Difference between revisions of "Thyroid gland"
(→Anaplastic thyroid carcinoma: split out) |
|||
| (18 intermediate revisions by the same user not shown) | |||
| Line 62: | Line 62: | ||
*[[Follicular thyroid carcinoma|Follicular carinoma]]. | *[[Follicular thyroid carcinoma|Follicular carinoma]]. | ||
*[[Medullary thyroid carcinoma|Medullary carcinoma]]. | *[[Medullary thyroid carcinoma|Medullary carcinoma]]. | ||
*Undifferentiated (anaplastic) carcinoma. | *[[Anaplastic thyroid carcinoma|Undifferentiated (anaplastic) carcinoma]]. | ||
*Poorly differentiated carcinoma. | *[[Poorly differentiated thyroid carcinoma|Poorly differentiated carcinoma]]. | ||
*[[Squamous cell carcinoma]]. | *[[Squamous cell carcinoma]]. | ||
*[[Mucoepidermoid carcinoma]]. | *[[Mucoepidermoid carcinoma]]. | ||
| Line 127: | Line 127: | ||
*p63 +ve. | *p63 +ve. | ||
**-ve in clear cells. | **-ve in clear cells. | ||
*CEA +ve (polyconal).<ref name=pmid7509563>{{cite journal |author=Mizukami Y, Nonomura A, Michigishi T, ''et al.'' |title=Solid cell nests of the thyroid. A histologic and immunohistochemical study |journal=Am. J. Clin. Pathol. |volume=101 |issue=2 |pages=186–91 |year=1994 |month=February |pmid=7509563 |doi= |url=}}</ref> | *[[CEA]] +ve (polyconal).<ref name=pmid7509563>{{cite journal |author=Mizukami Y, Nonomura A, Michigishi T, ''et al.'' |title=Solid cell nests of the thyroid. A histologic and immunohistochemical study |journal=Am. J. Clin. Pathol. |volume=101 |issue=2 |pages=186–91 |year=1994 |month=February |pmid=7509563 |doi= |url=}}</ref> | ||
**+ve also in clear cells. | **+ve also in clear cells. | ||
*Chromogranin A +ve ~45% of cases.<ref name=pmid7509563/> | *Chromogranin A +ve ~45% of cases.<ref name=pmid7509563/> | ||
| Line 137: | Line 137: | ||
*[[AKA]] ''[[nodular hyperplasia]]''. | *[[AKA]] ''[[nodular hyperplasia]]''. | ||
*[[AKA]] ''adenomatoid nodule''. | *[[AKA]] ''adenomatoid nodule''. | ||
{{Main|Thyroid gland nodular hyperplasia}} | |||
==Follicular thyroid adenoma== | ==Follicular thyroid adenoma== | ||
*[[AKA]] follicular adenoma, [[AKA]] thyroid follicular adenoma. | *[[AKA]] follicular adenoma, [[AKA]] thyroid follicular adenoma. | ||
{{Main|Follicular thyroid adenoma}} | |||
==Graves disease== | ==Graves disease== | ||
{{Main|Graves' disease}} | |||
==Idiopathic granulomatous thyroiditis== | ==Idiopathic granulomatous thyroiditis== | ||
| Line 331: | Line 207: | ||
==Riedel thyroiditis== | ==Riedel thyroiditis== | ||
*[[AKA]] ''invasive fibrous thyroiditis''.<ref name=pmid21568724>{{Cite journal | last1 = Fatourechi | first1 = MM. | last2 = Hay | first2 = ID. | last3 = McIver | first3 = B. | last4 = Sebo | first4 = TJ. | last5 = Fatourechi | first5 = V. | title = Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008. | journal = Thyroid | volume = 21 | issue = 7 | pages = 765-72 | month = Jul | year = 2011 | doi = 10.1089/thy.2010.0453 | PMID = 21568724 }}</ref> | *[[AKA]] ''invasive fibrous thyroiditis''.<ref name=pmid21568724>{{Cite journal | last1 = Fatourechi | first1 = MM. | last2 = Hay | first2 = ID. | last3 = McIver | first3 = B. | last4 = Sebo | first4 = TJ. | last5 = Fatourechi | first5 = V. | title = Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008. | journal = Thyroid | volume = 21 | issue = 7 | pages = 765-72 | month = Jul | year = 2011 | doi = 10.1089/thy.2010.0453 | PMID = 21568724 }}</ref> | ||
{{Main|Riedel thyroiditis}} | |||
==Hashimoto thyroiditis== | ==Hashimoto thyroiditis== | ||
{{Main|Hashimoto's thyroiditis}} | |||
==C-cell hyperplasia== | ==C-cell hyperplasia== | ||
*Abbreviated ''CCH''. | *Abbreviated ''CCH''. | ||
{{Main|C-cell hyperplasia}} | |||
==Adenolipoma of the thyroid== | |||
{{Main|Adenolipoma of the thyroid}} | |||
=Malignant neoplasm= | =Malignant neoplasm= | ||
| Line 437: | Line 231: | ||
==Follicular thyroid carcinoma== | ==Follicular thyroid carcinoma== | ||
*[[AKA]] ''follicular carcinoma''. | *[[AKA]] ''follicular carcinoma''. | ||
{{Main|Follicular thyroid carcinoma}} | |||
==Medullary thyroid carcinoma== | ==Medullary thyroid carcinoma== | ||
| Line 495: | Line 260: | ||
*[[AKA]] ''hyalinizing trabecular adenoma''. | *[[AKA]] ''hyalinizing trabecular adenoma''. | ||
*Abbreviated ''HTT''. | *Abbreviated ''HTT''. | ||
{{Main|Hyalinizing trabecular tumour}} | |||
==Hürthle cell neoplasm== | ==Hürthle cell neoplasm== | ||
*[[AKA]] ''oncocytic neoplasm''. | *[[AKA]] ''oncocytic neoplasm''. | ||
*Also spelled ''Hurthle cell neoplasm''. | *Also spelled ''Hurthle cell neoplasm''. | ||
{{Main|Hürthle cell neoplasm}} | |||
==Minocycline associated thyroid pigmentation== | ==Minocycline associated thyroid pigmentation== | ||
| Line 605: | Line 297: | ||
===Stains=== | ===Stains=== | ||
*[[Fontana-Masson stain]] +ve.<ref name=pmid10615019>{{Cite journal | last1 = Sant'Ambrogio | first1 = S. | last2 = Connelly | first2 = J. | last3 = DiMaio | first3 = D. | title = Minocycline pigmentation of heart valves. | journal = Cardiovasc Pathol | volume = 8 | issue = 6 | pages = 329-32 | month = | year = | doi = | PMID = 10615019 }}</ref> | *[[Fontana-Masson stain]] +ve.<ref name=pmid10615019>{{Cite journal | last1 = Sant'Ambrogio | first1 = S. | last2 = Connelly | first2 = J. | last3 = DiMaio | first3 = D. | title = Minocycline pigmentation of heart valves. | journal = Cardiovasc Pathol | volume = 8 | issue = 6 | pages = 329-32 | month = | year = | doi = | PMID = 10615019 }}</ref> | ||
==Sclerosing mucoepidermoid carcinoma with eosinophilia== | |||
{{Main|Sclerosing mucoepidermoid carcinoma with eosinophilia}} | |||
=See also= | =See also= | ||
Latest revision as of 03:43, 20 March 2018
The thyroid gland is an important little endocrine organ in the anterior neck. It is frequently afflicted by cancer... but the common cancer has such a good prognosis there is debate about how aggressively it should be treated. The cytopathology of the thyroid gland is dealt with in the thyroid cytology article.
The gland frustrates a significant number of pathologists, as the criteria for cancer are considered a bit wishy-washy.
Thyroid specimens
They come in three common varieties
- FNA (fine needle aspiration).
- Done to triage patients/rule-out malignancy - discussed in the article thyroid cytopathology.
- Hemithyroid.
- Done to get a definitive diagnosis.
- May be a "completion" - removal of the other half following definitive diagnosis.
- Total thyroid.
- Done for malignancy or follicular lesion.
Gross pathology
- White nodules - think:
- Lymphoid tissue.
- Papillary thyroid carcinoma - may be calcified.[1]
Diagnoses
Common
- Nodular hyperplasia -- most common.
- Lymphocytic thyroiditis.
- Papillary thyroid carcinoma (PTC) -- most common cancer.
- Parathyroid tissue.
Pitfalls/weird stuff
- Thyroid tissue lateral to the jugular vein (often referred to as lateral aberrant thyroid tissue) is generally considered metastatic thyroid carcinoma (papillary thyroid carcinoma) even if it looks benign.[2]
- This dictum is disputed.[3]
- The level VI and VII lymph nodes are medial to the jugular.
- Hashimoto's disease may have so many lymphocytes that it mimics a lymph node -- may lead to misdiagnosis of PTC.
- Parasitic nodule: clump of thyroid that is attached by a thin thread... but looks like a separate nodule; may lead to misdiagnosis of PTC.
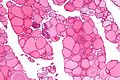
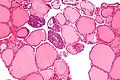
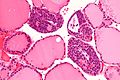
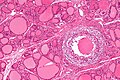
Image:
Diagnostic keys
The following should prompt careful examination:[5]
- Architecture: microfollicular, trabecular, solid, insular.
- Thick capsule.
- Necrosis - rare in the thyroid.
Thyroid IHC - general comments
- Not really useful.
- Papers with very small sample sizes abound.
Follicular thyroid carcinoma vs. papillary thyroid carcinoma
- CD31 more frequently positive in follicular lesions.[6]
- CD31 is a marker for microvessel density.
- Galectin-3 thought to be positive in papillary carcinoma.[6]
- HBME-1 thought to be positive in papillary lesions.[7]
Thyroid lesions per WHO
- Adapted from the Washington Manual of Surgical Pathology.[8]
Adenoma
- Follicular adenoma.
- Hyalinizing trabecular tumour.
Carcinoma
- Papillary carcinoma.
- Follicular carinoma.
- Medullary carcinoma.
- Undifferentiated (anaplastic) carcinoma.
- Poorly differentiated carcinoma.
- Squamous cell carcinoma.
- Mucoepidermoid carcinoma.
- Sclerosing mucoepidermoid carcinoma with eosinophilia.
- Mucinous carcinoma.
- Mixed medullary and follicular carinoma.
- Spindle cell tumour with thymus-like differentiation.
- Carcinoma showing thymus-like differentiation.
Others
- Teratoma.
- Lymphoma.
- Ectopic thymoma.
- Angiosarcoma + other soft tissue lesions.
- Paraganglioma.
- Solitary fibrous tumour.
- Follicular dendritic cell tumour.
- Langerhans cell histiocytosis.
- Metastasis.
Parathyroid glands
- May make an appearance in the context of thyroid surgery.
Benign
Solid cell nest of the thyroid gland
- AKA solid cell nest of thyroid.
General
- Embryonic remnants endodermal origin.[9]
- Incidental finding.
Note:
- Hypothesized to have some relation to mucoepidermoid carcinoma of the thyroid gland;[10] however, another study suspects a relationship with papillary thyroid carcinoma.[11]
Microscopic
Features:[9]
- Cellular solid or cystic cluster of variable size with:
- Cuboidal cellular morphology.
- May have columnar morphology.
- Moderate-to-scant eosinophilic cytoplasm.
- Round/ovoid nuclei with finely granular chromatin.
- Cuboidal cellular morphology.
- +/-Goblet cells (~30% of cases).[12]
DDx:[9]
- C-cell hyperplasia.
- Medullary carcinoma.
- Squamous lesions.
Images
www:
IHC
Features:[9]
- p63 +ve.
- -ve in clear cells.
- CEA +ve (polyconal).[12]
- +ve also in clear cells.
- Chromogranin A +ve ~45% of cases.[12]
Sign out
Solid cell nests of the thyroid gland are usually not reported.
Thyroid gland nodular hyperplasia
- AKA nodular hyperplasia.
- AKA adenomatoid nodule.
Follicular thyroid adenoma
Graves disease
Idiopathic granulomatous thyroiditis
- AKA granulomatous thyroiditis - non-specific term; granulomas may be due a number of causes.
- AKA subacute thyroiditis.
- AKA de Quervain thyroiditis.
- Should not be confused with de Quervain's disease (AKA gamer's thumb) something completely unrelated to the thyroid.
General
- Women > men.
- Etiology: possibly viral.[13]
Clinical:
- Tenderness.[14]
Management:
- Medical.
- Rarely surgery.[15]
Microscopic
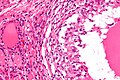
- Granulomas with multinucleated giant cells - usu. with engulfed colloid.
- Lymphocytes.
- Plasma cells.
- +/-Fibrosis.
DDx:
- Infectious granulomatous disease (fungal, microbacterial).
- Palpation thyroiditis.
- Sarcoidosis (classically intrafollicular distribution).
Images
Stains
- ZN -ve.
- GMS -ve.
Palpation thyroiditis
General
- Granulomatous inflammation due to palpation.
- Incidence of granulomas higher in surgical thyroid specimens than autopsies.[13]
Microscopic
Features:[13]
- Granulomas involving the follicle.
- Histiocytes within the colloid.
DDx:
- Idiopathic granulomatous thyroiditis.
- Sarcoidosis.
- Infectious granulomatous thyroiditis.
Stains
- ZN -ve.
- GMS -ve.
Riedel thyroiditis
Hashimoto thyroiditis
C-cell hyperplasia
- Abbreviated CCH.
Adenolipoma of the thyroid
Malignant neoplasm
There are a bunch of 'em. The most common, by far, is papillary.
Papillary thyroid carcinoma
- Abbreviated PTC.
Insular carcinoma
Follicular thyroid carcinoma
- AKA follicular carcinoma.
Medullary thyroid carcinoma
- Abbreviated MTC.
Poorly differentiated thyroid carcinoma
Anaplastic thyroid carcinoma
Lymphomas of the thyroid
General
- Rare.
- Increased risk with chronic inflammatory conditions.
- Fit in the the greater category of MALT lymphoma.
Microscopic
Features:
- Lymphoepithelial lesion - key feature.
- Plasma cells.
- "Overgrowth" - thyroid parenchyma displaced by lymphocytes.
Weird stuff
Hyalinizing trabecular tumour
- AKA hyalinizing trabecular adenoma.
- Abbreviated HTT.
Hürthle cell neoplasm
- AKA oncocytic neoplasm.
- Also spelled Hurthle cell neoplasm.
Minocycline associated thyroid pigmentation
- AKA minocycline thyroid.
General
- Benign pigmentation of the thyroid due to minocycline, an antibiotic.
- Reported at other sites, e.g. heart valves,[18] skin,[19] coronary arteries.
Gross
- Black thyroid.[20]
Images:
- Pigmented thyroid gland (rheumatology.org).
- Minocycline thyroid - gross and microscopic (archivesofpathology.org).[21]
Microscopic
Features:
- Granular yellow blobs:
- Location:
- Intracytoplasmic in the follicule-lining cells, i.e. follicular cells.
- Intrafollicular.
- Variable size ~0.5-4 micrometers.
- Location:
Notes:
- Pigment described as lipofuscin-like.[22]
Images
Stains
Sclerosing mucoepidermoid carcinoma with eosinophilia
See also
References
- ↑ BEC. 20 October 2009.
- ↑ JOHNSON, RW.; SAHA, NC. (Jun 1962). "The so-called lateral aberrant thyroid.". Br Med J 1 (5293): 1668-9. PMC 1958877. PMID 14452106. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1958877/.
- ↑ Escofet, X.; Khan, AZ.; Mazarani, W.; Woods, WG. (Jan 2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Promot Health 127 (1): 45-6. PMID 17319317.
- ↑ URL: http://radiopaedia.org/articles/lymph-node-levels-of-the-neck. Accessed on: 5 November 2012.
- ↑ SR. 17 January 2011.
- ↑ 6.0 6.1 Rydlova, M.; Ludvikova, M.; Stankova, I. (Jun 2008). "Potential diagnostic markers in nodular lesions of the thyroid gland: an immunohistochemical study.". Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 152 (1): 53-9. PMID 18795075.
- ↑ Papotti, M.; Rodriguez, J.; De Pompa, R.; Bartolazzi, A.; Rosai, J. (Apr 2005). "Galectin-3 and HBME-1 expression in well-differentiated thyroid tumors with follicular architecture of uncertain malignant potential.". Mod Pathol 18 (4): 541-6. doi:10.1038/modpathol.3800321. PMID 15529186.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 331. ISBN 978-0781765275.
- ↑ 9.0 9.1 9.2 9.3 Reis-Filho JS, Preto A, Soares P, Ricardo S, Cameselle-Teijeiro J, Sobrinho-Simões M (January 2003). "p63 expression in solid cell nests of the thyroid: further evidence for a stem cell origin". Mod. Pathol. 16 (1): 43–8. doi:10.1097/01.MP.0000047306.72278.39. PMID 12527712. http://www.nature.com/modpathol/journal/v16/n1/full/3880708a.html.
- ↑ Ozaki, O.; Ito, K.; Sugino, K.; Yasuda, K.; Yamashita, T.; Toshima, K.. "Solid cell nests of the thyroid gland: precursor of mucoepidermoid carcinoma?". World J Surg 16 (4): 685-8; discussion 688-9. PMID 1413837.
- ↑ Prichard, RS.; Lee, JC.; Gill, AJ.; Sywak, MS.; Fingleton, L.; Robinson, BG.; Sidhu, SB.; Delbridge, LW. (Feb 2012). "Mucoepidermoid carcinoma of the thyroid: a report of three cases and postulated histogenesis.". Thyroid 22 (2): 205-9. doi:10.1089/thy.2011.0276. PMID 22224821.
- ↑ 12.0 12.1 12.2 Mizukami Y, Nonomura A, Michigishi T, et al. (February 1994). "Solid cell nests of the thyroid. A histologic and immunohistochemical study". Am. J. Clin. Pathol. 101 (2): 186–91. PMID 7509563.
- ↑ 13.0 13.1 13.2 13.3 Lloyd, Ricardo V. (2002). Endocrine Diseases (AFIP Atlas of Nontumor Pathology). Toronto: American Registry of Pathology. ISBN 978-1881041733. http://www.amazon.com/Endocrine-Diseases-Atlas-Nontumer-Pathology/dp/1881041735.
- ↑ Szczepanek-Parulska, E.; Zybek, A.; Biczysko, M.; Majewski, P.; Ruchała, M. (2012). "What might cause pain in the thyroid gland? Report of a patient with subacute thyroiditis of atypical presentation.". Endokrynol Pol 63 (2): 138-42. PMID 22538753.
- ↑ Volpé, R. (1993). "The management of subacute (DeQuervain's) thyroiditis.". Thyroid 3 (3): 253-5. PMID 8257868.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 559. ISBN 978-0781740517.
- ↑ Fatourechi, MM.; Hay, ID.; McIver, B.; Sebo, TJ.; Fatourechi, V. (Jul 2011). "Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008.". Thyroid 21 (7): 765-72. doi:10.1089/thy.2010.0453. PMID 21568724.
- ↑ 18.0 18.1 Sant'Ambrogio, S.; Connelly, J.; DiMaio, D.. "Minocycline pigmentation of heart valves.". Cardiovasc Pathol 8 (6): 329-32. PMID 10615019.
- ↑ Geria AN, Tajirian AL, Kihiczak G, Schwartz RA (2009). "Minocycline-induced skin pigmentation: an update". Acta Dermatovenerol Croat 17 (2): 123–6. PMID 19595269.
- ↑ Noble, JG.; Christmas, TJ.; Chapple, C.; Katz, D.; Milroy, EJ. (Jan 1989). "The black thyroid: an unusual finding during neck exploration.". Postgrad Med J 65 (759): 34-5. PMC 2429157. PMID 2780449. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2429157/.
- ↑ 21.0 21.1 Raghavan, R.; Snyder, WH.; Sharma, S. (Mar 2004). "Pathologic quiz case: tumor in pigmented thyroid gland in a young man. Papillary thyroid carcinoma in a minocycline-induced, diffusely pigmented thyroid gland.". Arch Pathol Lab Med 128 (3): 355-6. doi:10.1043/1543-2165(2004)128355:PQCTIP2.0.CO;2. PMID 14987144.
- ↑ Gordon, G.; Sparano, BM.; Kramer, AW.; Kelly, RG.; Iatropoulos, MJ. (Oct 1984). "Thyroid gland pigmentation and minocycline therapy.". Am J Pathol 117 (1): 98-109. PMC 1900569. PMID 6435454. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1900569/.