Difference between revisions of "Ischemic colitis"
(+infobox) |
|||
| Line 26: | Line 26: | ||
| Prognosis = poor if severe | | Prognosis = poor if severe | ||
| Other = | | Other = | ||
| ClinDDx = other causes of [[colitis]] | | ClinDDx = other causes of [[colitis]], esp. [[infectious colitis]] | ||
}} | }} | ||
'''Ischemic colitis''' is inflammation of the [[colon]] due to a compromised blood supply. | '''Ischemic colitis''' is inflammation of the [[colon]] due to a compromised blood supply. | ||
| Line 49: | Line 49: | ||
Note: | Note: | ||
*Ischemia = compromised blood supply. | *Ischemia = compromised blood supply. | ||
Clinical - classic presentation:<ref name=pmid24070152>{{Cite journal | last1 = Tadros | first1 = M. | last2 = Majumder | first2 = S. | last3 = Birk | first3 = JW. | title = A review of ischemic colitis: is our clinical recognition and management adequate? | journal = Expert Rev Gastroenterol Hepatol | volume = 7 | issue = 7 | pages = 605-13 | month = Sep | year = 2013 | doi = 10.1586/17474124.2013.832485 | PMID = 24070152 }}</ref> | |||
*Abdominal pain. | |||
*Urgency to defecate. | |||
*Bloody diarrhea. | |||
Note: | |||
*Diarrhea may be non-bloody. | |||
**This is a poor prognosticator<ref name=pmid20961178>{{Cite journal | last1 = Montoro | first1 = MA. | last2 = Brandt | first2 = LJ. | last3 = Santolaria | first3 = S. | last4 = Gomollon | first4 = F. | last5 = Sánchez Puértolas | first5 = B. | last6 = Vera | first6 = J. | last7 = Bujanda | first7 = L. | last8 = Cosme | first8 = A. | last9 = Cabriada | first9 = JL. | title = Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). | journal = Scand J Gastroenterol | volume = 46 | issue = 2 | pages = 236-46 | month = Feb | year = 2011 | doi = 10.3109/00365521.2010.525794 | PMID = 20961178 }}</ref> and possibly increases likelihood of not identifying it in time. | |||
==Gross== | ==Gross== | ||
Revision as of 02:34, 12 December 2013
| Ischemic colitis | |
|---|---|
| Diagnosis in short | |
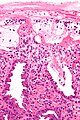
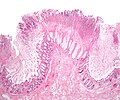
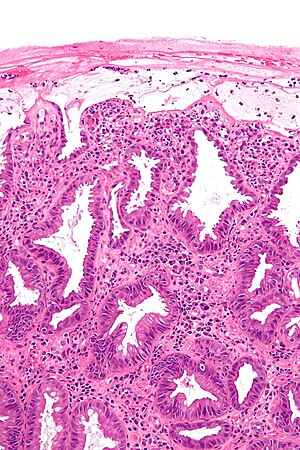 Ischemic colitis. H&E stain. | |
|
| |
| LM | withering crypts (colonic epithelium has decreased cytoplasm - NC ratio increased, usually with decreased goblet cells), crypt loss/drop-out, lamina propria hyalinization, submucosa hyalinization, +/-pseudomembranes, +/-vascular thrombi |
| LM DDx | inflammatory bowel disease, radiation colitis, toxins/drugs, infectious colitis |
| Gross | dusky appearing, +/-bowel wall thinning, +/-dilation |
| Site | colon |
|
| |
| Associated Dx | atherosclerosis |
| Clinical history | +/-cardiovascular disease |
| Signs | +/-blood per rectum, +/-diarrhea (may be non-bloody) |
| Blood work | +/-anemia |
| Prognosis | poor if severe |
| Clin. DDx | other causes of colitis, esp. infectious colitis |
Ischemic colitis is inflammation of the colon due to a compromised blood supply.
It is also known as colonic ischemia and ischemia of the colon.
General
- May occur together with ischemic enteritis, in which case it is known as ischemic enterocolitis.
Etiology - anything that leads to vascular occlusion:
- Atherosclerosis.
- Vasculitis.
- Embolization, e.g. thrombotic, foreign body.
Possible associated pathology:
- Necrotizing enteritis - necrosis of the small bowel only.
- Necrotizing enterocolitis - necrosis of the small and large bowel.
Closely related:
Note:
- Ischemia = compromised blood supply.
Clinical - classic presentation:[1]
- Abdominal pain.
- Urgency to defecate.
- Bloody diarrhea.
Note:
- Diarrhea may be non-bloody.
- This is a poor prognosticator[2] and possibly increases likelihood of not identifying it in time.
Gross
Features - location:[3]
- Luminal part (mucosa & submucosa) affected - edema.
- Splenic flexture of colon commonly affected (vascular watershed).
Note:
- May have pseudomembranes (classically assoc. with C. difficile colitis), i.e. mimics an infectious process.
- DDx for pseudomembranes:[4]
- C. difficile induced pseudomembranous colitis.
- Ischemic colitis.
- Volvulus.
- Necrotizing infections.
- ... anything that causes severe mucosal injury.
- Radiologic correlate = bowel wall thickening.
Microscopic
Features:
- Withering crypts - important.
- Colonic epithelium has decreased cytoplasm - NC ratio increased.
- Usually with decreased goblet cells.
- Crypt loss/drop-out.
- Less intestinal crypts present.
- Lamina propria hyalinization.
- Dense pink material replaces loose connective tissue.
- Submucosa hyalinization.
- +/-Pseudomembranes (microscopic):[4]
- Loss of surface epithelium.
- PMNs in lamina propria.
- +/-Capillary fibrin thrombi.
Note:
- Pseudomembranes arise from the crypts - considered acute.
DDx:
- Inflammatory bowel disease.
- Radiation colitis.
- Toxins/drugs.
- Infectious colitis.
Images
www:
Sign out
Biopsy
TRANSVERSE COLON, BIOPSY: - SEVERE ACTIVE COLITIS WITH ATTENUATED EPITHELIAL CYTOPLASM AND ULCERATION. - CELLULAR DEBRIS. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The attenuated cytoplasm is compatible with ischemia; however, it is not accompanied with other suggestive findings (crypt drop out, lamina propria fibrosis, pseudomembranes). The crypt architecture is test tube-like. The differential diagnosis includes: ischemia, drug reaction, infectious etiologies and, less likely, inflammatory bowel disease. Clinical correlation is required.
COLON, SPLENIC FLEXURE, BIOPSY: - PATCHY MODERATE ACTIVE COLITIS WITH ATTENUATED EPITHELIAL CYTOPLASM, FOCALLY DECREASED GOBLET CELLS AND ULCERATION. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with ischemia; however, they are not diagnostic. The differential diagnosis includes: ischemia, drug reaction, infectious etiologies and, less likely, inflammatory bowel disease. Clinical correlation is required.
Short version
LEFT COLON AND SIGMOID COLON, RESECTION: - PSEUDOMEMBRANOUS COLITIS, SEE COMMENT. - ONE LYMPH NODE NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 1 ). - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: Pseudomembrane formation is a non-specific finding. It is consistent with ischemia; however, it may be seen in other contexts, including infection. Clinical correlation is required.
Long version
RECTOSIGMOID, RESECTION: - BOWEL WALL ISCHEMIA WITH PERFORATION, SEROSITIS, MICROABSCESS FORMATION AND FOCAL POORLY FORMED PSEUDOMEMBRANES. - NEGATIVE FOR MALIGNANCY. - PLEASE SEE COMMENT. COMMENT: There is no evidence of inflammatory bowel disease: The unaffected mucosa does not have obvious architectural distortion. No granulomas are identified. The inflammation is largely associated with necrosis/ischemic changes and favoured to be reactive. The poorly formed pseudomembranes are associated with mural ischemic changes; they do not specifically suggest an infection in this context. The blood vessels do not show a vasculitis, or significant atherosclerosis. Thrombi are seen on several sections and found predominantly in the (smaller) veins. Considerations are thrombosis, thromboembolism, mechanical vascular compromise, and infectious etiologies. A vascular compromise is favoured as the underlying cause. Clinical and radiologic correlation is suggested.
Another long version
SIGMOID COLON, RESECTION: - BOWEL WALL ISCHEMIA WITH PERFORATION, SEROSITIS, AND FOCAL POORLY FORMED PSEUDOMEMBRANES. - MILD ATHEROSCLEROSIS. - DIVERTICULAR DISEASE. - TWO LYMPH NODES NEGATIVE FOR MALIGNANCY ( 0 POSITIVE / 2 ). - PLEASE SEE COMMENT. COMMENT: The sections show the changes of acute and chronic ischemic colitis (submucosal fibrosis, lamina propria hyalinization, focal crypt drop-out, decreased goblet cells, pigmented macrophages in the lamina propria, intraepithelial neutrophils). No granulomas are identified. The inflammation is largely associated with the necrosis/ischemic changes and favoured to be reactive. The poorly formed pseudomembranes are associated with mural ischemic changes; they do not specifically suggest an infectious etiology in this context. The blood vessels do not show a vasculitis. However, focal neutrophilic perivascular inflammation is seen; this is probably a reactive process. No vascular thrombi are identified. The findings are compatible with perforation secondary to a foreign body in the setting of chronic ischemia.
Micro
Negative for ischemic colitis
The sections show colorectal mucosa with preservation of the crypt density and epithelium with a normal nuclear-to-cytoplasm ratio. There is no apparent lamina propria hyalinization. The muscularis mucosa is prominent. Focally, lymphoid aggregates are present.
No cryptitis is present. Neutrophils are not apparent in the lamina propria. No erosions are identified.
The epithelium matures appropriately from the crypt base to the surface.
See also
References
- ↑ Tadros, M.; Majumder, S.; Birk, JW. (Sep 2013). "A review of ischemic colitis: is our clinical recognition and management adequate?". Expert Rev Gastroenterol Hepatol 7 (7): 605-13. doi:10.1586/17474124.2013.832485. PMID 24070152.
- ↑ Montoro, MA.; Brandt, LJ.; Santolaria, S.; Gomollon, F.; Sánchez Puértolas, B.; Vera, J.; Bujanda, L.; Cosme, A. et al. (Feb 2011). "Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study).". Scand J Gastroenterol 46 (2): 236-46. doi:10.3109/00365521.2010.525794. PMID 20961178.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 852. ISBN 0-7216-0187-1.
- ↑ 4.0 4.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 837-8. ISBN 0-7216-0187-1.
- ↑ Tan, J.; Pretorius, CF.; Flanagan, PV.; Pais, A. (2012). "Adverse drug reaction: rosuvastatin as a cause for ischaemic colitis in a 64-year-old woman.". BMJ Case Rep 2012. doi:10.1136/bcr.11.2011.5270. PMID 22744258.
- ↑ Fabra, I.; Roig, JV.; Sancho, C.; Mir-Labrador, J.; Sempere, J.; García-Ferrer, L. (Jan 2011). "[Cocaine-induced ischemic colitis in a high-risk patient treated conservatively].". Gastroenterol Hepatol 34 (1): 20-3. doi:10.1016/j.gastrohep.2010.10.005. PMID 21237534.
- ↑ Appu, S.; Thompson, G. (Nov 2001). "Gangrenous ischaemic colitis following non-steroidal anti-inflammatory drug overdose.". ANZ J Surg 71 (11): 694-5. PMID 11736840.