Mucinous tumours of the appendix
(Redirected from Appendiceal mucocele)
Jump to navigation
Jump to search
| Mucinous tumours of the appendix | |
|---|---|
| Diagnosis in short | |
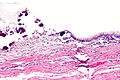
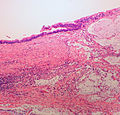
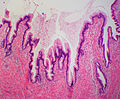
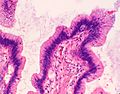
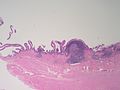
 Mucinous cystadenoma of the appendix. H&E stain. | |
|
| |
| LM | mucin, +/- nuclear atypia |
| Subtypes | see LMDDx |
| LM DDx | mucinous adenocarcinoma, entrapped mucin, mucinous cystadenoma |
| Site | appendix |
|
| |
| Prevalence | uncommon |
| Prognosis | dependent on stage and presence/absence of nuclear atypia |
| Clin. DDx | other appendiceal tumours, metastatic tumours |
| Treatment | right hemicolectomy or appendectomy (?) |
| Mucinous tumours of the appendix | |
|---|---|
| External resources | |
| EHVSC | 10183 |
Mucinous tumours of the appendix are uncommon tumours of the vermiform appendix that can have a benign or malignant behaviour.
Benign appendiceal mucocele and appendiceal mucocele redirect here.
General
- There are many classifications and they are controversial.[1]
- The controversy centres on whether to call all mucinous tumours outside of the appendix adenocarcinoma - regardless of whether they have atypia & show invasion.
- Many potential pathways for extra-appendiceal spread and peritoneal mucin deposition (pseudomyxoma peritonei)
- A mucinous neoplasm ruptures the appendix due to expansion by excessive mucin
- Could occur with either a benign or malignant neoplasm.
- Malignant mucinous glands infiltrate through the appendiceal wall or enter the lymphatics and spread throughout the peritoneum.
- Would require a malignant neoplasm.
- A mucinous neoplasm ruptures the appendix due to expansion by excessive mucin
- Panarelli and Yantiss created a nice summary table - that compares the classifications - see: comparison of classifications (archivesofpathology.org).[1]
- In women - an ovarian primary must be excluded.
- Concurrent bilateral ovarian tumours suggests the tumour originated from the appendix and spread to the ovaries.
- The 2003 classification by Misdraji et al.[2] is a good starting point if one is unfamilar with the topic, as it is the least complicated.
Misdraji classification of 2003
- Benign - low grade mucinous tumour.
- Borderline - mucinous tumour of uncertain malignant potential or borderline mucinous tumour.
- Malignant - mucinous adenocarcinoma.
Five year survival (in a series of 107 cases) as per Misdraji classification:[2]
| Tumour | Five year survival |
|---|---|
| LAMN | 100% |
| LAMN extra-appendiceal spread | 86% |
| MACA | 44% |
- LAMN = low-grade appendiceal mucinous neoplasm.
- LAMN extra-appendiceal = low-grade appendiceal mucinous neoplasm with extra-appendiceal spread.
- MACA = mucinous adenocarcinoma of the appendix.
World Health Organization classification
WHO classification:
- Adenoma with low-grade dysplasia.
- Adenoma with high-grade dysplasia.
- Low-grade invasive mucinous adenocarcinoma
- Confined to the appendiceal wall.
- Outside of the appendix.
- High-grade invasive mucinous adenocarcinoma.
Comparison between Misdraji and WHO classification
Adapted from Panarelli and Yantiss:[1]
| Stage | Cytologic dysplasia | Misdraji | World Health Organization |
|---|---|---|---|
| Confined to the mucosa | low-grade | low-grade appendiceal mucinous neoplasm (LAMN) | mucinous adenoma, negative for high-grade dysplasia |
| Confined to the mucosa | high-grade | non-invasive mucinous cystadenocarcinoma of the appendix | mucinous adenoma with high-grade dysplasia |
| At least into the submucosa, confined to the appendix | low-grade | low-grade appendiceal mucinous neoplasm (LAMN) | invasive mucinous adenocarcinoma, low-grade |
| At least into the submucosa, confined to the appendix | high-grade | mucinous adenocarcinoma of the appendix (MACA) | invasive mucinous adenocarcinoma, high-grade |
| Extra-appendiceal spread | low-grade | low-grade appendiceal mucinous neoplasm (LAMN) | invasive mucinous adenocarcinoma, low-grade |
| Extra-appendiceal spread | high-grade | mucinous adenocarcinoma of the appendix (MACA) | invasive mucinous adenocarcinoma, high-grade |
Microscopic
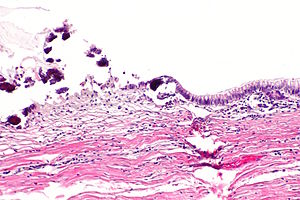
Low-grade appendiceal mucinous neoplasm
- AKA benign mucinous tumour of the appendix.
Microscopic:
- Single layer of epithelium with tufts.
- Vaguely resemble serrations, i.e. the saw-tooth pattern in hyperplastic polyps of the colon.
- Mucin contained (inside appendix only).
- mucin extravasation into the appendiceal wall does not upgrade the tumour.
- No marked nuclear atypia.
Note:
- May be deceptively bland appearing from a cytologic perspective.
Images
www:
- LAMN - low mag. (nature.com).[3]
- LAMN - high mag. (nature.com).[3]
- Appendiceal mucocele (pathlabmed.typepad.com).
Low-grade appendiceal mucinous neoplasm with extra-appendiceal spread
- AKA mucinous borderline tumour of the appendix.
Microscopic:
- Same as LAMN but mucin outside of the appendix.
- Cells in mucin, i.e. cellular mucin.
Mucinous adenocarcinoma of the appendix
- AKA malignant mucinous tumour of the appendix.
Microscopic:
- Marked nuclear pleomorphism.
- Invasion into the appendiceal wall.
Sign out
LAMN
VERMIFORM APPENDIX, APPENDECTOMY: - LOW-GRADE APPENDICEAL MUCINOUS NEOPLASM. -- NEGATIVE FOR EXTRA-APPENDICEAL MUCIN. -- MARGINS NEGATIVE FOR MUCINOUS NEOPLASM. - ACUTE APPENDICITIS. - ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX AND CECUM, APPENDECTOMY WITH CECAL CUFF: - LOW-GRADE APPENDICEAL MUCINOUS NEOPLASM (MUCINOUS CYSTADENOMA). - MARGINS NEGATIVE FOR MUCINOUS NEOPLASM. COMMENT: No extra-appendiceal mucin is identified. There is no invasion into the appendiceal wall.
WHO
APPENDIX, APPENDECTOMY: - APPENDICEAL MUCINOUS CYSTADENOMA WITH EXTENSIVE CALCIFICATION. -- NEGATIVE FOR HIGH-GRADE DYSPLASIA. - NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ 1.0 1.1 1.2 Panarelli, NC.; Yantiss, RK. (Oct 2011). "Mucinous neoplasms of the appendix and peritoneum.". Arch Pathol Lab Med 135 (10): 1261-8. doi:10.5858/arpa.2011-0034-RA. PMID 21970481.
- ↑ 2.0 2.1 Misdraji J, Yantiss RK, Graeme-Cook FM, Balis UJ, Young RH (August 2003). "Appendiceal mucinous neoplasms: a clinicopathologic analysis of 107 cases". Am. J. Surg. Pathol. 27 (8): 1089–103. PMID 12883241. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0147-5185&volume=27&issue=8&spage=1089.
- ↑ 3.0 3.1 Misdraji, J.; Burgart, LJ.; Lauwers, GY. (Dec 2004). "Defective mismatch repair in the pathogenesis of low-grade appendiceal mucinous neoplasms and adenocarcinomas.". Mod Pathol 17 (12): 1447-54. doi:10.1038/modpathol.3800212. PMID 15354187.