Difference between revisions of "Choriocarcinoma"
Jump to navigation
Jump to search
| Line 42: | Line 42: | ||
*Vaginal bleeding or testicular mass. | *Vaginal bleeding or testicular mass. | ||
*Occasionally thyrotoxicosis.<ref name=pmid8395487>{{Cite journal | last1 = O'Reilly | first1 = S. | last2 = Lyons | first2 = DJ. | last3 = Harrison | first3 = M. | last4 = Gaffney | first4 = E. | last5 = Cullen | first5 = M. | last6 = Clancy | first6 = L. | title = Thyrotoxicosis induced by choriocarcinoma a report of two cases. | journal = Ir Med J | volume = 86 | issue = 4 | pages = 124, 127 | month = | year = | doi = | PMID = 8395487 }}</ref> | *Occasionally thyrotoxicosis.<ref name=pmid8395487>{{Cite journal | last1 = O'Reilly | first1 = S. | last2 = Lyons | first2 = DJ. | last3 = Harrison | first3 = M. | last4 = Gaffney | first4 = E. | last5 = Cullen | first5 = M. | last6 = Clancy | first6 = L. | title = Thyrotoxicosis induced by choriocarcinoma a report of two cases. | journal = Ir Med J | volume = 86 | issue = 4 | pages = 124, 127 | month = | year = | doi = | PMID = 8395487 }}</ref> | ||
Note: | |||
*Beta-hCG is negative ~3 weeks after pregnancy.<ref name=pmid2436389 >{{Cite journal | last1 = Haenel | first1 = AF. | last2 = Hugentobler | first2 = W. | last3 = Brunner | first3 = S. | title = [The postpartum course of the HCG titer of maternal blood and its clinical relevance]. | journal = Z Geburtshilfe Perinatol | volume = 190 | issue = 6 | pages = 275-8 | month = | year = | doi = | PMID = 2436389 }}</ref> | |||
===Epidemiology=== | ===Epidemiology=== | ||
Revision as of 20:16, 1 December 2016
| Choriocarcinoma | |
|---|---|
| Diagnosis in short | |
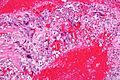
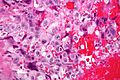
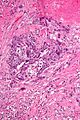
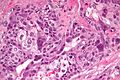
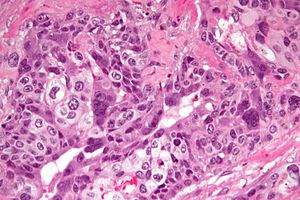 Choriocarcinoma. H&E stain. | |
|
| |
| LM | cytotrophoblasts, syncytiotrophoblast (often wrapped around the cytotrophoblasts) - multinucleated, hemorrhage (very common), necrosis (common) |
| LM DDx | mixed germ cell tumour, invasive hydatidiform mole, placental site trophoblastic tumour |
| IHC | beta-hCG +ve, CD10 +ve, p63 +ve, OCT3 -ve |
| Gross | dark friable, hemorrhagic/necrotic-appearing mass with an invasive border |
| Grossing notes | orchiectomy grossing |
| Staging | testicular cancer staging |
| Site | ovary, testis, uterus |
|
| |
| Associated Dx | complete hydatidiform mole |
| Clinical history | often preceded by pregnancy |
| Signs | testicular mass (male) |
| Symptoms | vaginal bleeding (female) |
| Prevalence | rare |
| Blood work | beta-hCG markedly elevated (usu. >10,000 IU) |
| Prognosis | often poor |
| Treatment | surgery and chemotherapy |
Choriocarcinoma is a rare aggressive germ cell tumour.
General
- Aggressive clinical course.
- Usually a mixed tumour, i.e. pure choriocarcinoma is rare, e.g. dysgerminoma + choriocarcinoma.
Clinical
- High beta-hCG -- usually > 10,000 IU.
- Vaginal bleeding or testicular mass.
- Occasionally thyrotoxicosis.[3]
Note:
- Beta-hCG is negative ~3 weeks after pregnancy.[4]
Epidemiology
- May be preceded by a complete hydatidiform mole.[5]
- More common in the far east.
- More common at extremes of fertile age (teens and 40-50 years).
Gross
- Dark, shaggy, focally hemorrhagic & friable/necrotic-appearing.
- Invasive border.
Microscopic
Features:
- Two cell populations:
- Cytotrophoblasts - key feature.
- Clear cytoplasm.
- Polygonal shaped cells in cords/masses.
- Distinct cell borders.
- Single uniform nucleus.
- Syncytiotrophoblasts - may be absent.[6]
- Large + many irreg. or lobular hyperchromatic nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- +/-Hemorrhage - classically in the centre of the lesion.
- +/-Necrosis.
Notes:
- No chorionic villi should be present.
- If chorionic villi are present... it is likely a type of hydatidiform mole.
- The dual cell population may not be evident at first.
- Hemorrhage and marked nuclear pleomorphism are suggestive of the diagnosis.
DDx:
- Invasive hydatidiform mole.
- Placental site trophoblastic tumour (PSTT).
- Mixed germ cell tumour - esp. for testicular and ovarian tumours.
Images
www:
- Choriocarcinoma - low mag. (webpathology.com).
- Choriocarcinoma (webpathology.com).
- Choriocarcinoma (webpathology.com).
- Choriocarcinoma (chestjournal.chestpubs.org).[7]
- Choriocarcinoma - uterus (med.jhmi.edu).
IHC
ISUP consensus paper by Ulbright et al.:[8]
- Beta-hCG +ve.
- Glypican 3 +ve/-ve.
- OCT3 -ve.
- AFP -ve.
Others:
- p63 +ve.[9]
- Ki-67 +ve -- typically >30%.
- CK7 +ve.[10][11]
- MUC-4 +ve.[12]
- CD10 +ve (10 +ve of 10 cases[13]).
Notes:
- Beta-hCG is classically said to be produced by syncytiotrophoblasts.[14]
See also
References
- ↑ Alvarado-Cabrero, I.; Hernández-Toriz, N.; Paner, GP. (Jan 2014). "Clinicopathologic analysis of choriocarcinoma as a pure or predominant component of germ cell tumor of the testis.". Am J Surg Pathol 38 (1): 111-8. doi:10.1097/PAS.0b013e3182a2926e. PMID 24145647.
- ↑ Mann, K.; Saller, B.; Hoermann, R. (1993). "Clinical use of HCG and hCG beta determinations.". Scand J Clin Lab Invest Suppl 216: 97-104. PMID 7690985.
- ↑ O'Reilly, S.; Lyons, DJ.; Harrison, M.; Gaffney, E.; Cullen, M.; Clancy, L.. "Thyrotoxicosis induced by choriocarcinoma a report of two cases.". Ir Med J 86 (4): 124, 127. PMID 8395487.
- ↑ Haenel, AF.; Hugentobler, W.; Brunner, S.. "[The postpartum course of the HCG titer of maternal blood and its clinical relevance].". Z Geburtshilfe Perinatol 190 (6): 275-8. PMID 2436389.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1110-1111. ISBN 0-7216-0187-1.
- ↑ URL: http://www.webpathology.com/image.asp?n=4&Case=36. Accessed on: 8 February 2011.
- ↑ Venkatram, S.; Muppuri, S.; Niazi, M.; Fuentes, GD. (Jul 2010). "A 24-year-old pregnant patient with diffuse alveolar hemorrhage.". Chest 138 (1): 220-3. doi:10.1378/chest.09-2688. PMID 20605823.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ Mittal, K.; Soslow, R.; McCluggage, WG. (Mar 2008). "Application of immunohistochemistry to gynecologic pathology.". Arch Pathol Lab Med 132 (3): 402-23. doi:10.1043/1543-2165(2008)132[402:AOITGP]2.0.CO;2. PMID 18318583.
- ↑ Park, SY.; Lee, DE.; Park, HJ.; Kim, KC.; Kim, YH. (Nov 2014). "Retroperitoneal nongestational choriocarcinoma in a 25-year-old woman.". Obstet Gynecol Sci 57 (6): 544-8. doi:10.5468/ogs.2014.57.6.544. PMID 25469347.
- ↑ Hemati, S.; Esnaashari, O.; Mohajeri, M.; Sarvizadeh, M. (May 2011). "Choriocarcinoma of the breast; a case report and review of literatures.". J Res Med Sci 16 (5): 707-11. PMID 22091297.
- ↑ Mao, TL.; Kurman, RJ.; Huang, CC.; Lin, MC.; Shih, IeM. (Nov 2007). "Immunohistochemistry of choriocarcinoma: an aid in differential diagnosis and in elucidating pathogenesis.". Am J Surg Pathol 31 (11): 1726-32. doi:10.1097/PAS.0b013e318058a529. PMID 18059230.
- ↑ Kalhor, N.; Ramirez, PT.; Deavers, MT.; Malpica, A.; Silva, EG. (Apr 2009). "Immunohistochemical studies of trophoblastic tumors.". Am J Surg Pathol 33 (4): 633-8. doi:10.1097/PAS.0b013e318191f2eb. PMID 19145204.
- ↑ 14.0 14.1 Cole, LA. (2010). "Biological functions of hCG and hCG-related molecules.". Reprod Biol Endocrinol 8: 102. doi:10.1186/1477-7827-8-102. PMC 2936313. PMID 20735820. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2936313/.
- ↑ Kovalevskaya, G.; Genbacev, O.; Fisher, SJ.; Caceres, E.; O'Connor, JF. (Aug 2002). "Trophoblast origin of hCG isoforms: cytotrophoblasts are the primary source of choriocarcinoma-like hCG.". Mol Cell Endocrinol 194 (1-2): 147-55. PMID 12242037.