, MA.; Ahuja, J.; Garcia, FU.. "Nodular myofibroblastic stromal hyperplasia of the mammary gland as an accurate name for pseudoangiomatous stromal hyperplasia of the mammary gland.". Breast J 8 (5): 290-3. PMID 12199757.
- ↑ URL: http://surgpathcriteria.stanford.edu/breast/collspher/. Accessed on: 4 September 2011.
- ↑ Boutayeb, S.; Benomar, S.; Sbitti, Y.; Harroudi, T.; Hassam, B.; Errihani, H. (2012). "Nipple adenoma in a man: An unusual case report.". Int J Surg Case Rep 3 (5): 190-2. doi:10.1016/j.ijscr.2011.05.008. PMID 22342578.
- ↑ Yang, WT.; Edeiken-Monroe, B.; Sneige, N.; Fornage, BD. (May 2006). "Sonographic and mammographic appearances of granular cell tumors of the breast with pathological correlation.". J Clin Ultrasound 34 (4): 153-60. doi:10.1002/jcu.20227. PMID 16615051.
- ↑ Tan, PH.; Harada, O.; Thike, AA.; Tse, GM. (Aug 2011). "Histiocytoid breast carcinoma: an enigmatic lobular entity.". J Clin Pathol 64 (8): 654-9. doi:10.1136/jcp.2011.088930. PMID 21398688.