Papillary thyroid carcinoma
Papillary thyroid carcinoma, abbreviated PTC, is the most common thyroid gland malignancy. It usually has an indolent course.
| Papillary thyroid carcinoma | |
|---|---|
| Diagnosis in short | |
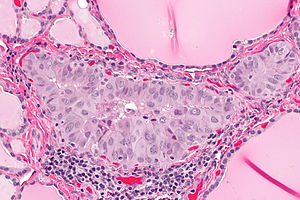 Papillary thyroid carcinoma. H&E stain. | |
|
| |
| LM | nuclear changes: nuclear membrane irregularities (e.g. raisinoid shape), +/-nuclear grooves, +/-nuclear pseudoinclusions, +/-nuclear clearing, nuclear enlargement (usu. mild), nucleoli; architectural changes: overlap of nuclei, papillae (not required), +/-psammoma bodies |
| Subtypes | tall cell variant, columnar cell variant, follicular variant, cribriform-morular variant, diffuse sclerosing variant, Warthin-like variant, solid variant, oncocytic variant, others |
| LM DDx | lymphocytic thyroiditis (Graves disease, Hashimoto thyroiditis), solid cell nest of thyroid, follicular thyroid carcinoma, follicular thyroid adenoma, adenomatoid nodule |
| IHC | HBME-1 +ve, CK19 +ve, Galectin-3 +ve, thyroglobulin +ve, TTF-1 +ve |
| Site | thyroid gland |
|
| |
| Syndromes | familial adenomatous polyposis (cribriform-morular variant) |
|
| |
| Signs | thyroid mass |
| Prevalence | very common |
| Prognosis | usu. good |
| Clin. DDx | other thyroid gland tumours |
General
Medical school memory device P's:
- Palpable lymph nodes.
- Popular - most common malignant neoplasm of the thyroid.
- Prognosis is good.
- Pre-Tx iodine scan.
- Post-Sx iodine scan.
- Psammoma bodies.
Notes:
- PTC is associated with radiation exposure.[1]
- Papillary thyroid microcarcinoma is defined as a tumour with a maximal dimension of 1.0 cm or less.[2]
Prognosis
Prognosis can be predicted by MAICS score. It which includes:[3]
- Metastases.
- Age.
- Invasion of surround tissues.
- Completeness of excision.
- Size of tumour.
Microscopic
Features:
- Nuclear changes - key feature.
- "Shrivelled nuclei"/"raisin" like nuclei, nuclei with a wavy ("textured", convoluted) nuclear membrane -- usu. easy to find.
- Nuclear pseudoinclusions -- usu. harder to find; have high specificity (nuclear pseudoinclusions appear as a result of the very convoluted nuclear membrane wrapping around parts of the cytoplasm; true nuclear inclusions in contrast are seen only in viral infections).
- Nuclear grooves, seen as a result of the highly "textured" nuclear membrane.
- Nuclear clearing (only on permanent section) - also known as "Orphan Annie eyes".
- Overlap of nuclei - "cells do not respect each other's borders" (easy to see at key feature at low power).
- Classically has papillae (nipple-like shape); papilla (definition): epithelium on fibrovascular core.
- Absence of papillae does not exclude diagnosis.
- Psammoma bodies.
- Circular, acellular, eosinophilic whorled bodies.
- Not necessary to make diagnosis - but very specific in the context of a specimen labeled "thyroid".
- Arise from infarction & calcification of papilla tips.[4]
Notes:
- Psammoma bodies are awesome if you see 'em, i.e. useful for arriving at the diagnosis.
- If there are no papillae structures -- you're unlikely to see psammoma bodies.
- At low power look for cellular areas/loss of follicles.
- Nuclear clearing seen in:
- Nuclear overlapping is easy to see at lower power-- should be the tip-off to look at high power for nuclear features.
- Nuclear inclusions are quite rare and not required to make the diagnosis -- but a very convincing feature if seen.
- Papillae may be seen in Graves disease.
- Thyroid tissue lateral to the jugular vein (often referred to as lateral aberrant thyroid tissue) is generally considered metastatic thyroid carcinoma (papillary thyroid carcinoma) even if it looks benign.[6]
- This dictum is disputed.[7]
- The level VI and VII lymph nodes are medial to the jugular.
DDx:
Subtypes of papillary thyroid carcinoma
There are many.
Poor prognosis variants:
Papillary thyroid carcinoma tall cell variant
General
- ~10% of PTC.[11]
- Often large > 6 cm.
Microscopic
Features:[12]
- 50% of cells with height 2x the width.[13]
- Eosinophilic cytoplasm.
- Well-defined cell borders.
- Nucleus stratified; basal location, i.e. closer to the basement membrane.
Negative:
- Nuclei not pseudostratified, if pseudostratified consider columnar cell variant.
Images:
Papillary thyroid carcinoma columnar cell variant
General
Epidemiology:
- Poor prognosis.
- Very rare.
Microscopic
Features:[15]
- Elongated nuclei (similar to colorectal adenocarcinoma) - key feature.
- +/-Pseudostratification of the nuclei (like in colorectal adenocarcinoma), differentiates from tall cell variant.
- Nuclear stratification - key feature.
- "Minimal" papillary features.
- "Tall cells".
- Clear-eosinophilic cytoplasm.
- Mitoses common.
Image: Columnar variant PTC (wiley.com).
Papillary thyroid carcinoma follicular variant
General
- May be confused with follicular carcinoma or follicular adenoma.
- Pathologists often disagree about this diagnosis.[16]
Microscopic
Features:[17]
- Small tightly packed follicles - key feature.
- Hypereosinophilic colloid.
- Nuclear features of PTC.
- Large nuclei.
- Typically have less nuclear pseudoinclusions than the conventional type.
- +/-Fibrous capsule (common).
DDx:
- Follicular thyroid carcinoma - has a fibrous capsule and invasion though it.
- Follicular thyroid adenoma - surrounded by a fibrous capsule.
- Adenomatoid nodule - round nuclei, no nuclear features of PTC.
Images:
- PTC follicular variant (surgicalpathologyatlas.com).
- PTC follicular variant (surgicalpathologyatlas.com).
- PTC follicular variant (thyroidcancercanada.org).[18]
Papillary thyroid carcinoma cribriform-morular variant
General
- Associated with familial adenomatous polyposis (FAP).[19]
Microscopic
Features:
- Circumscribed or even encapsulated neoplasm.
- Morules - interspersed balls of squamoid cells
- No keritinization or intercellular bridges.
- Homogenous, lightly eosinophilic glassy nuclei (biotin accumulation).
- Follicles
- Cribriform, papillary, trabecular and solid patterns.
- Columnar or cuboidal cells.
- Little colloid
- Papillary carcinoma nuclear features.
DDX:
- Papillary thyroid carcinoma
- Papillary thyroid carcinoma, tall cell variant
IHC
- CDX2 - Highlights the morules (CDX2 is positive in the biotin rich nuclei associated with morule formation in a variety of situations)[20]
- CD10 - Highlights the morules [21]
- Beta-catenin - nuclear and cytoplasmic - all tumour cells.
- Estrogen receptor - positive
- TTF-1 - positive
Molecular
- Up-regulating disturbances in the Wnt signaling pathway promote formation of morules with optically clear biotin rich nuclei [22]
- Mutation of the beta-catenin gene
- Mutation in APC
- Examples
- Well-differentiated fetal adenocarcinoma
- Papillary thyroid carcinoma, cribriform morular variant (mutation in APC in familial variants)
- Pancreatoblastoma
Papillary thyroid carcinoma diffuse sclerosing variant
General
- Usually young adults, children.
Microscopic
Features:[23]
- Papillae - usu. prominent.
- Squamous morules - key features.[24]
- Lymphocytes - abundant.
- Fibrosis.
DDx:
- Lymphocytic thyroiditis (esp. Hashimoto's thyroiditis).
Papillary thyroid carcinoma Warthin-like variant
- Resembles Warthin tumour.
Microscopic
Features:[15]
- Eosinophilic cytoplasm.
- Lymphocytic thyroiditis.
- Papillae.
Papillary thyroid carcinoma solid variant
Features:[9]
- Some studies suggest this has a poor prognosis.
- More common in children.
- Associated with Chernobyl nuclear accident.
Microscopic
Features:
- Solid sheets >50% of tumour mass.[9]
Papillary thyroid carcinoma oncocytic variant
Features:
- Possible association with autoimmune thyroiditis.[25]
Microscopic
Features:[25]
- Abundant oncocytic tumour cells with apical nuclei.
- Classic features of PTC:
- Grooves and and abundant pseudoinclusions.[26]
- >70% papillary architecture.[26]
- +/-Degenerative changes.
Note:
- CK19 +ve -- though not specific or sensitive.
IHC
Thyroid versus something else:
- Thyroglobulin +ve.
- TTF-1 (thyroid transcription factor-1) +ve.
- CD15 +ve.[citation needed]
PTC versus benign:[27]
- HBME-1 +ve (strong, diffuse).
- CK19 +ve (strong, diffuse).
- Galectin-3 +ve (strong, diffuse).
Molecular
- Currently not widely used in a diagnostic context.
Tabular summary
Molecular changes in papillary thyroid carcinoma as per Adeniran et al:[28]
| Molecular change | Frequency | Histology | Notes |
|---|---|---|---|
| BRAF point mutations | ~ 40% | tall cell variant | poorer prognosis, older individuals |
| RET/PTC rearrangments | ~ 20% | papillary architecture, psammoma bodies | younger individuals |
| RAS point mutations | ~ 15% | exclusively follicular variant | - |
Sign out
HEMITHYROID, RIGHT, COMPLETION OF TOTAL THYROIDECTOMY: - PAPILLARY THYROID CARCINOMA, FOLLICULAR VARIANT. -- TUMOUR SIZE: 4 MM (MAXIMAL). -- ARCHITECTURE: FOLLICULAR. -- CYTOMORPHOLOGY: CLASSICAL. -- HISTOLOGIC GRADE: G1 (WELL DIFFERENTIATED). -- NO TUMOUR CAPSULE IDENTIFIED. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. -- NEGATIVE FOR EXTRATHYROIDAL EXTENSION. -- SURGICAL MARGINS NEGATIVE FOR MALIGNANCY.
Note:
- If it is a completion thyroidectomy and the staging changes one should do a full synoptic report.
Microcarcinoma
A. LEFT HEMITHYROID, THYROIDECTOMY COMPLETION: - PAPILLARY THYROID MICROCARCINOMA. -- MARGINS NEGATIVE FOR MALIGNANCY. -- TUMOUR SIZE ~ 1 MILLIMETRE. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - PALPATION THYROIDITIS, FOCAL. - NODULAR HYPERPLASIA. B. LYMPH NODES, LEVEL 6 AND 7, LYMPH NODE DISSECTION: - TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ).
THYROID GLAND, TOTAL THYROIDECTOMY: - INCIDENTAL PAPILLARY THYROID MICROCARCINOMA. -- MARGINS NEGATIVE FOR MALIGNANCY. -- TUMOUR SIZE ~ 1 MILLIMETRE. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - NODULAR HYPERPLASIA. - ONE PARATHYROID GLAND.
Lymph node dissection
A. NECK, RIGHT LEVEL 2 AND 3, LYMPH NODE DISSECTION: - ONE LYMPH NODE POSITIVE FOR PAPILLARY THYROID CARCINOMA ( 1 POSITIVE / 4 ). B. NECK, RIGHT LEVEL 4, LYMPH NODE DISSECTION: - TWO LYMPH NODES, NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ). C. NECK, RIGHT LEVEL 6 AND 7, LYMPH NODE DISSECTION: - ONE LYMPH NODE POSITIVE FOR PAPILLARY THYROID CARCINOMA ( 1 POSITIVE / 3 ).
Micro
The sections show lymph nodes with tumour that has a papillary architecture. The tumour cell nuclei are enlarged and overlap. They also have nuclear grooves, nucleoli and abundant pseudoinclusions. The chromatin of the tumour cells has a powdery appearance.
See also
References
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 564. ISBN 978-0781740517.
- ↑ Sethom, A.; Riahi, I.; Riahi, K.; Akkari, K.; Benzarti, S.; Miled, I.; Chebbi, MK. (Jan 2011). "[Management of thyroid microcarcinoma. Report of 13 cases].". Tunis Med 89 (1): 23-5. PMID 21267823.
- ↑ Hay, ID.; Thompson, GB.; Grant, CS.; Bergstralh, EJ.; Dvorak, CE.; Gorman, CA.; Maurer, MS.; McIver, B. et al. (Aug 2002). "Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients.". World J Surg 26 (8): 879-85. doi:10.1007/s00268-002-6612-1. PMID 12016468.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 565. ISBN 978-0781740517.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 566. ISBN 978-0781740517.
- ↑ JOHNSON, RW.; SAHA, NC. (Jun 1962). "The so-called lateral aberrant thyroid.". Br Med J 1 (5293): 1668-9. PMC 1958877. PMID 14452106. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1958877/.
- ↑ Escofet, X.; Khan, AZ.; Mazarani, W.; Woods, WG. (Jan 2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Promot Health 127 (1): 45-6. PMID 17319317.
- ↑ Baloch, ZW.; LiVolsi, VA. (Jun 2006). "Cytologic and architectural mimics of papillary thyroid carcinoma. Diagnostic challenges in fine-needle aspiration and surgical pathology specimens.". Am J Clin Pathol 125 Suppl: S135-44. PMID 16830963.
- ↑ 9.0 9.1 9.2 9.3 9.4 Gonzalez-Gonzalez, R.; Bologna-Molina, R.; Carreon-Burciaga, RG.; Gómezpalacio-Gastelum, M.; Molina-Frechero, N.; Salazar-Rodríguez, S. (2011). "Papillary thyroid carcinoma: differential diagnosis and prognostic values of its different variants: review of the literature.". ISRN Oncol 2011: 915925. doi:10.5402/2011/915925. PMC 3302055. PMID 22432054. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3302055/.
- ↑ URL: http://emedicine.medscape.com/article/849000-overview#a0104. Accessed on: 1 May 2012.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 505. ISBN 978-0781779425.
- ↑ Urano M, Kiriyama Y, Takakuwa Y, Kuroda M (April 2009). "Tall cell variant of papillary thyroid carcinoma: Its characteristic features demonstrated by fine-needle aspiration cytology and immunohistochemical study". Diagn. Cytopathol.. doi:10.1002/dc.21086. PMID 19373912.
- ↑ 13.0 13.1 Ghossein R, Livolsi VA (November 2008). "Papillary thyroid carcinoma tall cell variant". Thyroid 18 (11): 1179–81. doi:10.1089/thy.2008.0164. PMID 18925842.
- ↑ S. Raphael. 17 January 2011.
- ↑ 15.0 15.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 506. ISBN 978-0781779425.
- ↑ Daniels, GH.. "What if many follicular variant papillary thyroid carcinomas are not malignant? A review of follicular variant papillary thyroid carcinoma and a proposal for a new classification.". Endocr Pract 17 (5): 768-87. doi:10.4158/EP10407.RA. PMID 21940284.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 88. ISBN 978-0443066856.
- ↑ URL: http://www.thyroidcancercanada.org/types-of-thyroid-cancer.php?lang=en. Accessed on: 9 January 2013.
- ↑ Groen EJ, Roos A, Muntinghe FL, et al. (September 2008). "Extra-intestinal manifestations of familial adenomatous polyposis". Ann. Surg. Oncol. 15 (9): 2439–50. doi:10.1245/s10434-008-9981-3. PMC 2518080. PMID 18612695. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518080/?tool=pubmed.
- ↑ Wani, Y.; Notohara, K.; Nakatani, Y.; Matsuzaki, A. (Oct 2009). "Aberrant nuclear Cdx2 expression in morule-forming tumours in different organs, accompanied by cytoplasmic reactivity.". Histopathology 55 (4): 465-8. doi:10.1111/j.1365-2559.2009.03382.x. PMID 19817898.
- ↑ Cameselle-Teijeiro, J.; Alberte-Lista, L.; Chiarelli, S.; Buriticá, C.; Gonçalves, L.; González-Cámpora, R.; Nogales, FF. (Feb 2008). "CD10 is a characteristic marker of tumours forming morules with biotin-rich, optically clear nuclei that occur in different organs.". Histopathology 52 (3): 389-92. doi:10.1111/j.1365-2559.2007.02911.x. PMID 18081818.
- ↑ Gamachi, A.; Kashima, K.; Daa, T.; Nakatani, Y.; Tsujimoto, M.; Yokoyama, S. (Nov 2003). "Aberrant intranuclear localization of biotin, biotin-binding enzymes, and beta-catenin in pregnancy-related endometrium and morule-associated neoplastic lesions.". Mod Pathol 16 (11): 1124-31. doi:10.1097/01.MP.0000092953.20717.48. PMID 14614052.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1122. ISBN 978-1416031215.
- ↑ Hirokawa, M.; Kuma, S.; Miyauchi, A.; Qian, ZR.; Nakasono, M.; Sano, T.; Kakudo, K.. "Morules in cribriform-morular variant of papillary thyroid carcinoma: Immunohistochemical characteristics and distinction from squamous metaplasia.". APMIS 112 (4-5): 275-82. doi:10.1111/j.1600-0463.2004.apm11204-0508.x. PMID 15233643.
- ↑ 25.0 25.1 Berho, M.; Suster, S. (Jan 1997). "The oncocytic variant of papillary carcinoma of the thyroid: a clinicopathologic study of 15 cases.". Hum Pathol 28 (1): 47-53. PMID 9013831.
- ↑ 26.0 26.1 Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 86. ISBN 978-0443066856.
- ↑ Mataraci, EA.; Ozgüven, BY.; Kabukçuoglu, F. (Mar 2012). "Expression of cytokeratin 19, HBME-1 and galectin-3 in neoplastic and nonneoplastic thyroid lesions.". Pol J Pathol 63 (1): 58-64. PMID 22535608.
- ↑ Adeniran, AJ.; Zhu, Z.; Gandhi, M.; Steward, DL.; Fidler, JP.; Giordano, TJ.; Biddinger, PW.; Nikiforov, YE. (Feb 2006). "Correlation between genetic alterations and microscopic features, clinical manifestations, and prognostic characteristics of thyroid papillary carcinomas.". Am J Surg Pathol 30 (2): 216-22. PMID 16434896.