Difference between revisions of "Glycogen storage diseases"
Jump to navigation
Jump to search
(→Cori disease: +image) |
Jensflorian (talk | contribs) (→Pompe disease: +update) |
||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Glycogen storage diseases''' a group of diseases characterized by the accumulation of glycogen. | '''Glycogen storage diseases''' a group of diseases characterized by the accumulation of glycogen. | ||
=Clinical picture= | |||
*Exercise intolerance | |||
*Usually due to specific muscle enzyme defects | |||
DDx: | |||
* Mitochondriopathies | |||
* Carnitine palmitoyltransferase II (CPT2) deficiency | |||
=General microscopic= | =General microscopic= | ||
Features:<ref>URL: [http://neuromuscular.wustl.edu/pathol/acidmchi.htm http://neuromuscular.wustl.edu/pathol/acidmchi.htm]. Accessed on: 11 January 2011.</ref> | Features:<ref>URL: [http://neuromuscular.wustl.edu/pathol/acidmchi.htm http://neuromuscular.wustl.edu/pathol/acidmchi.htm]. Accessed on: 11 January 2011.</ref> | ||
*+/-Vacuolated muscle fibres. | *+/-Vacuolated muscle fibres. | ||
*acid phosphatase+ve in vaculoes. | |||
*PAS+ve. | |||
Images: | Images: | ||
<gallery> | |||
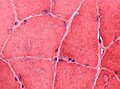
File:HE_glycogen_storage_disease_highmag.jpg | Abnormal glycogen is not easy to spot in this muscle biopsy HE stain (WC/jensflorian) | |||
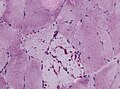
File:PAS_glycogen_storage_disease_intermed_mag.jpg | Intramuscular glycogen is usually PAS+++ve (WC/jensflorian) | |||
Trichrom_glycogen_storage_disease_intermed_mag..jpg | Lack of staining in intramuscular deposits, Trichrom Gömöri (WC/jensflorian) | |||
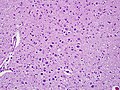
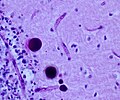
File:Polyglucosan body disease.jpg | Lafora-like polyglucosan bodies in the CNS, low magnification (WC/jensflorian) | |||
File:Adult polyglucosan body disease histopathology.jpg | Lafora-like polyglucosan bodies in the CNS, higher magnification(WC/marvin101) | |||
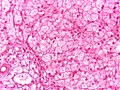
File:Glycogen storage disorder - Liver.jpg | Large vacuoles in the liver, HE stain (WC/Netha Hussain) | |||
</gallery> | |||
*[http://neuromuscular.wustl.edu/pathol/acidmalt.htm Glycogen storage disease (wustl.edu)]. | *[http://neuromuscular.wustl.edu/pathol/acidmalt.htm Glycogen storage disease (wustl.edu)]. | ||
*[http://www.brown.edu/Courses/Digital_Path/systemic_path/hepatobiliary/gsd1.html Glycogen storage disease (brown.edu)]. | *[http://www.brown.edu/Courses/Digital_Path/systemic_path/hepatobiliary/gsd1.html Glycogen storage disease (brown.edu)]. | ||
| Line 14: | Line 32: | ||
=Specific diseases= | =Specific diseases= | ||
==Pompe disease== | ==Pompe disease== | ||
*[[AKA]] | *[[AKA]] glycogen storage disease type II, [[AKA]] acid maltase deficiency, [[AKA]] alpha-1,4-glucosidase deficiency.<ref>URL: [http://www.ncbi.nlm.nih.gov/omim/606800 http://www.ncbi.nlm.nih.gov/omim/606800]. Accessed on: 11 January 2011.</ref> | ||
===General=== | ===General=== | ||
Deficiency of ''alpha-1,4-glucosidase''; it degrades glycogen to glucose in lysosomes. | *Deficiency of ''alpha-1,4-glucosidase''; it degrades glycogen to glucose in lysosomes. | ||
*Autosomal recessive inheritance. | |||
*Identified in 1932 by dutch pathologist Johannes C. Pompe.<ref>Pompe J-C. Over idiopatische hypertropie van het hart. Ned Tijdscr Geneeskd 1932; 76:304.</ref> | |||
* A enzyme replacement therapy exists. <ref>{{Cite journal | last1 = Amalfitano | first1 = A. | last2 = Bengur | first2 = AR. | last3 = Morse | first3 = RP. | last4 = Majure | first4 = JM. | last5 = Case | first5 = LE. | last6 = Veerling | first6 = DL. | last7 = Mackey | first7 = J. | last8 = Kishnani | first8 = P. | last9 = Smith | first9 = W. | title = Recombinant human acid alpha-glucosidase enzyme therapy for infantile glycogen storage disease type II: results of a phase I/II clinical trial. | journal = Genet Med | volume = 3 | issue = 2 | pages = 132-8 | month = | year = | doi = 10.109700125817-200103000-00007 | PMID = 11286229 }} | |||
</ref> | |||
===Clinical=== | |||
*infantile onset (usually at age 4-8months): | |||
**Floppy baby. | |||
**Macroglossia. | |||
**Hepatomegaly. | |||
**Big heart - often early death from cardiac failure. | |||
*late onset (usually at age 1-2years): | |||
**Progressive muscle weakness (myopathy). | |||
**Usually only mild cardiac involvement. | |||
Note: clinical course correlates with remaining enzyme activity.<ref>{{Cite journal | last1 = Hermans | first1 = MM. | last2 = van Leenen | first2 = D. | last3 = Kroos | first3 = MA. | last4 = Beesley | first4 = CE. | last5 = Van Der Ploeg | first5 = AT. | last6 = Sakuraba | first6 = H. | last7 = Wevers | first7 = R. | last8 = Kleijer | first8 = W. | last9 = Michelakakis | first9 = H. | title = Twenty-two novel mutations in the lysosomal alpha-glucosidase gene (GAA) underscore the genotype-phenotype correlation in glycogen storage disease type II. | journal = Hum Mutat | volume = 23 | issue = 1 | pages = 47-56 | month = Jan | year = 2004 | doi = 10.1002/humu.10286 | PMID = 14695532 }}</ref> | |||
===Diagnosis=== | |||
* | * Mutations in acid alpha-glucosidase. | ||
* | * Elevated serum CK (<10x). | ||
** | * Cytoplasmic (lysosomal) vacuoles (Acid phosphatase +ve). | ||
* Muscle fibers with vacuoles enlarged. | |||
* Type 1 fibers more often affected. | |||
* PAS+ve deposits. | |||
* Autophagic (Lysosomal) vacuoles in electron microscopy. | |||
<gallery> | |||
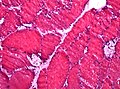
File:Pompe_vacuoles.jpg | Large vacuoles in Pompe disease (H&E, WC/jensflorian) | |||
File:Phenotypical-variation-within-22-families-with-Pompe-disease-1750-1172-8-182-S1.ogv | Clinical phenotype in Pompe disease (WC/Wens et. al.) | |||
</gallery> | |||
==Cori disease== | ==Cori disease== | ||
Latest revision as of 12:24, 17 April 2015
Glycogen storage diseases a group of diseases characterized by the accumulation of glycogen.
Clinical picture
- Exercise intolerance
- Usually due to specific muscle enzyme defects
DDx:
- Mitochondriopathies
- Carnitine palmitoyltransferase II (CPT2) deficiency
General microscopic
Features:[1]
- +/-Vacuolated muscle fibres.
- acid phosphatase+ve in vaculoes.
- PAS+ve.
Images:
Electron microscopy
- Electron dense deposits.
Specific diseases
Pompe disease
- AKA glycogen storage disease type II, AKA acid maltase deficiency, AKA alpha-1,4-glucosidase deficiency.[2]
General
- Deficiency of alpha-1,4-glucosidase; it degrades glycogen to glucose in lysosomes.
- Autosomal recessive inheritance.
- Identified in 1932 by dutch pathologist Johannes C. Pompe.[3]
- A enzyme replacement therapy exists. [4]
Clinical
- infantile onset (usually at age 4-8months):
- Floppy baby.
- Macroglossia.
- Hepatomegaly.
- Big heart - often early death from cardiac failure.
- late onset (usually at age 1-2years):
- Progressive muscle weakness (myopathy).
- Usually only mild cardiac involvement.
Note: clinical course correlates with remaining enzyme activity.[5]
Diagnosis
- Mutations in acid alpha-glucosidase.
- Elevated serum CK (<10x).
- Cytoplasmic (lysosomal) vacuoles (Acid phosphatase +ve).
- Muscle fibers with vacuoles enlarged.
- Type 1 fibers more often affected.
- PAS+ve deposits.
- Autophagic (Lysosomal) vacuoles in electron microscopy.
Cori disease
General
- Hepatomegaly.
Microscopic
Features:
- Hypertrophic hepatocytes with pale cytoplasm.
- Classically: PAS +ve, PAS-D -ve.
- Portal fibrosis.
Image:
Stains
See also
References
- ↑ URL: http://neuromuscular.wustl.edu/pathol/acidmchi.htm. Accessed on: 11 January 2011.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/606800. Accessed on: 11 January 2011.
- ↑ Pompe J-C. Over idiopatische hypertropie van het hart. Ned Tijdscr Geneeskd 1932; 76:304.
- ↑ Amalfitano, A.; Bengur, AR.; Morse, RP.; Majure, JM.; Case, LE.; Veerling, DL.; Mackey, J.; Kishnani, P. et al. "Recombinant human acid alpha-glucosidase enzyme therapy for infantile glycogen storage disease type II: results of a phase I/II clinical trial.". Genet Med 3 (2): 132-8. doi:10.109700125817-200103000-00007. PMID 11286229.
- ↑ Hermans, MM.; van Leenen, D.; Kroos, MA.; Beesley, CE.; Van Der Ploeg, AT.; Sakuraba, H.; Wevers, R.; Kleijer, W. et al. (Jan 2004). "Twenty-two novel mutations in the lysosomal alpha-glucosidase gene (GAA) underscore the genotype-phenotype correlation in glycogen storage disease type II.". Hum Mutat 23 (1): 47-56. doi:10.1002/humu.10286. PMID 14695532.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/232400. Accessed on: 25 January 2011.