Difference between revisions of "Autosomal dominant polycystic kidney disease"
Jump to navigation
Jump to search
| (10 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Polycystic kidney disease -- very low mag.jpg | ||
| Width = | | Width = | ||
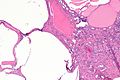
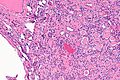
| Caption = | | Caption = Micrograph showing polycystic kidney disease in the context of autosomal dominant polycystic kidney disease. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = cortical cysts lined by simple flattened epithelium, normal renal tubules interspersed between cysts or tubules as seen in [[end-stage kidney]] (thyroidization), +/-fibrosis (late-stage), +/-calcifications | | Micro = cortical cysts lined by simple flattened epithelium, normal renal tubules interspersed between cysts or tubules as seen in [[end-stage kidney]] (thyroidization), +/-fibrosis (late-stage), +/-calcifications | ||
| Line 13: | Line 13: | ||
| Molecular = mutation in PKD1 gene or PKD2 gene | | Molecular = mutation in PKD1 gene or PKD2 gene | ||
| IF = | | IF = | ||
| Gross = enlarged kidney | | Gross = enlarged kidney with "too many cysts to count" | ||
| Grossing = | | Grossing = | ||
| Staging = | | Staging = | ||
| Line 36: | Line 36: | ||
==General== | ==General== | ||
*Incidence of renal cell carcinoma (RCC) is increased in ADPKD in relation to the general population; however, the increase may to be due to the higher incidence of RCC in patients with (advanced) chronic kidney disease rather than ADPKD.<ref name=pmid19446940>{{Cite journal | last1 = Nishimura | first1 = H. | last2 = Ubara | first2 = Y. | last3 = Nakamura | first3 = M. | last4 = Nakanishi | first4 = S. | last5 = Sawa | first5 = N. | last6 = Hoshino | first6 = J. | last7 = Suwabe | first7 = T. | last8 = Takemoto | first8 = F. | last9 = Nakagawa | first9 = M. | title = Renal cell carcinoma in autosomal dominant polycystic kidney disease. | journal = Am J Kidney Dis | volume = 54 | issue = 1 | pages = 165-8 | month = Jul | year = 2009 | doi = 10.1053/j.ajkd.2009.01.270 | PMID = 19446940 }}</ref> | |||
**In a series of 510 patients evaluated clinically, 10 were found to have renal cell carcinoma. Eight of the ten were seen on imaging and two were detected by pathology.<ref name=pmid19446940>{{Cite journal | last1 = Nishimura | first1 = H. | last2 = Ubara | first2 = Y. | last3 = Nakamura | first3 = M. | last4 = Nakanishi | first4 = S. | last5 = Sawa | first5 = N. | last6 = Hoshino | first6 = J. | last7 = Suwabe | first7 = T. | last8 = Takemoto | first8 = F. | last9 = Nakagawa | first9 = M. | title = Renal cell carcinoma in autosomal dominant polycystic kidney disease. | journal = Am J Kidney Dis | volume = 54 | issue = 1 | pages = 165-8 | month = Jul | year = 2009 | doi = 10.1053/j.ajkd.2009.01.270 | PMID = 19446940 }}</ref> | |||
*In a series 301 renal surgeries on 240 ADPKD patients, 16 malignant lesions were seen.<ref name=pmid23752029>{{Cite journal | last1 = Jilg | first1 = CA. | last2 = Drendel | first2 = V. | last3 = Bacher | first3 = J. | last4 = Pisarski | first4 = P. | last5 = Neeff | first5 = H. | last6 = Drognitz | first6 = O. | last7 = Schwardt | first7 = M. | last8 = Gläsker | first8 = S. | last9 = Malinoc | first9 = A. | title = Autosomal dominant polycystic kidney disease: prevalence of renal neoplasias in surgical kidney specimens. | journal = Nephron Clin Pract | volume = 123 | issue = 1-2 | pages = 13-21 | month = | year = 2013 | doi = 10.1159/000351049 | PMID = 23752029 }}</ref> | |||
**10 [[papillary RCC]]s. | |||
**5 [[clear cell RCC]]s. | |||
**1 urothelial carcinoma. | |||
===Etiology=== | ===Etiology=== | ||
*Mutation in ''PKD1'' gene or ''PKD2'' gene. | *Mutation in ''PKD1'' gene or ''PKD2'' gene. | ||
| Line 90: | Line 97: | ||
**Morphologically similar to acquired renal cystic disease.<ref name=rj_oct2010>RJ. 20 October 2010.</ref> | **Morphologically similar to acquired renal cystic disease.<ref name=rj_oct2010>RJ. 20 October 2010.</ref> | ||
**It is said that "... if you can count 'em it's simple cysts; if you can't it's polycystic (renal disease)."<ref name=rj_oct2010>RJ. 20 October 2010.</ref><ref>{{cite book |author= Barbaric, Zoran L. |title=[http://books.google.com/books?id=uABgezxjhYwC&pg=PA87&lpg=PA87&dq=cystic+renal+disease,+%22if+you+can+count+them%22&source=bl&ots=GYyIdR9YmS&sig=DBYzT8LO2MltLA-wwW-0QwnQ6Lk&hl=en&ei=0hF-Taz0IsG3twe5yfG6BQ&sa=X&oi=book_result&ct=result&resnum=1&ved=0CBoQ6AEwAA#v=onepage&q=cystic%20renal%20disease%2C%20%22if%20you%20can%20count%20them%22&f=false Principles of Genitourinary Radiology] |publisher=Thieme |location= |year=1994 |pages= 87 |edition=2nd |isbn=978-0865774933 |oclc= |doi= |accessdate=}}</ref> | **It is said that "... if you can count 'em it's simple cysts; if you can't it's polycystic (renal disease)."<ref name=rj_oct2010>RJ. 20 October 2010.</ref><ref>{{cite book |author= Barbaric, Zoran L. |title=[http://books.google.com/books?id=uABgezxjhYwC&pg=PA87&lpg=PA87&dq=cystic+renal+disease,+%22if+you+can+count+them%22&source=bl&ots=GYyIdR9YmS&sig=DBYzT8LO2MltLA-wwW-0QwnQ6Lk&hl=en&ei=0hF-Taz0IsG3twe5yfG6BQ&sa=X&oi=book_result&ct=result&resnum=1&ved=0CBoQ6AEwAA#v=onepage&q=cystic%20renal%20disease%2C%20%22if%20you%20can%20count%20them%22&f=false Principles of Genitourinary Radiology] |publisher=Thieme |location= |year=1994 |pages= 87 |edition=2nd |isbn=978-0865774933 |oclc= |doi= |accessdate=}}</ref> | ||
===Images=== | |||
<gallery> | |||
Image: Polycystic kidney disease -- extremely low mag.jpg | PKD - extremely low mag. (WC) | |||
Image: Polycystic kidney disease -- very low mag.jpg | PKD - very low mag. (WC) | |||
Image: Polycystic kidney disease -- low mag.jpg | PKD - low mag. (WC) | |||
Image: Polycystic kidney disease -- intermed mag.jpg | PKD - intermed. mag. (WC) | |||
</gallery> | |||
==Sign out== | ==Sign out== | ||
<pre> | |||
Kidney, Right, Nephrectomy: | |||
- Polycystic kidney with chronic pyelonephritis and changes of chronic | |||
renal failure, consistent with polycystic kidney disease. | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
===Alternate=== | |||
<pre> | <pre> | ||
Left Kidney, Nephrectomy: | Left Kidney, Nephrectomy: | ||
| Line 98: | Line 121: | ||
- NEGATIVE for malignancy. | - NEGATIVE for malignancy. | ||
</pre> | </pre> | ||
===Micro=== | |||
The sections show kidney with innumerable cysts and focal benign calcifications. Some atypical cysts with papillations are present. These have bland epithelial cells and do not have apparent proliferative activity. No mass lesion is present. No significant atypia is present. | |||
==See also== | ==See also== | ||
Latest revision as of 19:01, 11 September 2016
| Autosomal dominant polycystic kidney disease | |
|---|---|
| Diagnosis in short | |
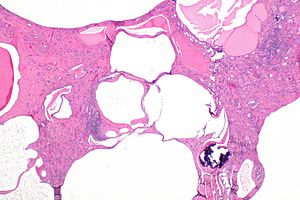 Micrograph showing polycystic kidney disease in the context of autosomal dominant polycystic kidney disease. H&E stain. | |
|
| |
| LM | cortical cysts lined by simple flattened epithelium, normal renal tubules interspersed between cysts or tubules as seen in end-stage kidney (thyroidization), +/-fibrosis (late-stage), +/-calcifications |
| Subtypes | PKD1 gene associated, PKD2 gene associated |
| LM DDx | acquired cystic renal disease |
| Molecular | mutation in PKD1 gene or PKD2 gene |
| Gross | enlarged kidney with "too many cysts to count" |
| Site | kidney - see cystic kidney diseases |
|
| |
| Associated Dx | end-stage kidney, liver cysts; PKD1 associated: cerebral aneurysms; PKD2 associated: colonic diverticula, aortic aneurysm, mitral valve prolapse |
| Clinical history | family member with polycystic kidney disease |
| Prevalence | uncommon |
| Radiology | polycystic kidneys |
| Prognosis | progressive renal failure |
| Treatment | +/-nephrectomy, dialysis, renal transplant |
Autosomal dominant polycystic kidney disease, abbreviated ADPKD, is a common genetic cause of chronic renal failure.
Surgically removed to due to symptoms (mass effect); native nephrectomy often done concurrently with renal transplant.[1]
General
- Incidence of renal cell carcinoma (RCC) is increased in ADPKD in relation to the general population; however, the increase may to be due to the higher incidence of RCC in patients with (advanced) chronic kidney disease rather than ADPKD.[2]
- In a series of 510 patients evaluated clinically, 10 were found to have renal cell carcinoma. Eight of the ten were seen on imaging and two were detected by pathology.[2]
- In a series 301 renal surgeries on 240 ADPKD patients, 16 malignant lesions were seen.[3]
- 10 papillary RCCs.
- 5 clear cell RCCs.
- 1 urothelial carcinoma.
Etiology
- Mutation in PKD1 gene or PKD2 gene.
- Is classified in a large group of diseases - ciliopathies.
PKD1 related disease:[4]
- Encodes polycystin.
- Death at ~53 years.
- Associated with cerebral aneurysms.
PKD2 related disease:[4]
- Death at ~69 years.
- Associated with colonic diverticula, aortic aneurysm, mitral valve prolapse.
Liver cysts and PKD
General
Features:
- Most common extra-renal manifestation of PKD; dependent on age, sex and renal function:[5]
- Age dependence:
- 10-17% <40 years old have liver cysts.
- 70-75% >60 years old have liver cysts.
- Renal function:
- 60-70% of patients with end-stage renal disease (ESRD) and near-ESRD.
- Females more often affected.
- Age dependence:
- Hepatic function usu. preserved.
Complications:[4]
- Infected cyst.
- Cholangiocarcinoma.
Microscopic
Features:
- Von Meyenburg complexes:
- Cluster of dilated ducts with "altered" bile.
- Surrounded by collagenous stroma.
See: Medical liver disease.
Gross
Features:
- Thin walled cysts.
- Number of cysts:
- If you can count 'em it favours acquired renal cystic disease... if you can't it favours the genetic condition.
- Number of cysts:
Microscopic
Features:[6]
- Cortical cysts lined by simple flattened epithelium.
- Normal renal tubules interspersed between cysts or tubules as seen in end-stage kidney (thyroidization).
- +/-Fibrosis (late-stage).
- +/-Calcifications.[citation needed]
DDx:
- Acquired renal cystic disease - rarely.[7]
Images
Sign out
Kidney, Right, Nephrectomy:
- Polycystic kidney with chronic pyelonephritis and changes of chronic
renal failure, consistent with polycystic kidney disease.
- NEGATIVE for malignancy.
Alternate
Left Kidney, Nephrectomy: - Polycystic kidney with changes of chronic renal failure (thyroidization), consistent with polycystic kidney disease. - NEGATIVE for malignancy.
Micro
The sections show kidney with innumerable cysts and focal benign calcifications. Some atypical cysts with papillations are present. These have bland epithelial cells and do not have apparent proliferative activity. No mass lesion is present. No significant atypia is present.
See also
References
- ↑ Veroux, M.; Zerbo, D.; Basile, G.; Gozzo, C.; Sinagra, N.; Giaquinta, A.; Sanfiorenzo, A.; Veroux, P. (2016). "Simultaneous Native Nephrectomy and Kidney Transplantation in Patients With Autosomal Dominant Polycystic Kidney Disease.". PLoS One 11 (6): e0155481. doi:10.1371/journal.pone.0155481. PMID 27257690.
- ↑ 2.0 2.1 Nishimura, H.; Ubara, Y.; Nakamura, M.; Nakanishi, S.; Sawa, N.; Hoshino, J.; Suwabe, T.; Takemoto, F. et al. (Jul 2009). "Renal cell carcinoma in autosomal dominant polycystic kidney disease.". Am J Kidney Dis 54 (1): 165-8. doi:10.1053/j.ajkd.2009.01.270. PMID 19446940.
- ↑ Jilg, CA.; Drendel, V.; Bacher, J.; Pisarski, P.; Neeff, H.; Drognitz, O.; Schwardt, M.; Gläsker, S. et al. (2013). "Autosomal dominant polycystic kidney disease: prevalence of renal neoplasias in surgical kidney specimens.". Nephron Clin Pract 123 (1-2): 13-21. doi:10.1159/000351049. PMID 23752029.
- ↑ 4.0 4.1 4.2 Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 174-5. ISBN 978-0-443-10012-3.
- ↑ Perrone RD (June 1997). "Extrarenal manifestations of ADPKD". Kidney Int. 51 (6): 2022–36. PMID 9186898. http://www.nature.com/ki/journal/v51/n6/pdf/ki1997276a.pdf.
- ↑ Fogo, Agnes B.; Kashgarian, Michael (2005). Diagnostic Atlas of Renal Pathology: A Companion to Brenner and Rector's The Kidney 7E (1st ed.). Saunders. pp. 426. ISBN 978-1416028710.
- ↑ Kessler M, Testevuide P, Aymard B, Huu TC (1991). "Acquired renal cystic disease mimicking adult polycystic kidney disease in a patient undergoing long-term hemodialysis". Am. J. Nephrol. 11 (6): 513–7. PMID 1819219.
- ↑ 8.0 8.1 RJ. 20 October 2010.
- ↑ Barbaric, Zoran L. (1994). Principles of Genitourinary Radiology (2nd ed.). Thieme. pp. 87. ISBN 978-0865774933.