Difference between revisions of "Adrenal gland"
(→Myelolipoma: more) |
(→IHC) |
||
| (85 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
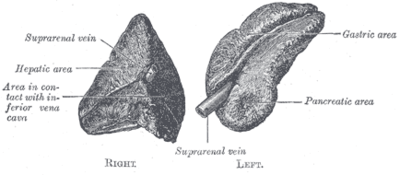
[[Image:Gray1183.png|thumb|400px|A drawing of the adrenal glands.]] | |||
'''Adrenal gland''' is a little organ that hangs-out above the [[kidney]]. Pathologists rarely see it. It uncommonly is affected by tumours. | '''Adrenal gland''' is a little organ that hangs-out above the [[kidney]]. Pathologists rarely see it. It uncommonly is affected by tumours. | ||
==Anatomy & histology== | ==Anatomy & histology== | ||
:''Adrenal cortical rest'' redirects here. | |||
===Anatomy=== | ===Anatomy=== | ||
*Cortex. | *Cortex. | ||
*Medulla. | *Medulla. | ||
=== | Note: | ||
*Adrenal tissue may be associated with gonads or between gonads and adrenal gland proper.<ref>{{Cite journal | last1 = Barwick | first1 = TD. | last2 = Malhotra | first2 = A. | last3 = Webb | first3 = JA. | last4 = Savage | first4 = MO. | last5 = Reznek | first5 = RH. | title = Embryology of the adrenal glands and its relevance to diagnostic imaging. | journal = Clin Radiol | volume = 60 | issue = 9 | pages = 953-9 | month = Sep | year = 2005 | doi = 10.1016/j.crad.2005.04.006 | PMID = 16124976 }}</ref> | |||
===Microscopic=== | |||
It is composed of a ''cortex'' and a ''medulla''. | It is composed of a ''cortex'' and a ''medulla''. | ||
| Line 21: | Line 26: | ||
#*Marked eosinophilia of cytoplasm - '''key feature'''. | #*Marked eosinophilia of cytoplasm - '''key feature'''. | ||
#*Granular/reticular cytoplasm. | #*Granular/reticular cytoplasm. | ||
Note: | |||
*Normal cortex may not be completely encapsulated, i.e. the adrenal capsule may have defects.<ref>{{Ref_H4P4|1236}}</ref> | |||
**In other words: the cortex may "spill" into the surrounding fat. | |||
====Medulla==== | ====Medulla==== | ||
| Line 29: | Line 38: | ||
Produce ''NED'': norepinephrine, epinephrine, dopamine. | Produce ''NED'': norepinephrine, epinephrine, dopamine. | ||
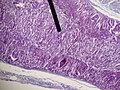
=====Images===== | |||
<gallery> | |||
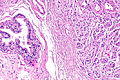
Image:Adrenal_gland_(medulla).JPG | Adrenal medulla. (WC) | |||
Image:Adrenal_cortical_carcinoma_-_low_mag.jpg | Adrenal cortex & medulla (right of image), and tumour (left of image). (WC/Nephron) | |||
</gallery> | |||
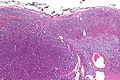
<gallery> | |||
Image:Adrenal rest - epididymis -- low mag.jpg | Adrenal rest - low mag. (WC/Nephron) | |||
Image:Adrenal rest - epididymis -- intermed mag.jpg | Adrenal rest - intermed. mag. (WC/Nephron) | |||
Image:Adrenal rest - epididymis -- high mag.jpg | Adrenal rest - high mag. (WC/Nephron) | |||
</gallery> | |||
=====www===== | |||
*[http://www.webpathology.com/image.asp?case=78&n=5 Adrenal medulla (webpathology.com)]. | |||
===IHC=== | |||
Adrenal cortex:<ref name=pmid18579979>{{Cite journal | last1 = De Padua | first1 = M. | last2 = Rajagopal | first2 = V. | title = Myxoid adrenal adenoma with focal pseudoglandular pattern. | journal = Indian J Med Sci | volume = 62 | issue = 5 | pages = 199-203 | month = May | year = 2008 | doi = | PMID = 18579979 }}</ref> | |||
*Chromogranin A -ve. | |||
*Synaptophysin +ve. | |||
*Alpha-inhibin +ve. | |||
*Vimentin +ve. | |||
*Melan A +ve. | |||
*AE1/AE3 -ve. | |||
*RCC -ve (0 +ve of 63 cases<ref name=pmid21490444>{{Cite journal | last1 = Sangoi | first1 = AR. | last2 = Fujiwara | first2 = M. | last3 = West | first3 = RB. | last4 = Montgomery | first4 = KD. | last5 = Bonventre | first5 = JV. | last6 = Higgins | first6 = JP. | last7 = Rouse | first7 = RV. | last8 = Gokden | first8 = N. | last9 = McKenney | first9 = JK. | title = Immunohistochemical distinction of primary adrenal cortical lesions from metastatic clear cell renal cell carcinoma: a study of 248 cases. | journal = Am J Surg Pathol | volume = 35 | issue = 5 | pages = 678-86 | month = May | year = 2011 | doi = 10.1097/PAS.0b013e3182152629 | PMID = 21490444 }}</ref>). | |||
*EMA -ve (0 +ve of 63 cases<ref name=pmid21490444/>). | |||
A panel that may be useful for [[adrenal cortical adenoma|adenoma]] versus [[adrenal cortical carcinoma|carcinoma]]:<ref name=pmid26317117>{{Cite journal | last1 = Kovach | first1 = AE. | last2 = Nucera | first2 = C. | last3 = Lam | first3 = QT. | last4 = Nguyen | first4 = A. | last5 = Dias-Santagata | first5 = D. | last6 = Sadow | first6 = PM. | title = Genomic and immunohistochemical analysis in human adrenal cortical neoplasia reveal beta-catenin mutations as potential prognostic biomarker. | journal = Discoveries (Craiova) | volume = 3 | issue = 2 | pages = | month = | year = | doi = 10.15190/d.2015.32 | PMID = 26317117 }} | |||
</ref><ref name=pmid11196463>{{Cite journal | last1 = Arola | first1 = J. | last2 = Salmenkivi | first2 = K. | last3 = Liu | first3 = J. | last4 = Kahri | first4 = AI. | last5 = Heikkilä | first5 = P. | title = p53 and Ki67 in adrenocortical tumors. | journal = Endocr Res | volume = 26 | issue = 4 | pages = 861-5 | month = Nov | year = 2000 | doi = | PMID = 11196463 }}</ref> | |||
*Beta-catenin, p53, reticulin, inhibin, melan A, Ki-67. | |||
==Clinical== | ==Clinical== | ||
| Line 39: | Line 77: | ||
The section covers non-neoplastic pathologies of the adrenal gland. These uncommonly come to the pathologist. | The section covers non-neoplastic pathologies of the adrenal gland. These uncommonly come to the pathologist. | ||
*Adrenal incidentalomas<ref>{{Cite journal | last1 = Aljabri | first1 = KS. | last2 = Bokhari | first2 = SA. | last3 = Alkeraithi | first3 = M. | title = Adrenal hemangioma in a 19-year-old female. | journal = Ann Saudi Med | volume = 31 | issue = 4 | pages = 421-3 | month = | year = | doi = 10.4103/0256-4947.76411 | PMID = 21293064 }}</ref> | |||
**Adrenal tumors | |||
**Greater than 1 cm | |||
**Identified on imaging performed for other indications | |||
*Found in up to 10% of patients undergoing abdominal imaging. | |||
*Management problematic | |||
** Guidelines incorporate lesion size, functional status and imaging features. | |||
**Resection is generally advocated for | |||
***Functioning lesions. | |||
***Radiographic features suggestive of malignancy. | |||
***Growth during observation. | |||
==Stress response== | ==Stress response== | ||
*In fetuses - fat content increases due to stress<ref name=pmid964978>{{cite journal |author=Becker MJ, Becker AE |title=Fat distribution in the adrenal cortex as an indication of the mode of intrauterine death |journal=Hum. Pathol. |volume=7 |issue=5 |pages=495–504 |year=1976 |month=September |pmid=964978 |doi= |url=}}</ref> -- see: ''[[Fetal_autopsy#Adrenal_fetal_fat_pattern]]''. | *In fetuses - fat content increases due to stress<ref name=pmid964978>{{cite journal |author=Becker MJ, Becker AE |title=Fat distribution in the adrenal cortex as an indication of the mode of intrauterine death |journal=Hum. Pathol. |volume=7 |issue=5 |pages=495–504 |year=1976 |month=September |pmid=964978 |doi= |url=}}</ref> -- see: ''[[Fetal_autopsy#Adrenal_fetal_fat_pattern]]''. | ||
| Line 44: | Line 93: | ||
==Spironolactone bodies== | ==Spironolactone bodies== | ||
{{Main|Spironolactone bodies}} | |||
==Hemorrhagic adrenalitis== | ==Hemorrhagic adrenalitis== | ||
*[[AKA]] ''Waterhouse-Friderichsen syndrome''. | |||
===General=== | ===General=== | ||
*Classically thought to be only due to ''Neisseria meningitidis''; however, more recently also associated with ''Staphylococcus aureus'',<ref name=pmid16177250>{{cite journal |author=Adem PV, Montgomery CP, Husain AN, ''et al.'' |title=Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children |journal=N. Engl. J. Med. |volume=353 |issue=12 |pages=1245–51 |year=2005 |month=September |pmid=16177250 |doi=10.1056/NEJMoa044194 |url=}}</ref> and ''Streptococcus pneumoniae''.<ref name=pmid14747454>{{cite journal |author=Hamilton D, Harris MD, Foweraker J, Gresham GA |title=Waterhouse-Friderichsen syndrome as a result of non-meningococcal infection |journal=J. Clin. Pathol. |volume=57 |issue=2 |pages=208–9 |year=2004 |month=February |pmid=14747454 |pmc=1770213 |doi= |url=}}</ref> | |||
*Classically thought to be only due to ''Neisseria meningitidis''; however, more recently also associated with '' | |||
===Gross=== | ===Gross=== | ||
| Line 70: | Line 112: | ||
Image: [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770213/figure/f1/ Haemorrhage in adrenal (nih.gov)]. | Image: [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770213/figure/f1/ Haemorrhage in adrenal (nih.gov)]. | ||
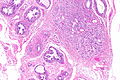
<gallery> | |||
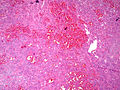
Image:Adrenal WaterhouseFriderichse EColiSepsis LP PA.JPG|Adrenal hemorrhage -low power - E. coli sepsis (SKB) | |||
Image:Adrenal WaterhouseFriderichse EColiSepsis MP PA.JPG|thumb|Adrenal hemorrhage - medium power - E. coli sepsis (SKB) | |||
</gallery> | |||
==Adrenal cytomegaly== | ==Adrenal cytomegaly== | ||
| Line 114: | Line 161: | ||
=Benign neoplasms= | =Benign neoplasms= | ||
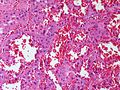
==Adrenal hemangioma== | |||
Radiographic incidentalomas but may be large and calcified raising a radiographic ddx of adrenal cortical carcinoma. | |||
*Rare. | |||
*40 and 70 years. | |||
*2:1 female-to-male ratio | |||
<gallery> | |||
Image:Adrenal Hemangioma LP CTR.jpg|Adrenal hemangioma - low power (SKB) | |||
Image:Adrenal Hemangioma MP CTR.jpg|Adrenal hemangioma - medium power (SKB) | |||
</gallery> | |||
==Adrenal cortical adenoma== | |||
{{Main|Adrenal cortical adenoma}} | |||
==Pheochromocytoma== | |||
{{Main|Pheochromocytoma}} | |||
==Adrenal ganglioneuroma== | |||
{{Main|Ganglioneuroma}} | |||
===General=== | ===General=== | ||
* | *May be retroperitoneal. | ||
*Multiple ganglioneuromas may be due to [[multiple endocrine neoplasia IIb]]. | |||
===Gross=== | |||
* | *Solid. | ||
* | *White. | ||
* | *Firm. | ||
* | *Well-circumscribed. | ||
*May be nodular. | |||
* | |||
DDx (gross): | |||
*[[Leiomyoma]]. | |||
* | |||
Images: | Images: | ||
*[http://commons.wikimedia.org/wiki/File: | *[http://commons.wikimedia.org/wiki/File:Adrenal_ganglioneuroma_02.JPG Adrenal ganglioneuroma (WC)]. | ||
*[http:// | *[http://www.webpathology.com/image.asp?n=2&Case=84 Ganglioneuroma (webpathology.com)]. | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
| Line 225: | Line 208: | ||
Images: | Images: | ||
*[http://commons.wikimedia.org/wiki/File:Ganglion_high_mag.jpg Ganglion - benign (WC)]. | *[http://commons.wikimedia.org/wiki/File:Ganglion_high_mag.jpg Ganglion - benign (WC)]. | ||
==Adrenal myelolipoma== | ==Adrenal myelolipoma== | ||
{{Main|Adrenal myelolipoma}} | |||
==Adenomatoid tumour== | ==Adenomatoid tumour== | ||
| Line 263: | Line 219: | ||
*[[AKA]] ''adrenal cortical carcinoma''. | *[[AKA]] ''adrenal cortical carcinoma''. | ||
*Abbreviated ''ACC''. | *Abbreviated ''ACC''. | ||
{{Main|Adrenocortical carcinoma}} | |||
==Neuroblastoma== | ==Neuroblastoma== | ||
{{Main|Neuroblastoma}} | |||
=See also= | =See also= | ||
Latest revision as of 18:21, 6 March 2018
Adrenal gland is a little organ that hangs-out above the kidney. Pathologists rarely see it. It uncommonly is affected by tumours.
Anatomy & histology
- Adrenal cortical rest redirects here.
Anatomy
- Cortex.
- Medulla.
Note:
- Adrenal tissue may be associated with gonads or between gonads and adrenal gland proper.[1]
Microscopic
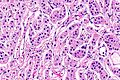
It is composed of a cortex and a medulla.
Cortex
It has three layers - mnemonic: GFR (from superficial to deep):
- Zona glomerulosa - salt (e.g. aldosterone).
- Eosinophilic cytoplasm. (???)
- Layer normally discontinuous.
- Zona fasciculata - sugar (e.g. cortisol).
- Clear cytoplasm - key feature.
- Largest part of the cortex ~ 70%.
- Cells in cords/nests. (???)
- Zona reticularis - steroid (e.g. dehydroepiandrosterone).
- Marked eosinophilia of cytoplasm - key feature.
- Granular/reticular cytoplasm.
Note:
- Normal cortex may not be completely encapsulated, i.e. the adrenal capsule may have defects.[2]
- In other words: the cortex may "spill" into the surrounding fat.
Medulla
It consists of two cell types:[3]
- Chromaffin cells.
- Arise of neural crest.
- Sustentacular cells (supporting cells).
Produce NED: norepinephrine, epinephrine, dopamine.
Images
www
IHC
Adrenal cortex:[4]
- Chromogranin A -ve.
- Synaptophysin +ve.
- Alpha-inhibin +ve.
- Vimentin +ve.
- Melan A +ve.
- AE1/AE3 -ve.
- RCC -ve (0 +ve of 63 cases[5]).
- EMA -ve (0 +ve of 63 cases[5]).
A panel that may be useful for adenoma versus carcinoma:[6][7]
- Beta-catenin, p53, reticulin, inhibin, melan A, Ki-67.
Clinical
Patients getting a bilateral adrenalectomy get pre-treatment with steroids.[8]
Adrenal insufficiency is an immediate danger post-op.[9]
Benign
The section covers non-neoplastic pathologies of the adrenal gland. These uncommonly come to the pathologist.
- Adrenal incidentalomas[10]
- Adrenal tumors
- Greater than 1 cm
- Identified on imaging performed for other indications
- Found in up to 10% of patients undergoing abdominal imaging.
- Management problematic
- Guidelines incorporate lesion size, functional status and imaging features.
- Resection is generally advocated for
- Functioning lesions.
- Radiographic features suggestive of malignancy.
- Growth during observation.
Stress response
- In fetuses - fat content increases due to stress[11] -- see: Fetal_autopsy#Adrenal_fetal_fat_pattern.
- In newborns/children/adults - fat content decreases due to stress.
Spironolactone bodies
Hemorrhagic adrenalitis
- AKA Waterhouse-Friderichsen syndrome.
General
- Classically thought to be only due to Neisseria meningitidis; however, more recently also associated with Staphylococcus aureus,[12] and Streptococcus pneumoniae.[13]
Gross
Features:
- Massive haemorrhage within the substance of the adrenal gland.
DDx (autopsy):
- Post-mortem changes.
Microscopic
Features:
- Massive haemorrhage within the substance of the adrenal gland.
Image: Haemorrhage in adrenal (nih.gov).
Adrenal cytomegaly
General
May be associated with:[14]
- Beckwith-Wiedemann syndrome.
- Prematurity.
- Rh-incompatibility.[15]
Microscopic
Features:
- Large cells in the adrenal cortex.[15]
Addison disease
General
- Chronic adrenocortical insufficiency.
Clinical:
- Brown skin - due POMC (a precursor of ACTH and melanocyte stimulating hormone (MSH)).[16]
- POMC presence implies the pituitary gland intact.
- Hypotension.
- Nausea and vomiting.
DDx:[17]
- Autoimmune.
- Tuberculosis.
- AIDS.
- Malignancy.
Notes:
- Secondary adrenocortical insufficiency (due to pituitary pathology):[18]
- No hyperpigmentation (as no POMC).
- Aldosterone usu. normal.
Microscopic
Features:[16]
- Atrophy adrenal cortex - specifically zona fasciculata and zona reticularis.
Notes:
- There is preservation of zona glomerulosa and medulla.
Benign neoplasms
Adrenal hemangioma
Radiographic incidentalomas but may be large and calcified raising a radiographic ddx of adrenal cortical carcinoma.
- Rare.
- 40 and 70 years.
- 2:1 female-to-male ratio
Adrenal cortical adenoma
Pheochromocytoma
Adrenal ganglioneuroma
General
- May be retroperitoneal.
- Multiple ganglioneuromas may be due to multiple endocrine neoplasia IIb.
Gross
- Solid.
- White.
- Firm.
- Well-circumscribed.
- May be nodular.
DDx (gross):
Images:
Microscopic
Features:
- Ganglion cells - key feature.
- Large cells with large nucleus.
- Prominent nucleolus.
- Large cells with large nucleus.
- Disordered fibrinous material.
Images:
Adrenal myelolipoma
Adenomatoid tumour
See: Adenomatoid tumours (uterine tumours).
Malignant neoplasms
Adrenocortical carcinoma
- AKA adrenal cortical carcinoma.
- Abbreviated ACC.
Neuroblastoma
See also
References
- ↑ Barwick, TD.; Malhotra, A.; Webb, JA.; Savage, MO.; Reznek, RH. (Sep 2005). "Embryology of the adrenal glands and its relevance to diagnostic imaging.". Clin Radiol 60 (9): 953-9. doi:10.1016/j.crad.2005.04.006. PMID 16124976.
- ↑ Mills, Stacey E. (2012). Histology for Pathologists (4th ed.). Lippincott Williams & Wilkins. pp. 1236. ISBN 978-1451113037.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1159. ISBN 978-1416031215.
- ↑ De Padua, M.; Rajagopal, V. (May 2008). "Myxoid adrenal adenoma with focal pseudoglandular pattern.". Indian J Med Sci 62 (5): 199-203. PMID 18579979.
- ↑ 5.0 5.1 Sangoi, AR.; Fujiwara, M.; West, RB.; Montgomery, KD.; Bonventre, JV.; Higgins, JP.; Rouse, RV.; Gokden, N. et al. (May 2011). "Immunohistochemical distinction of primary adrenal cortical lesions from metastatic clear cell renal cell carcinoma: a study of 248 cases.". Am J Surg Pathol 35 (5): 678-86. doi:10.1097/PAS.0b013e3182152629. PMID 21490444.
- ↑ Kovach, AE.; Nucera, C.; Lam, QT.; Nguyen, A.; Dias-Santagata, D.; Sadow, PM.. "Genomic and immunohistochemical analysis in human adrenal cortical neoplasia reveal beta-catenin mutations as potential prognostic biomarker.". Discoveries (Craiova) 3 (2). doi:10.15190/d.2015.32. PMID 26317117.
- ↑ Arola, J.; Salmenkivi, K.; Liu, J.; Kahri, AI.; Heikkilä, P. (Nov 2000). "p53 and Ki67 in adrenocortical tumors.". Endocr Res 26 (4): 861-5. PMID 11196463.
- ↑ URL: http://www3.interscience.wiley.com/cgi-bin/fulltext/119909358/PDFSTART. Accessed on: 21 August 2010.
- ↑ URL: http://ats.ctsnetjournals.org/cgi/content/full/62/5/1516. Accessed on: 21 August 2010.
- ↑ Aljabri, KS.; Bokhari, SA.; Alkeraithi, M.. "Adrenal hemangioma in a 19-year-old female.". Ann Saudi Med 31 (4): 421-3. doi:10.4103/0256-4947.76411. PMID 21293064.
- ↑ Becker MJ, Becker AE (September 1976). "Fat distribution in the adrenal cortex as an indication of the mode of intrauterine death". Hum. Pathol. 7 (5): 495–504. PMID 964978.
- ↑ Adem PV, Montgomery CP, Husain AN, et al. (September 2005). "Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children". N. Engl. J. Med. 353 (12): 1245–51. doi:10.1056/NEJMoa044194. PMID 16177250.
- ↑ Hamilton D, Harris MD, Foweraker J, Gresham GA (February 2004). "Waterhouse-Friderichsen syndrome as a result of non-meningococcal infection". J. Clin. Pathol. 57 (2): 208–9. PMC 1770213. PMID 14747454. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770213/.
- ↑ URL: http://www.humpath.com/?adrenal-cytomegaly. Accessed on: 3 January 2012.
- ↑ 15.0 15.1 Aterman, K.; Kerenyi, N.; Lee, M. (1972). "Adrenal cytomegaly.". Virchows Arch A Pathol Pathol Anat 355 (2): 105-22. PMID 4336262.
- ↑ 16.0 16.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1157. ISBN 978-1416031215.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1155. ISBN 978-1416031215.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 585. ISBN 978-1416054542.