Difference between revisions of "Nodular hyperplasia of the prostate gland"
Jump to navigation
Jump to search
| Line 7: | Line 7: | ||
| Micro = stromal and/or glandular hyperplasia | | Micro = stromal and/or glandular hyperplasia | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = | | LMDDx = [[smooth muscle tumour of uncertain malignant potential]], subtle [[prostate carcinoma]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = | ||
| Line 18: | Line 18: | ||
| Assdx = | | Assdx = | ||
| Syndromes = | | Syndromes = | ||
| Clinicalhx = | | Clinicalhx = old man | ||
| Signs = hematuria, weak urine stream, incomplete urinary emptying, post-void dribbling, prolonged voiding, intermittency, hesitancy | | Signs = hematuria, weak urine stream, incomplete urinary emptying, post-void dribbling, prolonged voiding, intermittency, hesitancy | ||
| Symptoms = increased frequency of urination, straining | | Symptoms = increased frequency of urination, straining | ||
| Line 28: | Line 28: | ||
| Other = | | Other = | ||
| ClinDDx = other causes of hematuria ([[urothelial carcinoma]], [[renal cell carcinoma]], cystitis), other causes of obstruction ([[prostate carcinoma]], [[urothelial carcinoma]]) | | ClinDDx = other causes of hematuria ([[urothelial carcinoma]], [[renal cell carcinoma]], cystitis), other causes of obstruction ([[prostate carcinoma]], [[urothelial carcinoma]]) | ||
| Tx = medical, TURP | | Tx = medical, [[TURP]] | ||
}} | }} | ||
'''Nodular hyperplasia of the prostate gland''', also '''benign prostatic hyperplasia''' (abbreviated '''BPH'''), is a common benign pathology of the [[prostate gland]]. | '''Nodular hyperplasia of the prostate gland''', also '''benign prostatic hyperplasia''' (abbreviated '''BPH'''), is a common benign pathology of the [[prostate gland]]. | ||
Revision as of 03:21, 6 August 2015
| Nodular hyperplasia of the prostate gland | |
|---|---|
| Diagnosis in short | |
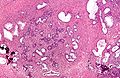
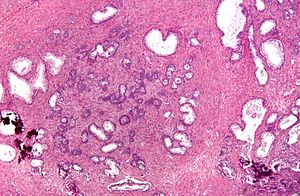 Nodular hyperplasia of the prostate gland. H&E stain. | |
|
| |
| Synonyms | benign prostatic hyperplasia, benign prostatic hypertrophy (misnomer) |
|
| |
| LM | stromal and/or glandular hyperplasia |
| LM DDx | smooth muscle tumour of uncertain malignant potential, subtle prostate carcinoma |
| Gross | enlarged prostate gland, nodularity |
| Grossing notes | prostate chips, radical prostatectomy |
| Site | prostate gland |
|
| |
| Clinical history | old man |
| Signs | hematuria, weak urine stream, incomplete urinary emptying, post-void dribbling, prolonged voiding, intermittency, hesitancy |
| Symptoms | increased frequency of urination, straining |
| Prevalence | very common, esp. elderly |
| Blood work | +/-elevation of PSA (mild) |
| Prognosis | benign |
| Clin. DDx | other causes of hematuria (urothelial carcinoma, renal cell carcinoma, cystitis), other causes of obstruction (prostate carcinoma, urothelial carcinoma) |
| Treatment | medical, TURP |
Nodular hyperplasia of the prostate gland, also benign prostatic hyperplasia (abbreviated BPH), is a common benign pathology of the prostate gland.
It is also known as prostatic nodular hyperplasia. Occasionally, it is referred to as benign prostatic hypertrophy; this is a misnomer. This pathology is not a hypertrophy.
General
- Very common.
- Incidence increases with age.
Clinical - mnemonic I WISH 2p:[1]
- Intermittency.
- Weak stream.
- Incomplete emptying.
- Straining.
- Hesitancy.
- Post-void dribbling.
- Prolonged voiding.
Others:
- Hematuria - common.[2]
Treatment:
- Medications.
- Transurethral resection of the prostate (TURP).
Gross
- Enlargement of the prostate.
- Nodularity of the prostate.
Microscopic
Features:
- Stromal and/or glandular hyperplasia.
- Stromal component has small blood vessels.
Notes:
- Should not be diagnosed on core biopsy!
- One series suggests clinically relevant prostate cancer is seen in ~1.5% of resections for BPH.[3]
DDx:
- Urothelial carcinoma - significant nuclear atypia.
- Prostate carcinoma - especially low-grade.
- Smooth muscle tumour of uncertain malignant potential - lacks small vessels.[4]
Images
Sign out
Urothelium present
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION. - UROTHELIAL MUCOSA WITH A MILD LYMPHOCYTIC INFILTRATE. - NEGATIVE FOR MALIGNANCY.
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP) AND URINARY BLADDER NECK: - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION. - UROTHELIUM WITH THE CHANGES OF CYSTITIS CYSTICA ET GLANDULARIS. - NEGATIVE FOR MALIGNANCY.
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP) AND URINARY BLADDER NECK: - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION, AND FOCAL ACUTE AND CHRONIC INFLAMMATION. - UROTHELIUM WITH THE CHANGES OF CYSTITIS CYSTICA ET GLANDULARIS. - NEGATIVE FOR MALIGNANCY.
Prostate tissue, transurethral resection of prostate: - Benign prostatic tissue - Benign urothelial mucosa with mild inflammation and calcification - Negative for malignancy
No urothelium present
PROSTATE GLAND, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION.
Post-TURP granuloma present
PROSTATE TISSUE, TRANSURETHRAL RESECTION OF THE PROSTATE (TURP): - BENIGN PROSTATIC TISSUE WITH GLANDULAR AND STROMAL PROLIFERATION WITH PROMINENT BLOOD VESSELS AND SQUAMOUS METAPLASIA. - PALISADING GRANULOMA WITH NECROTIC CORE, SEE COMMENT. - UROTHELIAL MUCOSA WITH A MILD INFLAMMATORY INFILTRATE. - NEGATIVE FOR MALIGNANCY. COMMENT: This is morphologically consistent with a post-TURP granuloma.
See also
References
- ↑ Shiau, Carolyn; Toren, Andrew (2006). Toronto Notes 2006: Comprehensive Medical Reference (Review for MCCQE 1 and USMLE Step 2) (22nd edition (2006) ed.). Toronto Notes for Medical Students, Inc.. pp. U5. ISBN 978-0968592861.
- ↑ Sharp, VJ.; Barnes, KT.; Erickson, BA. (Dec 2013). "Assessment of asymptomatic microscopic hematuria in adults.". Am Fam Physician 88 (11): 747-54. PMID 24364522.
- ↑ Skrzypczyk, MA.; Dobruch, J.; Nyk, L.; Szostek, P.; Szempliński, S.; Borówka, A. (2014). "Should all specimens taken during surgical treatment of patients with benign prostatic hyperplasia be assessed by a pathologist?". Cent European J Urol 67 (3): 227-32. doi:10.5173/ceju.2014.03.art2. PMID 25247076.
- ↑ Hansel, DE.; Herawi, M.; Montgomery, E.; Epstein, JI. (Jan 2007). "Spindle cell lesions of the adult prostate.". Mod Pathol 20 (1): 148-58. doi:10.1038/modpathol.3800676. PMID 17170745.