Difference between revisions of "Low-grade papillary urothelial carcinoma"
Jump to navigation
Jump to search
(split-out) |
(+dx) |
||
| Line 121: | Line 121: | ||
[[Category:Urothelium]] | [[Category:Urothelium]] | ||
[[Category:Genitourinary pathology]] | [[Category:Genitourinary pathology]] | ||
[[Category:Diagnosis]] | |||
Revision as of 02:37, 14 November 2013
| Low-grade papillary urothelial carcinoma | |
|---|---|
| Diagnosis in short | |
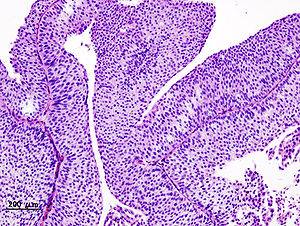 Low-grade papillary urothelial carcinoma. H&E stain. | |
|
| |
| LM | papillae (fibrovascular cores covered by urothelium) -- usually with fusion and branching, small nuclei (~3x a resting lymphocyte), +/-invasion into the lamina propria (rare), +/-mitoses (uncommon) |
| LM DDx | PUNLMP, urothelial papilloma, inverted papilloma, high-grade papillary urothelial carcinoma |
| IHC | Ki-67 low (<25% of cells) |
| Gross | exophytic lesion, frond-like appearance, friable |
| Site | urothelium |
|
| |
| Syndromes | Lynch syndrome |
|
| |
| Signs | hematuria |
| Prevalence | very common |
| Prognosis | very good |
| Clin. DDx | high-grade papillary urothelial carcinoma, urothelial papilloma |
Low-grade papillary urothelial carcinoma, abbreviated LGPUC,[1] is a very common indolent form of cancer that arises from the urothelium.
It is also known as low-grade papillary urothelial cell carcinoma, abbreviated LGPUCC.
General
- Very common.
- Very good prognosis - if it is non-invasive.
- Usually non-invasive.[2]
Note:
- Invasive low-grade UCC is:[2]
- ~75% nested variant of urothelial carcinoma.
- ~25: low-grade papillary urothelial carcinoma.
Gross
- Exophytic lesion.
- Frond-like appearance.
Microscopic
Features:[3]
- Papillae = fibrovascular cores covered by urothelium.
- Usually with fusion of papillae and branching of papillae.
- Small nuclei (~3x a resting lymphocyte).
- +/-Invasion into the lamina propria (rare).
- Rare mitoses.
- Usually difficult to find.
- Basal location.
Criteria for invasion:[2]
- Stromal reaction.
- Infiltrating single cells.
- Small nests.
- Retraction artifact.
- Paradoxical differentiation.
Note:
- Nuclei slightly larger than in PUNLMPs.
- The presence/absence of muscle should be commented on in biopsy specimens.
- Adipose tissue may be seen in the lamina propria; tumour adjacent to adipose tissue on a biopsy does not imply invasion deep to the muscularis propria.[4]
DDx:
- PUNLMP.
- High grade papillary urothelial carcinoma.
- Inverted urothelial papilloma - often have peripheral palisading.
- Urothelial papilloma.
IHC
- Ki-67:
Molecular
Molecular changes:[9]
- FGFR3
- HRAS
- Loss of heterozygosity - chromosome 9.
Note:
- Not currently used diagnostically.
Sign out
URINARY BLADDER LESION ("TUMOUR"), RESECTION:
- LOW-GRADE PAPILLARY UROTHELIAL CARCINOMA.
-- NEGATIVE FOR LAMINA PROPRIA INVASION.
- NO MUSCULARIS PROPRIA IDENTIFIED.
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION OF BLADDER TUMOUR (TURBT):
- LOW-GRADE PAPILLARY UROTHELIAL CARCINOMA.
- NEGATIVE FOR LAMINA PROPRIA INVASION.
- NO MUSCULARIS PROPRIA IDENTIFIED.
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION OF BLADDER TUMOUR (TURBT):
- LOW-GRADE PAPILLARY UROTHELIAL CARCINOMA.
- NEGATIVE FOR LAMINA PROPRIA INVASION.
- MUSCULARIS PROPRIA PRESENT.
See also
References
- ↑ Watts, KE.; Montironi, R.; Mazzucchelli, R.; van der Kwast, T.; Osunkoya, AO.; Stephenson, AJ.; Hansel, DE. (Aug 2012). "Clinicopathologic characteristics of 23 cases of invasive low-grade papillary urothelial carcinoma.". Urology 80 (2): 361-6. doi:10.1016/j.urology.2012.04.010. PMID 22857755.
- ↑ 2.0 2.1 2.2 Toll, AD.; Epstein, JI. (Jul 2012). "Invasive low-grade papillary urothelial carcinoma: a clinicopathologic analysis of 41 cases.". Am J Surg Pathol 36 (7): 1081-6. doi:10.1097/PAS.0b013e318253d6e0. PMID 22510761.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 310. ISBN 978-0781765275.
- ↑ Bochner, BH.; Nichols, PW.; Skinner, DG. (Mar 1995). "Overstaging of transitional cell carcinoma: clinical significance of lamina propria fat within the urinary bladder.". Urology 45 (3): 528-31. doi:10.1016/S0090-4295(99)80030-2. PMID 7879346.
- ↑ Miyamoto, H.; Brimo, F.; Schultz, L.; Ye, H.; Miller, JS.; Fajardo, DA.; Lee, TK.; Epstein, JI. et al. (Aug 2010). "Low-grade papillary urothelial carcinoma of the urinary bladder: a clinicopathologic analysis of a post-World Health Organization/International Society of Urological Pathology classification cohort from a single academic center.". Arch Pathol Lab Med 134 (8): 1160-3. doi:10.1043/2009-0403-OA.1. PMID 20670136.
- ↑ Isfoss, BL.; Majak, B.; Busch, C.; Braathen, GJ. (Apr 2011). "Simplification of grading papillary urothelial neoplasia using a reduced set of diagnostic features.". Anal Quant Cytol Histol 33 (2): 68-74. PMID 21980608.
- ↑ Rajcani, J.; Kajo, K.; Adamkov, M.; Moravekova, E.; Lauko, L.; Felcanova, D.; Bencat, M. (2013). "Immunohistochemical characterization of urothelial carcinoma.". Bratisl Lek Listy 114 (8): 431-8. PMID 23944616.
- ↑ Pich, A.; Chiusa, L.; Comino, A.; Navone, R. (1994). "Cell proliferation indices, morphometry and DNA flow cytometry provide objective criteria for distinguishing low and high grade bladder carcinomas.". Virchows Arch 424 (2): 143-8. PMID 7910097.
- ↑ Ehdaie, B.; Theodorescu, D. (Jan 2008). "Molecular markers in transitional cell carcinoma of the bladder: New insights into mechanisms and prognosis.". Indian J Urol 24 (1): 61-7. doi:10.4103/0970-1591.38606. PMC 2684226. PMID 19468362. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684226/.